My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.19 n.58 Murcia Apr. 2020 Epub May 18, 2020
https://dx.doi.org/eglobal.384261
Originals
Sexual partnership between people living with HIV: managing serological diferences
1Ribeirão Preto College of Nursing of the University of São Paulo, Brazil.
2Federal University of Piaui, Brazil.
Objective
To analyze whether there are differences between socio-demographic, clinical and affective-sexual characteristics in the different sexual partnerships between people living with HIV/AIDS.
Methods
This is a cross-sectional study carried out in a care service specialized in the treatment of people with Human Immunodeficiency Virus, with 173 participants. Data were collected through interviews with a questionnaire built for the study.
Results
Statistical evidences were verified between the serology of the partner and the sex, marital status, child, number of children. The serology of the sexual partner also presented scientific evidence among the type variables of partnership, use of the male condom, insertive vaginal sex, dissemination of the HIV diagnosis to the sexual partnership and the importance of spreading HIV to the partner.
Conclusion
The serology of the partner was influenced by sociodemographic and affective-sexual variables.
Key words: HIV; Acquired Immunodeficiency Syndrome; Patient Assistance; Sexual behavior
INTRODUCTION
Although HIV/AIDS remains an incurable disease, scientific advances in drug treatment and diagnostic resources have made it possible to reduce morbidity and mortality and increase the life expectancy of people infected with the virus. Treatment with antiretrovirals has attenuated the process of illness, modifying the identity of AIDS that has come to be considered as a chronic condition1 2.
All this context leads to the emergence of a conjugal relationship between people with HIV in whom both are infected by the virus, called seroconcordant, or in which only one of them is infected serodifferent couples. Despite the change in the fight against HIV/AIDS, from a lethal disease to a controlled chronicity, this situation is still a major challenge for health professionals, regarding information that involves this problem3 4
The infected sexual partners face issues ranging from the risk of HIV transmission through sexual intercourse, stigma and even the administration of the serological difference, with respect to the reproductive decision3.
It is pointed up concerns about other dimensions also affected by this disease, such as marital settings of discordant couples and prevention measures adopted by them. The objective was to analyze if there are differences between the sociodemographic, clinical and affective-sexual characteristics in the different sexual partnerships between people living with HIV/AIDS (PLHA).
METHODS
Cross-sectional study, developed at a specialized care service (SAE) of an Integrated Health Center in the State of Piauí, in the northeast region of Brazill.
The unit studied has a structure for ambulatory care of several specialties. The service has a team composed of three infectologists, two nurses and two nursing technicians, to better organize the flow of care, and is linked to the single health system (SUS), which is the health system in force in Brazil, with universal and free access. During the year 2017, 216 patients with viral hepatitis and 996 with HIV/AIDS were treated in the center4
For the definition of the sample we used a sample calculation for finite populations adopting sample error of 0.08 and confidence level of 95.0%, resulting in a sample of 173 users, from a population of 715 people. The inclusion criteria of the study were: individuals of both sexes, with age greater than or equal to 18 years; who was in a fixed or casual relationship in the last 30 days, with the result of an HIV serological test, whether or not the syndrome developed; being at the SAE at the time of data collection.
Exclusion criteria were: being pregnant and deprived of liberty, due to the inherent specificities of the clinical management of these populations and the organization of the local health care network. Also excluded were those who gained access to medication by the Program, but with follow-up in private service.
The recruitment of the participants was as they appeared in the service for care, and occurred in a reserved place, before or after consultations with infectologists. The data were collected through an interview, from November 2016 to March 2017, with the application of a questionnaire with possibilities of dichotomous or multiple responses.
The data were obtained through a semi-structured questionnaire, derived from a macro project titled "Risk management of HIV transmission among sexual partners of people living with HIV/AIDS", which was submitted to theoretical face validation and content examination, by two nurse researchers with expertise in the subject, and a psychologist with experience in the assistance and research of serodiscordant couples who analyzed the comprehension and relevance of the items, clarity of the essay, presence of ambiguities and study objectives.
