My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.21 n.65 Murcia Jan. 2022 Epub Mar 28, 2022
https://dx.doi.org/10.6018/eglobal.484571
Originals
Sexually Transmitted Infections in the Riparians Population: prevalence and risk behavior
1 Graduanda en Enfermería, Universidad Federal de Paraíba. João Pessoa, PB, Brasil. bebelamartelleto1@gmail.com
2 Enfermera. Maestra en Enfermería - Programa de Posgraduación en Enfermería (PPGENF) de la Universidad Federal de Paraíba, João Pessoa, PB, Brasil.
3 Enfermera. Doctora en Enfermería. Profesora adjunta del Departamento de Enfermería Clínica de la Universidad Federal de Paraíba, João Pessoa, PB, Brasil.
Introduction:
The riparians population is considered vulnerable to Sexually Transmitted Infections due to restrictions related to access to health, information and education.
Objective:
To analyze the prevalence of self-reported Sexually Transmitted Infections among the riparians population and associated sociodemographic and behavioral factors.
Material and Method:
Cross-sectional, analytical study, conducted with 250 riparians dwellers from João Pessoa, Paraiba state, from June to October 2019. Data were collected through interviews using a structured questionnaire. Logistic regression analysis was performed. The research was approved by the Research Ethics Committee under opinion number 3,340,273.
Results:
The prevalence of Sexually Transmitted Infections was 20.8%. Male ribs (OR=3.27; CI95%:1.74-6.15), who reported sexual intercourse with sex workers (OR=6.54; CI95%:3.05-14.0) and illicit drug use (OR 2.13; CI95%:1.10-4.13) were more likely to develop sexually transmitted infection.
Conclusions
High prevalence of sexually transmitted infections and presence of risk behaviors among riparians. Screening, early diagnosis and health education is essential for discontinuation of the transmission chain.
Keywords: Sexually Transmitted Infections; Vulnerable Populations; Epidemiology; Risk Behavior; Public Health
INTRODUCTION
Sexually Transmitted Infections (STIs) represent an important health problem, both for infected individuals and for health authorities in Brazil and the world, mainly because they are infections that facilitate the transmission of human immunodeficiency virus (HIV)1.
According to PAHO Brazil2 there has not been a decline in STIs cases since 2012 and daily more than 1 million people are contaminated by curable STIs. In general, the number of cases of these infections among individuals in Brazil remains constant, but the sociodemographic and behavioral risk characteristics have changed over time, aspects that favor the permanence of STIs.
Vulnerability and the risk of contamination of STIs are linked to lack and social exclusion. Socioeconomically unfavorable populations are considered vulnerable because they do not have the necessary resources to contain the risks to which they are exposed. Therefore, the low level of education, limited access to health services and the practice of risky sexual behaviors are aspects related to vulnerability to STIs3.
In this context, the riparians populations are framed. These populations are characterized by having their homes located on the banks of rivers and by presenting restrictions related to access to health, information and education4.
In Brazil, the riparians population was recognized as a traditional population by Presidential Decree N 6,040/2007, thus ensuring its valorization, food security, accessible language of information and respect for its socio-environmental and cultural diversity. Most of this population is in the Brazilian Amazon, which survive crafts, fishing and agriculture5.
In the state of Paraiba some of these communities are in the urban area, in subnormal clusters, with houses located on the banks of the main rivers that cut through the cities. They are individuals exposed to river pollution, with inadequate housing conditions, low income and limited access to health services.
In the meantime, riparians populations present risk factors that may contribute to the practice of risky sexual behavior and, consequently, increased vulnerability to STIs acquisition. The initiation of early sexual life, the consumption of alcohol and other drugs, the practice of unsafe sex and the multiplicity of partners are the risk behaviors that favor the prevalence and incidence of these infections, making it challenging to combat STIs6,7.
In May 2016, the World Health Organization considered the Global Health Sector Strategy 2016-2021 on STIs. This strategy includes an increase in evidence-based interventions and services to control and eradicate sexual transmission of infections, which represents one of the public health concerns in 20308.
