My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.21 n.67 Murcia Jul. 2022 Epub Sep 19, 2022
https://dx.doi.org/10.6018/eglobal.508071
Originals
Quality of the clinical nursing records of a Neonatal - Intensive Care Unit
1Faculty of Nursing. University of Business and Social Sciences (UCES). Buenos Aires, Argentina
2Nursing Care Sciences Research Group. Magdalena University. Santa Marta, Colombia
3Maternal and Child Hospital “Ramón Sardá. Buenos Aires, Argentina
Introduction:
The clinical history is a record for monitoring the assistance provided by health professionals, which has legal and professional implications and is considered the cornerstone of the hospital information system. This must meet a series of characteristics or requirements in terms of content, order, documentary standardization and legibility which, in nursing practice, allow scientific knowledge as well as clinical practice to be related.
Objective:
To measure the quality of the nursing records of the Neonatal Intensive Care Unit of a public institution in the City of Buenos Aires, Argentina.
Method:
An Observational, analytical, and cross-sectional study. 396 nursing records, selected by random sampling, were analyzed. A comparison grid was used to identify compliance with the quality requirements of the registry determined according to legal and institutional requirements.
Results:
A general compliance with the quality criteria of 71.95% average (minimum compliance) was found, with the priority intervention areas being the recording of nursing diagnoses and the response to nursing care. The shift and the training level showed a relationship with better general indexes in the different dimensions.
Conclusions:
It is expected that the results of this study can contribute to the identification of areas of intervention to improve the recording of care and activities performed by nursing professionals, while seeking to increase resources to address the issue.
Keywords: Nursing Records; Quality Management; Nursing Process
INTRODUCTION
Evidence-Based Nursing (EBN) has been considered in healthcare practice as a relevant tool for improving the quality of care by promoting timely and efficient care, improving care management, and reducing the possibility of errors in daily practice1. However, this process deserves the generation of reliable information about our actions, considering the patient record as the document within the hospital practice in which our actions are reflected upon, also known as the nursing clinical record, for what it becomes imperative the analysis of the registration processes as a first instance for the assessment of evidence-based practice.
The registration process is regulated by statutes that seek to ensure patient safety. In Argentina, Chapter IV of Law 26 529 of 2009, Law on Patient Rights, Medical History, and Informed Consent, establish aspects related to the structure of the Medical History (MH) registry, including the data to be recorded and other legal aspects such as integrity, uniqueness, inviolability, legitimacy, access, and the penalties applicable to those who fail to comply with the obligations of the legislation2.
In terms of structure, the Argentine legislation mentions that the MH should include the date on which the record was initiated, the identifying data of the patient and his or her family nucleus, data of the intervening professional, relevant history (genetic, physiological and pathological), all medical acts performed (medication supplies, practices, main and complementary studies, diagnosis, prognosis, evolution, among others) and that they should be clear, accurate, complete and legible2. It is important to recognize that nursing professionals, together with other healthcare professionals, oversee patient care, and are responsible for the entries in the registry and for the information that is omitted, and in the event of non-compliance, as mentioned in the legislation, sanctions are entailed as they constitute a risk in the quality assurance of healthcare.
An accurate medical record not only improves effective communication through continuity of care, but also positively impacts on the quality of patient care by protecting patients from potential health care-related harm1.
From the nursing discipline, it has been referred that the documentation should be succinct, systematic, and chronological, following the phases of the Nursing Process (NP), since it allows the possibility of systematically assessing the health problems, both real and potential, negative and positive, of the person and his/her family, with the ultimate purpose of satisfying the health needs that are detected3. The NP emerged in the mid-twentieth century and allowed the adoption of a logical scheme of action for nursing professionals, oriented towards the provision of client-centered care4. It is composed of five sequential steps: Assessment, Diagnosis, Planning, Implementation and Evaluation, which represent the logical and sequential form for the subsequent documentation of care. The nursing professional should record what is observed, measured, interpreted, and experienced by the patient, the resulting nursing diagnosis, the interventions performed (both autonomously and in collaboration), and the evaluation of the results after the identification and intervention of a problem.
There is a growing interest in improving the quality of health care, which has relevant implications in the health service, so nursing records must be accurate and accepTable. As mentioned by several authors, the records filled out by the nursing staff have been written in a repetitive manner, showing the lack of significant data on the patient's health status and evolution, and consequently showing crucial inaccuracies of legal relevance5,6. It is therefore essential for the quality assurance of health care to be committed to patient safety, with nursing clinical records being a relevant issue as evidence for quality control7.