Sociodemographic, clinical variables related to the stage of HIV infection, variables of the affective-sexual life and related to the offer and actions of the health service offered by the professionals were analyzed.
For the characterization of the study population, descriptive analyzes were made through univariate tests. The data were analyzed using the Software Statistical Package for the Social Sciences version 20.0. and the study met national and international standards of research ethics involving human subjects.
RESULTS
Regarding sociodemographic and clinical variables and their association with the serology of the partner, it was identified that the serodiscordant sexual partnerships were mostly male 55 (31.8%), young adults with ages ranging from 18 to 39 years 48 (27.7%), mostly from Teresina 47 (27.2%). Regarding the level of schooling, 28 (16.2%) of the serodiscordant sexual partnerships completed high school, 39 (22.5%) were brown, 37 (21.45), the majority had children 37 (21.4% %), with a monthly income of up to 3 wages 46 (27.9%), with a number of people in the household that varied from 1 to 2 people 48 (27.7%).
Regarding the clinical variables, serodiscordant sexual partners had a predominance of CD4 cell counts above 500 cells/mm³ 49 (28.3%), with undetectable viral load 57 (32.9%) (Table 1).
Table 1. Socio-demographic and clinical variables of PLHA according to the serology of the sexual partnership. Teresina (PI), Brazil, 2018 (n=173)

There was statistical association between partner's serology (serodiscordant/soroconcordante/unknown) and socio-demographic variables: sex (p = 0.051), Civil status (p> 0.001), children (p> 0.001), number of children (p = 0.005) (Table 1).
As for the affective-sexual variables and their association with the partner's serology, 35 (20.2%) of the serodiscordant couples were heterosexual, 62 (35.8%) established a relationship with fixed sexual partners. Regarding the use of male condoms, 80 (46.2%) reported consistent use, of which 37 (21.4%) were serodiscordant and 19 (11.0%) were unknown. Regarding the co-infection of another STI, syphilis was the most prevalent 42 (24.3%) among the individuals studied, of which 12 (6.9%) occurred among people with HIV who reported having a serodiscordant sexual partnership with HIV.