In the light of the above, this study is justified by the importance of knowing the scenario of riparians populations about STIs, as well as by the scarcity of studies directed to this population. Thus, the study aims to analyze the prevalence of self-reported Sexually Transmitted Infections (STIs) among the riparians population of the municipality of João Pessoa, Paraiba, and sociodemographic and behavioral factors associated with infections.
MATERIALS AND METHODS
This is a cross-sectional, analytical study conducted with the riparians population living in the municipality of João Pessoa, in the state of Paraiba, from June to October 2019.
The study population consisted of people over 18 living in riparians communities. Individuals who had more than one residence, where at least one of them, was not located in the riparians community investigated, were excluded. For the composition of the sample, 11,498 individuals were considered, since it corresponds to the sum of the total number of residents of these communities. For the determination of the sample size, a Confidence Interval (CI) of 95%, a desirable margin of error of 5.4% and an estimated frequency of 26.15% were admitted, referring to the estimate of the STIs obtained by calculating the average points of the intervals of the estimates of the main STIs found in studies9,10. Thus, the number of 250 participants in the sample was obtained.
Data were collected at a structured support site within the riparians community, with the support of the family health team. The riparians dwellers were invited to participate in the study through prior contact made by community health agents (CHA). Eligible individuals were informed about the importance of the study and objectives. Upon acceptance of the participant, an individual and private interview was conducted through a structured questionnaire, validated and adapted from the instrument used in the Knowledge, Attitudes and Practices Survey in the Brazilian Population, including sociodemographic data and risk factors and behaviors for the acquisition of STIs11.
The collected data were entered in a Microsoft Excel spreadsheet and imported into the statistical program SPSS version 20.0 for statistical analysis. The prevalence of STIs, according to the report, was calculated with a 95% confidence interval (95%CI).
The dependent variable of this research was operationalized as follows: "Did you have any sexually transmitted diseases?", with response options such as: (0) No/ (1) Yes. Specify (infection and/or signs and symptoms)". The variables considered independent were: gender (male and female), age (18 to 40 years, > 40 years), schooling (up to eight years of schooling and over 8 years of schooling), marital status (married/sTable union and single/divorced/widowed), monthly income (up to one minimum wage and above one minimum wage), age of first sexual intercourse (≤ 15 years and > 15 years), number of sexual partners in the last 12 months (0 to 1 partner and ≥ 2 partners), condom use in the last sexual intercourse (yes and no), frequency of condom use (always/sometimes and never), sexual intercourse with sex workers (yes and no), use of illicit drugs in life (yes and no), currently smokes (yes and no) and prison history (yes and no).
To investigate the association between sociodemographic and behavioral variables, we used the bivariate analysis of the logistic regression model, generating odds or odds ratio (OR) with 95% CI. Values of p<0.05 were considered significant.
It is emphasized that the ethical precepts that guide the research involving human beings, described and established by Resolution n. 466/2012 of the National Health Council (NHC) were obeyed. All participants signed the Free and Informed Consent Form (TCLE) in two ways. The study was approved by the Research Ethics Committee (CEP) of the Federal University of Paraiba (UFPB) under the number of opinion 3,340,273.
RESULTS
Of the total of 250 riparians interviewed in the study, there was a predominance of female riparians - 170 (68.0%), in the age group between 18 and 39 years - 108 (43.2%), with up to eight years of schooling - 155 (62.0%). Regarding marital status, 160 (64.0%) reported being married or having consensual union and 208 (83.2%) with monthly family income up to 1.5 minimum wage (Minimum wage: R$998.00).
The prevalence of self-reported STIs among individuals was 20.8% (95% CI: 18.2-23.3) which corresponds to 52 riparians who reported the presence of STIs in life. Among the Reported STIs are syphilis, 17 (32.7%), gonorrhea, 15 (28.8%), Human Papilloma Virus (HPV), 9 (17.3%), HIV, 2 (3.8%), herpes, 1 (1.9%), and others, 8 (15.4%). Of the riparians who reported the presence of STIs, the most frequent clinical signs related to the presence of infection were vaginal and/or urethral discharge, 24 (46.2%), and the appearance of blisters in the genital region, 23 (44.2%). Regarding treatment, 48 (92.3%) of the riparians sought treatment for STIs presented, as shown in Table 1.