Currently, health institutions adhere to the practice of monitoring and reviewing records, since they serve as a reflection of the organization and quality of health care8. Due to their legal nature, nursing records represent a support to the work of the professionals of the discipline; however, due to their variability, complexity, and lack of unification in the criteria, in many opportunities, these records do not show in writing the care provided9. Some authors highlight the need to follow up on the quality compliance of the records and to develop a continuous improvement plan10. Studies related to the follow-up of nursing records specifically serve to assess the quality of care provided by this group of professionals3.
A study conducted by Rojas & Pastor described, by means of self-reporting, that 78.5% of the nursing professionals in Intensive Care Units applied the NP11. Regarding the phases, they described that 95.4% performed the activities of assessment (95.4%), intervention (87.7%), planning (75.4%), diagnosis (61.5%) and evaluation (60.0%); However, in studies that have measured the application of the NP and the recording of the activities, it has been described that the aforementioned activities were not fully integrated, were omitted or there was no concordance between them12-14. In addition, other studies have described that nursing professionals who work in stressful environments are 81% less likely to implement the EP, while those with good management and knowledge of the NP are 8.38 times more likely to implement it15.
Considering that records and their components have undergone variations over the years, and differ in their characteristics between professions, specialties and adapt to the regulations of each country, it is necessary to design tools that allow the identification of the necessary components of the clinical record, this aspect as the first challenge in the evaluation of the quality of the records.
Therefore, the present study was designed with the objective of measuring the quality of the nursing records of the Neonatal Intensive Care Unit of a public health institution in Buenos Aires, Argentina, based on the dimensions of the record: Structure and Nursing Process.
METHOD
Population and sample
The population consisted of the clinical nursing records (nursing notes) of the Neonatal Intensive Care Unit of a public health institution. The sample was calculated considering the formula for calculating the sample for infinite populations and seeking to achieve a 95% confidence level and a 5% margin of error. This resulted in the need to carry out 377 observations, to which an estimated loss percentage of 20% was added, according to similar studies, to prevent human errors in the application of the collation grids. The final sample consisted of 396 observations from the different shifts (day, night, and weekends), thus fulfilling the purpose of the work. The simple random sampling was used.
The data were collected between May and December 2019.
Procedure
Initially, a search for studies related to the subject was carried out in different databases (Scielo, BHL, Scholar Google and PubMed) in English and Spanish. The areas referred to the quality of the records in the different studies were identified. This review was complemented with the requirements outlined in current legislation and with a detailed analysis of the nursing clinical record form of the institution.
Under the above standards, a preliminary version of the instrument was prepared, developing a series of statements considered critical and assessed according to a dichotomous scale (Complies=1 point, Does not comply=0 points). Next, the main variables addressed by the instrument were determined: Structure of the record and Nursing Process. The dimensions of the first case were Patient Identification and Record Characteristics, while in the second case were Assessment, Diagnosis, Planning, Implementation and Evaluation.
In order to achieve content validity, the instrument underwent validation by experts, who were considered according to their knowledge and expertise and who made group observations and individual revisions, which were implemented in the instrument. These observations were mostly semantic corrections.
The final version of the instrument consisted of 44 items valued at 40 points corresponding to the Global Efficiency Index (GEI) of the nursing record, which is the sum of the two dimensions: Global Efficacy Index of the structure (GEIS) of the nursing record (18 items/18 points) and the Global Efficacy Index of the process (GEIP) (25 items/22 points). A pilot test of 6 observations was carried out, obtaining positive results.
The instrument included questions based on the sex and level of training of the professional who filled out the registry, and also the shift in which it was filled out for comparative analysis.
Data collection
The data were collected at the end of the shifts, so that there was no intervention in the process of filling out the records or in the work dynamics of the professionals. A check grid was also implemented.
Data analysis
The information collected was tabulated in a database in Microsoft Excel and analyzed using InfoStat v/L software (version 29-09-2020). Descriptive statistical measures such as absolute (n) and relative (%) frequency were calculated. Relationships between variables were calculated using the Mann-Whitney U and Kruskal-Wallis tests. The Chi2 test (X2) was used to identify independence between dichotomous categorical variables. A significance level (SL) ofp<0.05 was set.
RESULTS
Sample description
A total of 466 nursing records were included in the study, of which 396 were found to be correctly filled in the check grid, corresponding to the final sample.
The records corresponded to 6-hour shifts, distributed in three groups: day and night from Monday to Friday and 12 hours on weekends and holidays, in a total of 285 (72%) of the first two and 111 (28%) observations of the second. Regarding sex, 317 records (80%) were filled out by women and 79 (20%) by men; and regarding the level of training, 270 (68%) were filled out by Nursing Technicians and 126 (32%) by Registered Nurses.