In analyzing sexual practices, we can see a confirmation of the gender roles identified in our society, a clear division of vaginal sex between heterosexual women and anal sex among men who have sex with men (MSM). Regarding the use of alcohol in sexual intercourse between sexual partners, 36 (20.8%) reported never doing this practice and 32 (18.5%) reported having performed a few times. The use of other drugs during sexual intercourse was reported by 8 (4.6%) of the interviewees.
The serological status of seropositivity to HIV occurred in 53 (30.6%) of the serodiscordant couples, 20 (11.6%) of the individuals reported not to reveal their seropositivity, 46 (26.6%) considered it important to disclose HIV for the sexual partnership (Table 2).
Table 2. Sexual-affective variables of PLHA according to the serology of the sexual partnership. Teresina (PI), Brazil, 2018 (n=173)
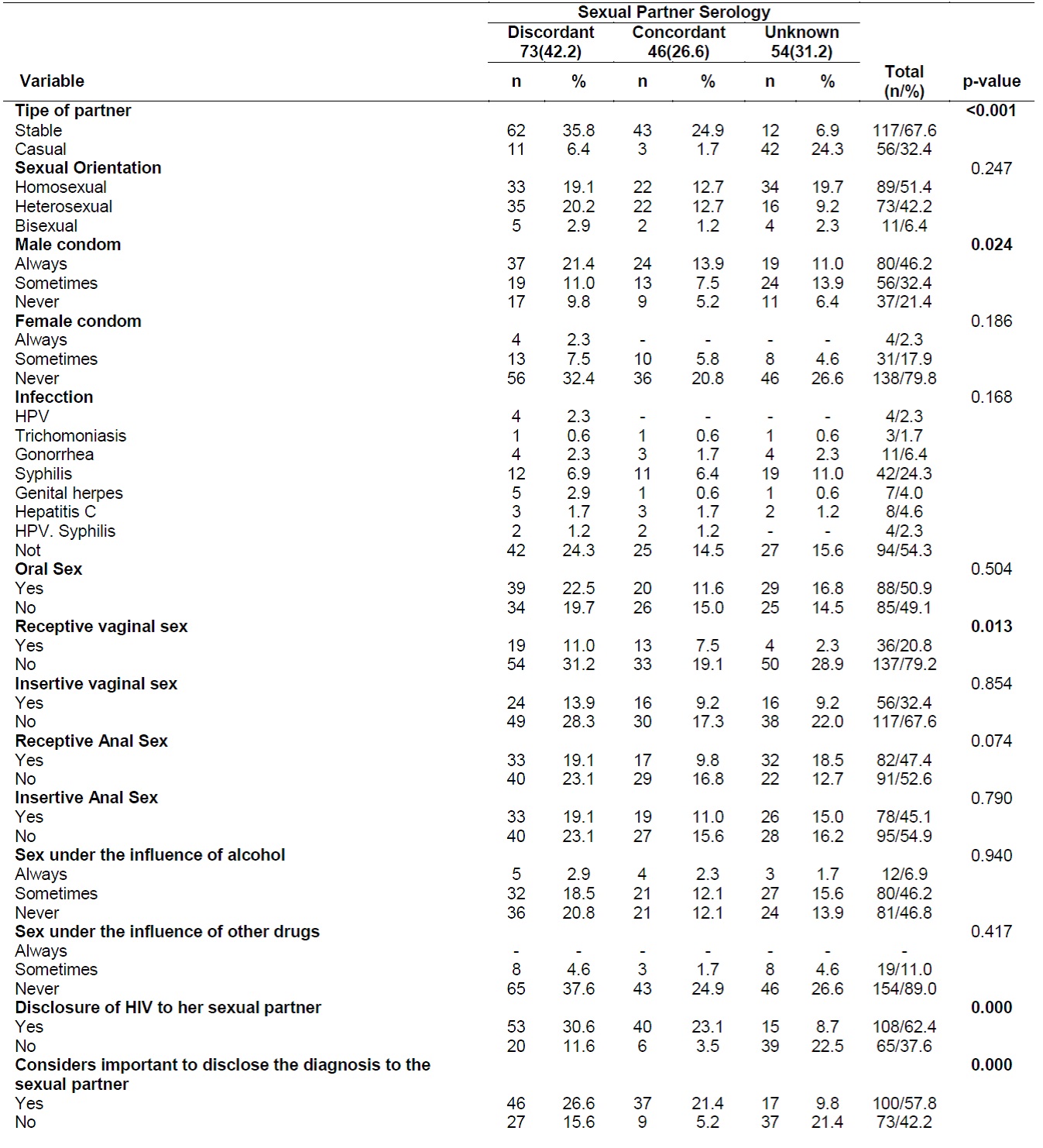
A sorologia do parceiro sexual (sorodiscordante) foi associada com as variáveis: tipo de parceria (p<0,001), uso do preservativo masculino (p=0,024), prática sexual vaginal insertivo (p=0,013), divulgação do diagnóstico do HIV para a parceria sexual (p<0,001) e considera importante a divulgação do HIV para o parceiro (p<0,001) (Table 2).
DISCUSSION
In this study, the prevalence of men living with HIV / AIDS was higher, as observed in other studies, which coincides with the epidemiological profile of HIV/AIDS infection in Brazil, which reinforces the importance of reaching adult and young men so that specific interventions and care can be developed5 6 7 8 9.
In this study, the establishment of sexual partnerships among young adults, with incomes of up to three wages and basic and average schooling, corroborates a study carried out among couples living in the context of HIV/AIDS recruited in 14 European countries. In the present study, there was a predominance of brown ethnicity, which can be explained by the predominance of this ethnic group over all others in Brazil, as a result of the strong miscegenation5 10 11
As for socioeconomic conditions, the authors point out that the management of the risk of sexual transmission of HIV among sexual partners and the choice of a prevention strategy are particularly influenced by economically, socially, politically and culturally disadvantaged positions, limiting prevention behavior and ability to make decisions about safe sex practices5 6.