Table 1: Characteristics related to the presence of STIs in individuals from riparians communities. João Pessoa, PB, Brazil, 2019.

Source: Search Data, 2019.
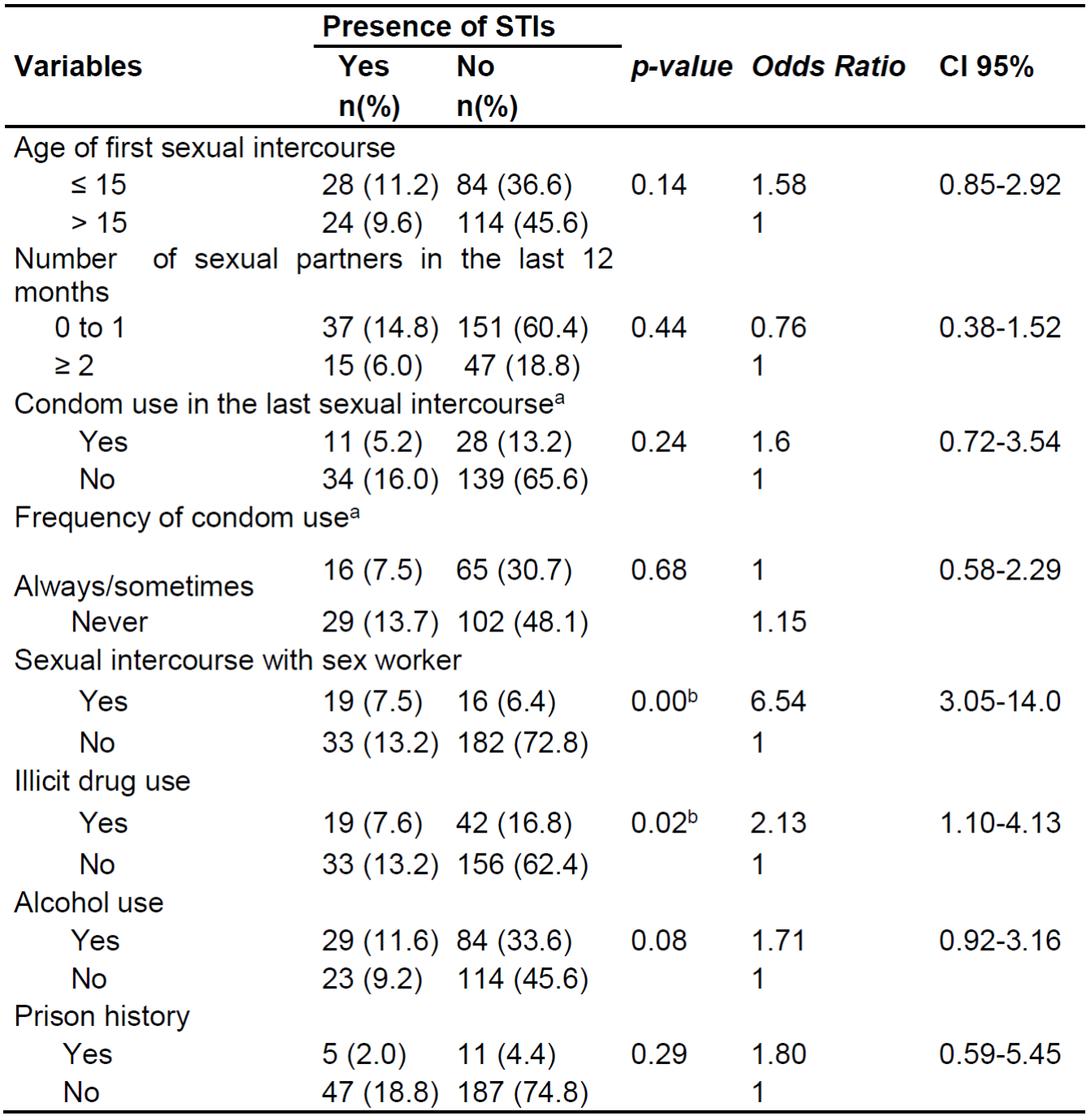
Bivariate analyses of sociodemographic characteristics and the main risk behaviors reported by riparians and their association with the presence of STIs were performed. Regarding the sociodemographic variables (gender, age, education, marital status and income) statistical significance was observed for the variable gender (OR = 3.27; CI 95%:1.74-6.15), according to Table 2.
Table 2: Sociodemographic characteristics associated with the presence of STIs in individuals from riparians communities. João Pessoa, PB, Brazil, 2019.
ª Significant value with p<0,05.
Source: Search Data, 2019.
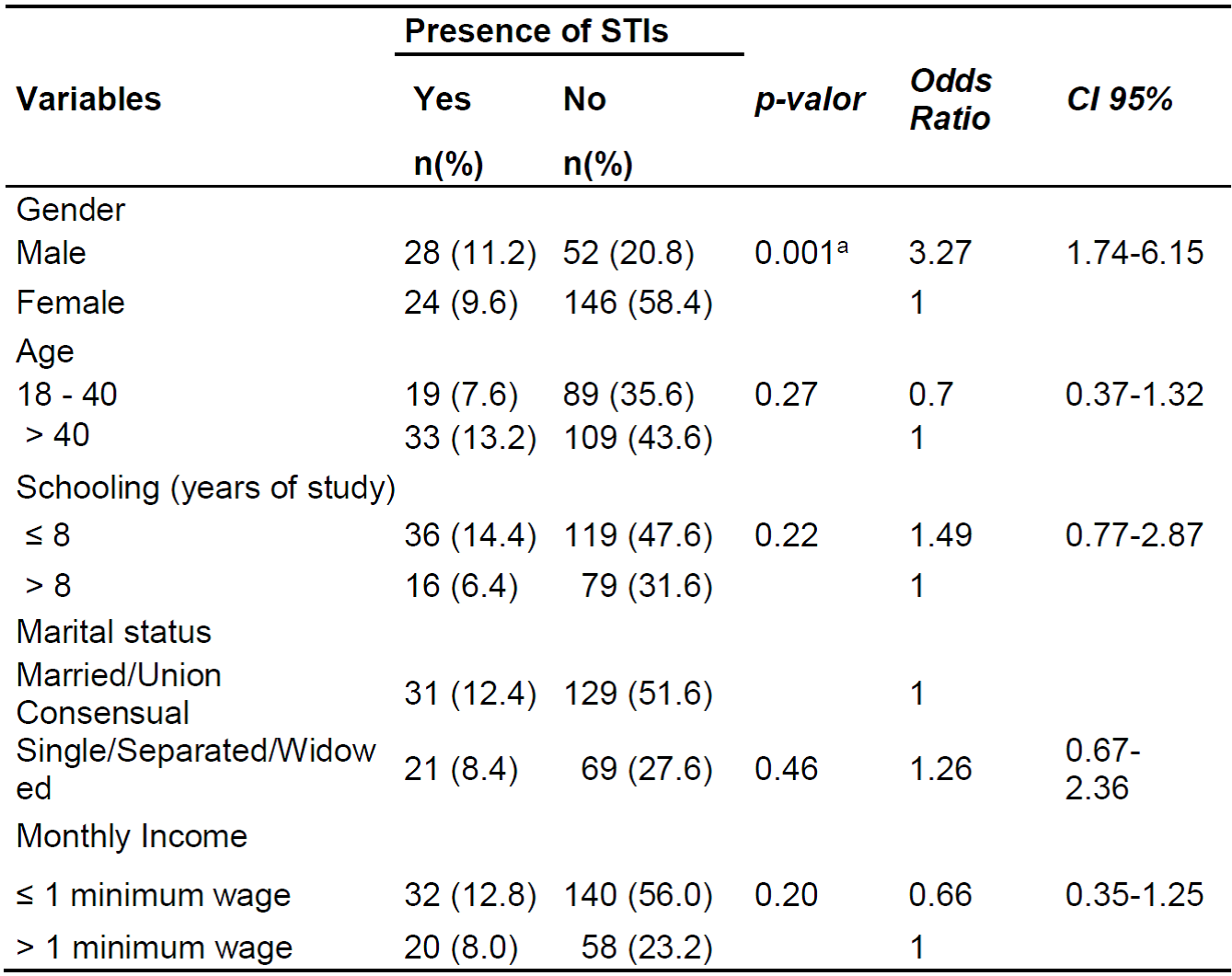
Regarding the main risk behaviors, the variables that presented statistical significance with the presence of STIs were sexual intercourse with sex workers (OR 6.54; CI95%:3.05-14.0) and illicit drug use (OR 2.13; IC95%: 1.10-4.13). Thus, it was observed that the riparians who reported sexual intercourse with a sex worker and who at some point in their lives used illicit drugs are seven and twice as likely to acquire an STI, respectively (Table 3).