With regard to undetectable viral load, viral suppression sustained through antiretroviral therapy reduces the risk of sexual transmission of HIV, expanding the possibilities of prevention. Similarly, other variables were also listed in the literature as decisive in HIV transmission, such as the impact of age of the infected person, type and frequency of sexual activity, circumcision, presence of other sexually transmitted infections, use of barrier contraception methods, host genetic background, presence of mutation in HIV co-receptors, variability in histocompatibility antigens, and Killers cell immunoglobulin-like receptors10 12 13.
Regarding the serology of the partner, in the present study, the majority are serodiscordant couples and a significant percentage is unaware of the serology of the partner. When it comes to sexual partnerships, there is concern about the aspects that involve HIV transmission, especially in the acute phase of infection in which the greatest chance of transmission occurs. In fixed sex partnerships, negotiating condom use is an obstacle for such couples, since the failure to use condoms in many relationships is characterized as a sign of confidence14 15.
Regarding the affective-sexual characteristics of the present study, the majority of people living with HIV/AIDS are in a fixed partnership, married, stable union or living with the partner. Authors point out that transmission occurs mainly among couples in stable relationships since this type of relationship favors the inconsistent use of the condom5 16.
In the present study, a significant percentage of couples living in the context of HIV are MSM, with serology discordant to HIV. Dealing with different expressions of sexuality has been a major challenge for society and health services, still very supported by a biomedical and heterosexist model.
Regarding sexual orientation, MSM present distinct vulnerabilities to HIV, which may be related to both sexual attitudes and behaviors as well as the incipient strategies of the health services in proposing recruitment and qualified assistance to this profile of sexual partnerships10.
However, the literature points out the importance of the implementation of combined strategies, articulating primarily the use of condoms in all sexual relations linked to the introduction of early antiretroviral therapies (HAART), favoring the reduction of blood plasma viral load, regardless of the presence of viral load undetectable17 18.
Consistent use of condoms in all sexual relationships is still not a commonly performed practice among a significant number of couples, especially among discordant sexual partnerships, thus demonstrating the need to implement improvements in preventive practices in specialized care services. Inconsistent condom use among PLHA has been identified in studies conducted in other countries. A study conducted in Brazil showed a prevalence of use of 28.7%19 20 21
Condom use consistently among people living in the context of HIV is necessary not only among serodiscordant couples but also among seroconcordant partnerships, since this strategy avoids the process of reinfection of strains already resistant to antiretrovirals, serves as a barrier in the spread of other STIs and even decreases viral load during sexual intercourse21.
Another variable that was highlighted was the inconsistent use of the male condom among individuals with unknown serology. A study conducted in Atlanta, Georgia, identified a situation similar to our study, in which it found that 44% of sexually active people living with HIV infection engage in unhealthy sex partners with HIV/negative status. Participants often did not know the HIV status of their sexual partners22.
Despite the provisions of synergistic strategies for the prevention of HIV transmission and health promotion, the complexity of interpersonal relationships still weakens decision-making by preventive measures, with a major influence on STI vulnerabilities23.
Despite the level of recent evidence that suppression of viral load decreases the risk of HIV transmission, it is important to emphasize the possibility of coinfections, mainly because the presence of another sexually transmitted infection favors an increase in viral load, risk for the spread of this vírus24.
Despite the level of recent evidence that suppression of viral load decreases the risk of HIV transmission, it is important to emphasize the possibility of coinfections, mainly because the presence of another sexually transmitted infection favors an increase in viral load, risk factors for the spread of this virus.
Being HIV-positive and having a sexual partnership presents major challenges such as dealing with emotional factors and stressors linked to the disease, HIV stigma in family and social networks, the impact of this disclosure on interpersonal relationships and lack of support by specialized care services, especially for the HIV negative partner25.
The revelation of the serological status of this HIV infection profoundly influences the daily routine of PLWHA, mainly in terms of mental well-being, social relations, and even adherence to drug therapy. Negative aspects linked to the disclosure of HIV can profoundly affect the quality of lives of these patients, and the feeling involved in such an event can lead to self-isolation25.