DISCUSSION
The riparians communities that live in the urban area, in a space of subnormal clusters, are marked by socioeconomic inequalities and health-related vulnerabilities that favor the risk for the acquisition of STIs. Due to the scarcity of studies related to the theme and the target audience of the study, for comparative analyses will be considered research involving other vulnerable populations.
Regarding the sociodemographic aspects of the riparians investigated, low income and low schooling are observed. A population survey of 492 riparians from the Amazon region obtained similar findings, in which 68.5% reported having up to nine years of schooling. According to this research, this fact is related to the barriers of locomotion found by this population to move to the school environment12. In addition, low schooling is closely related to the high prevalence of STIs, due to the limitation of information on infections and forms of prevention, becoming an important barrier to the promotion of sexual health in riparians areas13.
The study showed a self-reported prevalence of STIs of 20.8% (95% CI: 18.2-23.3). The prevalence found in the study was higher than in a study conducted with 31,639 women from rural West Africa (4.0%; 95% CI: 3.8-4.2%)14. A systematic review study on adult homeless people in the United States showed a prevalence of STIs from 2.1% to 52.5%(15). Among the reported STIs, syphilis was the most frequent infection, 17 (32.7%). Epidemiological data reveal that the prevalence of syphilis, while stabilizing in the general population, presents high prevalence in population segments under greater vulnerability and risk of infection. It is possible that declines in the general population reflect changes that occur in specific sexual networks, such as sexual networks of different-sex couples, while the incidence may be increasing in other sexual networks, such as between Men who have Sex with Men (SWM) and sexual intercourse with sex workers16,17.
Of the riparians who reported the presence of STIs, the most self-reported clinical sign of infection was vaginal and/or urethral discharge, 24 (46.2%), followed by the presence of blisters and wounds. A similar finding was found in a study conducted with indigenous people living in rural and riparians villages in Guatemala that showed that the most frequent symptom of STIs was genital discharge (48.5%)18. The presence of STIs symptoms in vulnerable populations may be related to a lower level of schooling that reflects knowledge and efforts to prevent STIs15, which could be seen in the present study. Moreover, there is evidence that this fact occurs due to the early onset of sexual life, related to a lower knowledge about the forms of transmission of STIs, culminating in unprotected sexual practice19.
The analysis of sociodemographic factors showed that male riparians are three times more likely (OR=3.27; CI 95%:1.74-6.15) of presenting an STIs. Regarding the association of sex with higher chances of acquiring STIs, studies20,21 corroborate this finding. This fact can be justified due to the image of virility associated with the male sex, who believes that the search for the health service for prevention is a demonstration of weakness, which implies low access to primary care services, reinforcing the importance of the National Policy of Men's Health.
Regarding risk behaviors, the analysis showed that riparians who reported sexual intercourse with sex workers are six times more likely (OR 6.54; CI95%:3.05-14.0) to present an STIs. A study22 developed in Brazilian capitals concluded that 61.2% of sex workers would accept the practice of sexual intercourse without a condom for reason, such as remuneration, emotional involvement, alcohol use or other drugs. This result highlights the need to strengthen prevention measures, especially the encouragement of safer sexual behaviors with condom use and awareness of the risk of infection.