Disclosing to a family member can be a different challenge when compared to disclosure to the spouse or sexual partner. Prediction of negative consequences is the main barrier to non-disclosure, mainly because of fear of discrimination and stigmatization, or an unfavorable partner reaction. In this way, the decision about when and for whom to disclose is often described as a complex calculation weighing the perceived risks and benefits. 26
In addition, this strategy is being recognized as an important part in the prevention of this infection, especially for the possibility of support of the partner for adherence to clinical care, medication and the emotional contribution to the infected person, in addition, the couple can still discuss the best strategy to be used. 27 28
The emotional impact of HIV disclosure for serodifferent couples involves high psychic distress. Scientific evidence indicates that the serodiscordant state increases the pressure for a relationship in terms of anxiety, guilt and fears of transmission that may be emotionally exhaustive, there are also barriers to pregnancy. 29
The lack of disclosure of the serological condition for the partner reflects the lack of dialogue between the couple on the prevention method, the emphasis mainly involves fixed sex partnerships with discordant serology, with a greater possibility of risk for HIV transmission.
CONCLUSION
The chronification of HIV / AIDS allowed people living with HIV to establish a variety of partnerships (fixed, casual, seroconcordant, or discordant). There was a predominance of establishment of a relationship with a sexual association that was serodiscordant among individuals who declared themselves to be heterosexual and had a fixed partnership, most of them consistently used the male condom, syphilis was the most present coinfection between these sexual partnerships and the use of alcohol is present in the sexual intercourse. The revelation of the serological situation was performed by a significant percentage of the participants and most consider it important to reveal their current serological condition.
The serology of the sexual partnership presented statistically significant differences between the: type of partnership, use of the male condom, insertive vaginal sex, disclosure of HIV to the partner and considers it important to disclose HIV to the partner.
REFERENCIAS
1. Hancuch K, Baeten J, Ngure K, Celum C, Mugo N, Tindimwebwa E, et al. Safer conception among HIV-1 serodiscordant couples in East Africa: understanding knowledge, attitudes, and experiences, AIDS Care, 2018; 30(8): 973-981. doi: 10.1080/09540121.2018.1437251 [ Links ]
2. Brown, J., Njoroge, B., Akama, E., Breitnauer, B., Leddy, A., Darbes, L.,Mmeje, O. A novel safer conception counseling toolkit for the prevention of HIV: A mixed-methods evaluation in Kisumu, Kenya. AIDS Education and Prevention, 2016; 28 (6): 524-538. doi: 10.1521/aeap.2016.28.6.524 [ Links ]
3. Oliveira LB, Matos MCB, Jesus GJ, Reis RK, Gir E, Araújo TME. Sexual partnerships of people living with the Human Immunodeficiency Virus. Rev Rene. 2017; 18 (6): 825-31. doi: 10.15253/2175-6783.2017000600017 [ Links ]
4. Oliveira LB, Matos MCB, Costa CRB, Jesus GJ, Argolo JGM, Reis RK. Establishment of partnerships in people living with hiv/aids attended in a specialized center: experience report. Sylwan. 2017; 161(7):106-212. http://www.sylwan.ibles.org/syl/index.php/pdf/stream/884Tf/1497309728 [ Links ]
5. Mwakalapuka A, Mwampagatwa I, Bali T, Mwashambwa M, Kibusi S. Emotional and Relationship Dynamics between HIV SeroDiscordance and Concordance Couples: A Narrative Literature Review and Theoretical Framework. ARC J Public Health Community Med. 2017; 2(2): 1-14. https://ecommons.aku.edu/eastafrica_fhs_sonam/146 [ Links ]
6. Atujuna M, Newman PA, Wallace M, Eluhu M, Rubincam C, Brown B, et al. Contexts of vulnerability and the acceptability of new biomedical HIV prevention technologies among key populations in South Africa: A qualitative study. PLoS ONE. 2018; 13(2): e0191251. doi: https://doi.org/10.1371/journal.pone.0191251 [ Links ]
7. Dourado I, MacCarthy S, Reddy M, Calazans G, Gruskin S. Revisitando o uso do preservativo no Brasil. Rev bras epidemiol. 2015 Sep; 18 (Suppl 1): 63-88. doi: http://dx.doi.org/10.1590/1809-4503201500050006 [ Links ]
8. Brasil. Departamento de DST, Aids e Hepatites Virais, Secretaria de Vigilância em Saúde, Ministério da Saúde. Boletim Epidemiológico HIV-AIDS. 2016. [ Links ]
9. Tam VV, Cuong DD, Alfven T, Phuc HD, Chuc NTK, Hoa NP., et al. HIV serodiscordance among married HIV patients initiating antiretroviral therapy in northern Vietnam. AIDS Research and Therapy. 2016; 13(12): 39. doi:https://doi.org/10.1186/s12981-016-0124-9 [ Links ]
10. Rodger AJ, Cambiano V, Bruun T, et al. Sexual Activity Without Condoms and Risk of HIV Transmission in Serodifferent Couples When the HIV-Positive Partner Is Using Suppressive Antiretroviral Therapy. JAMA. 2016; 316(2): 171-181. doi: 10.1001/jama.2016.5148 [ Links ]
11. Dube BNR, Marshall TP, Ryan RP. Predictors of human immunodeficiency virus (HIV) infection in primary care: a systematic review protocol. Systematic Reviews. 2016; 5(3): 158-64. doi: 10.1186/s13643-016-0333-2 [ Links ]
12. Lam CR, Holtz TH, Leelawiwat, W, Mock PA, Chonwattana W, Wimonsate W. et al. Subtypes and Risk Behaviors Among Incident HIV Cases in the Bangkok Men Who Have Sex with Men Cohort Study Thailand, 2006-2014. AIDS Research and Human Retroviruses. 2017; 33(10): 1004-1012. doi: https://doi.org/10.1089/aid.2016.0119 [ Links ]
13. Perry, NS., Wade Taylor, S., Elsesser, S. et al. The Predominant Relationship Between Sexual Environment Characteristics and HIV-Serodiscordant Condomless Anal Sex Among HIV-Positive Men Who Have Sex With Men (MSM). AIDS Behav. 2016; 20(6): 1228-35. doi: https://doi.org/10.1007/s10461-015-1202-z [ Links ]
14. Cremin I, Hallett T. Estimating the range of potential epidemiological impact of pre-exposure prophylaxis: run-away success or run-away failure? AIDS, 2015; 29(6): 733-739. doi: 10.1097/QAD.0000000000000591. [ Links ]
15. Taylor SW. Psaros C, Pantalone DW, Tinsley J, Elsesser AS, Mayer KH. Life-Steps for PrEP adherence: demonstration of a CBT-Based Intervention to Increase Adherence to Preexposure Prophylaxis (PrEP) Medication Among Sexual-Minority Men at High Risk for HIV Acquisition. Cognitive and Behavioral Practice. 2017; 24(1): 38-49. doi: 10.1016/j.cbpra.2016.02.004 [ Links ]
16. Bernier A, Lazar F, Matamba G, Loukid M, Bonifaz C, Diop S., et al. ‘‘Was it a mistake to tell others that you are infected with HIV?": factors associated with regret following HIV disclosure among people living with HIV in five countries (Mali, Morocco, Democratic Republic of the Congo, Ecuador and Romania). Results from a Community-Based Research. AIDS and Behavior. 2015; 19(2): 311-3. doi: 10.1007/s10461-014-0976-8 [ Links ]
17. Afe AJ, Fadero T, Oluokun O. HIV Sero-Discordant Couples in Southwest Nigeria: Prevalence and Associated Risk Factors. Journal of Clinical Research In HIV AIDS And Prevention 2015- 3(2):24-31. doi: 10.14302/issn.2324-7339.jcrhap-18-2236 [ Links ]