The study also showed that riparians who use illicit drugs are more likely (OR 2,13; CI95%: 1.10-4.13) to develop an STIs. Associations between illicit drug use and STIs were also evidenced in other studies23,24. A study23 conducted in the United States with young adults showed an association between these variables (OR: 3.10, 95%CI: 2.77-3.47) and in a study24 conducted with 2,320 Aboriginal individuals living in the Torres Strait Islands, also identified an association between illicit drug use and the prevalence of self-reported STIs (OR: 1.86, 95% CI: 1.24, 2,79).
Most of the time, the use of illicit drugs may be related to the sensations of the neurological effects caused by drugs that decrease the perception of the individual's risk, which can impact the non-use of condoms during sexual intercourse. This result may suggest that the reduction in illicit drug use may have a significant impact on the transmission of STIs25,26.
Limitations of the study are its cross-sectional type, which does not allow inferring a cause-and-effect relationship between the variables. Data related to the prevalence of STIs, and its signs and symptoms were collected through self-report and may be subject to memory bias and measurement error. However, the study provides important data on STIs in riparians populations and the main factors that may be associated with the development and transmissibility of these infections.
CONCLUSIONS
The research provides evidence of a high prevalence of self-reported STIs in the riparians population and that being male, having sex with sex workers and using illicit drugs increase the chances of riparians presenting an STIs.
With this, riparian populations experience situations of vulnerability, such as socioeconomically unfavorable conditions and difficulty in accessing health services that expose them to health-related risks. It is possible to visualize the need for health education practices directed to the sexual health of riparians populations, with a view to reducing risk behaviors and promoting knowledge about the importance of preventing STIs.
It is expected that the findings will contribute to the strengthening of public policy actions aimed at this population group and that strategies for the prevention and screening of STIs be expanded. As well as provide subsidies for future research focusing on the theme of STIs in riparians populations.
REFERENCIAS
1. Brasil. Ministério da Saúde. Boletim Epidemiológico HIV. Brasília (DF): Ministério da Saúde (BR), Departamento de DST, Aids e Hepatites Virais; 2020. Available from: http://www.aids.gov.br/pt-br/pub/2020/boletim-epidemiologico-hivaids-2020. [ Links ]
2. OPAS Brasil. Organização Pan-Americana da Saúde/Organização Mundial de Saúde. Doenças Transmissíveis & Análise de Situação de Saúde. Brasília: OPAS/OMS; 2019. [ Links ]
3. Costa MIF, Rodrigues RR, Teixeira RM, Paula PHA, Luna IT, Pinheiro PNC. Adolescents in situations of poverty: resilience and vulnerabilities to sexually transmitted infections. Rev. Bras. Enferm. [Internet]. 2020 [access 12 nov 2020]; 73(Suppl. 4). Doi: https://doi.org/10.1590/0034-7167-2019-0242 [ Links ]
4. Parmejiani EP, Queiroz ABA, Pinheiro AS, Cordeiro EM, Moura MAV, Paula MBM. Sexual and reproductive health in riverine communities: integrative review. Rev Esc Enferm USP [Internet]. 2021 [access 14 jun 2021]; 55:e03664. Doi: https://doi.org/10.1590/S1980-220X2019033103664 [ Links ]