18. Suzan-Monti M, Lorente N, Demoulin B, Marcellin F, Pre´au M, Dray-Spira R., et al. Sexual risk behaviour among people living with HIV according to the biomedical risk of transmission: results from the ANRS-VESPA2 survey. Journal of the International AIDS Society. 2016; 19:1: 20095. doi: http://dx.doi.org/10.7448/IAS.19.1.20095 [ Links ]
19. Engedashet E, Alemayehu W, Gezahegn, T. Unprotected sexual practice and associated factors among People Living with HIV at Ante Retroviral Therapy clinics in Debrezeit Town, Ethiopia: a cross sectional study. Reproductive Health 2014, 11:56. doi: https://doi.org/10.1186/1742-4755-11-56 [ Links ]
20. Kilembe W, Wall KM, Mokgoro M, Mwaanga A, Dissen E, Kamusoko M, et al. (2015) Knowledge of HIV Serodiscordance, Transmission, and Prevention among Couples in Durban, South Africa. PLoS ONE 10(4): e0124548. doi: https://doi.org/10.1371/journal.pone.0124548 [ Links ]
21. Reis RK, Melo ES, Gir E. Fatores associados ao uso inconsistente do preservativo entre pessoas vivendo com HIV/Aids. Rev Bras Enferm. 2016; 69(1): 47-53. doi: http://dx.doi.org/10.1590/0034-7167.2016690106i [ Links ]
22. Kalichman SC, Cherry C, Kalichaman MO, Washington C, Grebler T, Hoyt G., et al., Sexual Behaviors and Transmission Risks Among People Living with HIV: Beliefs, Perceptions, and Challenges to Using Treatments as Prevention. Achives of Sexual Behavior. 2016; 45(6): 1421-14. doi: 10.1007/s10508-015-0559-4 [ Links ]
23. Queiroz Artur Acelino Francisco Luz Nunes, Sousa Álvaro Francisco Lopes de, Matos Matheus Costa Brandão, Araújo Telma Maria Evangelista, Reis Renata Karina, Moura Maria Eliete Batista. Knowledge about HIV/AIDS and implications of establishing partnerships among Hornet(r) users. Rev Bras Enferm. 2018; 71 (4): 1949-1955. doi: http://dx.doi.org/10.1590/0034-7167-2017-0409 [ Links ]
24. Zwolinska K, Fleischer-Stepniewska K, Knysz B, Blachowicz O, Piasecki E. Genetic diagnosis of seronegative (HIV-) partner of female patient with AIDS in the context of HIV transmission. HIV & AIDS Review. International Journal of HIV-Related Problems. 2016;15(2):97-100. https://www.termedia.pl/Genetic-diagnosis-of-seronegative-HIV-partner-of-female-patient-with-AIDS-in-the-context-of-HIV-transmission,106,27843,0,1.html [ Links ]
25. Marcellin, F., Suzan-Monti, M., Vilotitch, A. et al. AIDS Behav. Disclosure of HIV Status Beyond Sexual Partners by People Living with HIV in France: A Call for Help? Results from the National Cross-Sectional Survey ANRSVESPA2. AIDS behavior. 2017; 21(1): 196-206. doi: https://doi.org/10.1007/s10461-016-1549-9 [ Links ]
26. Conroy AA, Wong LH. How reliable are self-reports of HIV status disclosure? Evidence from couples in Malawi. Social Science & Medicine. 2015; 144: 28-37. doi: 10.1016/j.socscimed.2015.09.007. [ Links ]
27. Cissé M, Diop S, ABADIE A, Henry E, Bernier A, Fugon L., et al. Factors associated with HIV voluntary disclosure to one's steady sexual partner in mali: results from a community-based study. Journal of Biosocial Science. 2016; 48(1): 51-65. doi: https://doi.org/10.1017/S0021932014000546 [ Links ]
28. Obiri-Yeboah D, Amoako-Sakyi D, Baidoo L, Adu-Oppong A, Rheinlander T. The 'Fears' of disclosing HIV status to sexual partners: a mixed methods study in a counseling setting in Ghana. AIDS Behavior. 2016 Jan;20(1):126-36. doi: 10.1007/s10461-015-1022-1. [ Links ]
29. Cherayi S, Jose JP. The determinants of distress among HIV discordant couples. HIV & AIDS Review. 2015; 14(4): 119-125. doi: 10.1016/j.hivar.2015.05.006 [ Links ]
Received: June 19, 2019; Accepted: February 26, 2020











 text in
text in 