5. Presidência da República Casa Civil. Decreto nº 6040, de 7 de fevereiro de 2007. Institui a Política Nacional de Desenvolvimento Sustentável dos Povos e Comunidades Tradicionais. Brasil: Casa Civil; 2007. Available from: http://www.planalto.gov.br/ccivil_03/_ato2007-2010/2007/decreto/d6040.htm#:~:text=DECRETO%20N%C2%BA%206.040%2C%20DE%207,que%20lhe%20confere%20o%20art [ Links ]
6. Neves RG, Wendt A, Flores TR, Costa CS, Costa FS, Tovo-Rodrigues, et al. Simultaneidade de comportamentos de risco para infecções sexualmente transmissíveis em adolescentes brasileiros, 2012. Epidemiol. Serv Saúde [Internet]. 2017 [access 14 jun 2021]; 26(3). Doi: https://doi.org/10.5123/S1679-49742017000300003 [ Links ]
7. Graf DD, Mesenburg MA, Fassa AG. Comportamento sexual de risco e fatores associados em universitários de uma cidade do sul do Brasil. Rev Saude Publica [Internet]. 2020 [access 14 jun 2021]; 54(41). Doi: https://doi.org/10.11606/s1518-8787.2020054001709 [ Links ]
8. World Health Organization (WHO). Global health sector strategy on sexually transmitted infections 2016-2021: toward ending STIs. Geneva: World Health Organization; 2016. Available from: https://apps.who.int/iris/bitstream/handle/10665/246296/WHO-RHR-16.09-eng.pdf. [ Links ]
9. Rocha DFNC, Rosa LRC, Silva CA, Oliveira BR., Martins TLS, Martins RMB, et al. Epidemiology of HIV, syphilis, and hepatitis B an0d C among manual cane cutters in low-income regions of Brazil. BMC Infect Dis [Internet]. 2018 [access 25 nov 2020];18(1). Doi: https://doi.org/10.1186/s12879-018-3439-4 [ Links ]
10. Amorim TF, Teles SA, Moraes LC, Matos MA, Carneiro MADS, Nogueira DJ, et al. Symptomatic Sexually Transmitted Infections in Brazil's emerging rural populations. J Assoc Nurses Aids Care [Internet]. 2018 [access 25 nov 2020]; 29(6):942-8. Doi: https://doi.org/10.1016/j.jana.2018.05.004 [ Links ]
11. Brasil. Ministério da Saúde. Pesquisa de conhecimentos, atitudes e práticas na população brasileira. Brasília (DF): Ministério da Saúde (BR), Secretaria de Vigilância em Saúde; 2011. Available from: https://bvsms.saude.gov.br/bvs/publicacoes/pesquisa_conhecimentos_atitudes_praticas_populacao_brasileira.pdf [ Links ]
12. Gama ASM, Fernandes TG, Parente RCP, Secoli SR. Inquérito de saúde em comunidades ribeirinhas do Amazonas, Brasil. Cad Saúde Pública (Online) [Internet]. 2018 [access 0 jul 2020]; 34(2):e00002817. Doi: https://doi.org/10.1590/0102-311x00002817 [ Links ]
13. Pereira AL, Silva LR, Palma LM, Moura LCL, Moura MA. Impacto do grau de escolaridade e idade no diagnóstico tardio de sífilis em gestantes. Femina [Internet]. 2020 [access em 15 jun 2021]; 48(9):563-567. Available from: https://docs.bvsalud.org/biblioref/2020/10/1122585/femina-2020-489-563-567.pdf [ Links ]
14. Zango SH, Lingani M, Valea I, Samadoulougou OS, Bihoun B, Rouamba T, et al. malaria and curable sexually transmited infections in pregnant women: a two-years observational study in rural burkina faso. Plos One [Internet]. 2020 [access 15 jun 2021]; 15(11):e0242368. Doi: https://doi.org/10.1371/journal.pone.0242368 [ Links ]
15. Williams SP, Bryant KL. Sexually transmitted infection prevalenc among homeless adults in the United States: A systematic literature review. Sex trans. dis. [Internet]. 2018 [access 15 jun 2021]; 45(7):494-504. Doi: https://doi.org/ 10.1097/OLQ.0000000000000780 [ Links ]
16. Brito AKM, Medeiros HRL, Santos MLL, Nunes EM, Souza TA, Bezerra KKS. Prevalência de infecções sexualmente transmissíveis em mulheres assistidas na atenção básica de saúde. Temas em saúde [Internet]. 2018 [access 15 jun 2021]; 59-75. Available from: https://temasemsaude.com/wp-content/uploads/2018/10/fip201804.pdf [ Links ]
17. Pinto VM, Basso CR, Barros CRS, Gutierrez EB. Fatores associados às infecções sexualmente transmissíveis: inquérito populacional no município de São Paulo, Brasil. Ciênc. Saúde Coletiva [Internet]. 2018 [access 25 nov 2020]; 23(7): 2423-2432. Doi: http://dx.doi.org/10.1590/1413-81232018237.20602016 [ Links ]
18. Ezeonwu MC, Stecher HA, Carrick RN, Smith LA, Hoock J, Bain CE, et al. Risk factors and prevalence of symptons of sexually transmitted infections in Rural Mayan Villagens in Guatemala. Health Care for Women International [Internet]. 2020 [access 15 jun 2021]; 41(10): 1166-1181. Doi: https://doi.org/10.1080/07399332.2020.1791119 [ Links ]
19. Rowley J, Vander Hoorn S, Korenromp E, Baixo N, Unemo M, Abu-Raddad LJ, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ [Internet]. 2019 [access 25 nov 2020]; 97(8):548-562. Doi: https://doi.org/10.2471/BLT.18.228486 [ Links ]
20. Ribeiro LL, Moreira WC, Carvalho ARB, Sousa MCP, Carvalho ML, Castro TMBQ. Vulnerabilidade de pescadores de comunidades riberirinhas às infecções sexualmente transmissíveis. Revista Cubana de Enfermería [Internet]. 2017 [access 15 jun 2021]; 33(3). Available from: http://www.revenfermeria.sld.cu/index.php/enf/article/view/1231/288 [ Links ]
21. Santos MM, Menezes DDO, Oliveira LLC, Sampaio DC, Rivemales MCC. Perfil das infecções sexualmente transmissíveis em um município do recôncavo baiano. J Nurs Health [Internet]. 2020 [access 15 jun 2021]; 10(3):e20103006. Available from: https://periodicos.ufpel.edu.br/ojs2/index.php/enfermagem/article/view/18557/11863 [ Links ]
22. Braga LP, Szwarcwald CL, Damacena GN. Caracterização de mulheres trabalhadoras do sexo em capitais brasileiras, 2016. Epidemiol Serv Saúde [Internet]. 2020 [access 25 nov 2021]; 29(4). Doi: https://doi.org/10.5123/S1679-49742020000400002. [ Links ]
23. Haider MR, Kingori C, Brown MJ, Battle-Fisher M, Chertok IA. Illicit drug use and sexually transmitted infections among young adults in US: evidence from a nationally representative survey. International Journal of STD & AIDS [Internet]. 2020 [access 15 jun 2021]; 31(13). Doi: https://doi.org/10.1177/0956462420950603 [ Links ]
24. Wand H, Ward J, Bryant J, Delaney-Thiele D, Worth H, Pitts M, et al. Individual and population level impacts of illicit drug use, sexual risk behaviours on sexually transmitted infections among young Aboriginal and Torres Strait Islander people: results from the GOANNA survey. BMC Public Health [Internet]. 2016 [access 15 jun 2021]; 19(16). Doi: https://doi.org/10.1186/s12889-016-3195-6 [ Links ]
25. Silva AA, Silva KCO. Álcool e drogas ilícitas e doenças sexualmente transmissíveis entre adolescentes. R Interd [Internet]. 2017 [access 25 nov 2020]; 10(2):65-73. Available from: https://revistainterdisciplinar.uninovafapi.edu.br/index.php/revinter/article/view/1105 [ Links ]
26. Kuteesa MO, Weiss HA, Cook S, Seeley J, Ssentongo JN, Kizindo R, et al. Epidemiology of Alcohol Misuse and Illicit Drug Use Among Young People Aged 15-24 Years in Fishing Communities in Uganda. Int J Environ Res Public Health [Internet]. 2020 [access 15 jun 2021]; 17(7). Doi: https://doi.org/10.3390/ijerph17072401 [ Links ]
Received: June 25, 2021; Accepted: September 28, 2021











 text in
text in