Structure of registry
When reviewing the structure of the nursing records, it was found that the indicators with the highest compliance in the dimension ofpatient identificationwere the placement of the first and last name (99.7%), gestational age at birth (99.5%), current date (99.3%), number of days of life (99.2%) and date of birth of the child (99.0%); while the date of admission, placement of the first and second bracelet were the least compliant with 69.7%, 70.2% and 69.9% compliance, respectively (Table 1).
In the dimensionCharacteristics of the record, it was found that correct spelling and grammar were the indicators with the highest compliance with percentages of 96.7% and 96.7%, respectively. On the other hand, the time of recording and the registration number of the professional caregiver were only complied with by 39.4% and 41.4%, respectively (Table 1).
Nursing Process
Regarding the registration of the Nursing Process, in the assessment dimension an average compliance of 72.5% was found. Compliance with the recording of heart rate, blood pressure, oxygen saturation and current weight of the newborn were greater than 90.0%, while tolerance to feeding and the description of two or more organic systems were recorded in 20.2% and 35.6%, respectively. In the diagnosis dimension the compliance was 0.2%, with only one registry that included at least one nursing diagnosis.
In the planning and execution of the nursing interventions, it was found that the volume intake, parenteral hydration, and elimination were recorded at a level higher than 95.0%, while there was a relationship between the interventions performed by the nursing professionals with the medical diagnoses in 26.3% of the records.
In relation to the interventions performed in collaboration with medical staff, the recording of transfusions volume was recorded in 99.3% and the recording of the blood draw volume was recorded in only 61.3% of occasions. Interventions in collaboration with other professionals were poorly recorded, with compliance rates ranging from 4.6% to 40.1%.
Finally, in the evaluation dimension, it was found that 39.6% described the user's responses to nursing care manifested in vital signs and 35.8% described the patient's response to nursing care, in at least two organ systems.
Inferential analysis
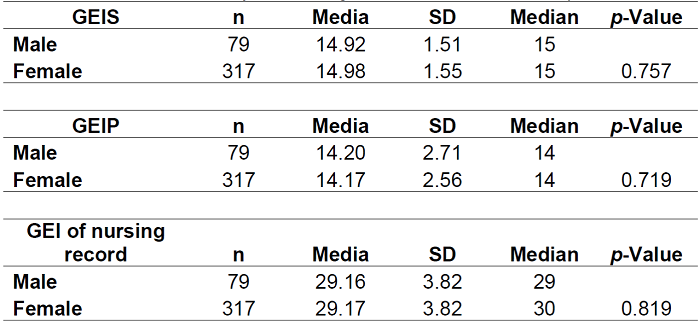
It was found that in the Global Efficacy Index of the structure (GEIS), the average score of the sample was 14.97 out of 18 maximum points, representing 83.1% compliance. Meanwhile, the Global Efficacy Index of the process (GEIP) was 13.81 on average out of 22 maximum points, representing 62.77% compliance. Regarding the Global Efficiency Index (GEI) of Nursing Records, the average score was 28.78 out of 40 total points, representing 71.95% compliance (Table 2).
When investigating the relationship between the dimensions of the instrument and the work shift, it was found that the GEIS dimension had higher scores in the night shift (p:<0.001). The GEIP and GEI of nursing record dimensions showed no relationship with the work shift (Table 3).
When analyzing the quality of the nursing record and its relationship with the sex of the professional who fills it out, no statistically significant differences were detected, so it can be said that there is no relationship between these variables (Table 4).
Finally, a relationship was found between the level of education and the quality of the nursing record, with higher GEI in those completed by Registered Nurses (χ2: 6.81,p:0.009).
DISCUSSION
As the complexity of health care increases, it is necessary to have strategies to ensure effective communication in which patient safety is the fundamental axis. The nursing clinical record thus enables to monitor the continuity of care, while providing safe care and allowing the review of decisions made for carrying out nursing interventions7.
The Nursing Process is conceived as the method that underlies the professional nursing practice, so it is imperative not only to be known and applied in practice, but also to leave written evidence of its implementation in the nursing records8,16. The results of the present study highlight shortcomings regarding the documentation of the NP in its different steps, fact which highlights the relevance of conducting studies to monitor the quality of the records and the implementation of continuous improvement plans, as detailed in the literature consulted.
In our study, according to the record structure, we found a compliance of 82.5%, and the priority intervention areas were identified as inadequate correction of errors, signature without including the professional registration number, and the lack of annotation of the time of completion of the registry. In addition, other variables specific to the service, such as the recording of the neonatal bracelet (wristband) numbers, were found to be deficient. The data of the present study do not coincide with the findings of similar studies in which the level of compliance with the registry structure was found to be high, and the areas that presented deficiencies were those related to the documentation of water balance and vital signs, and also the use of unofficial abbreviations17.
When analyzing compliance with the recording of nursing diagnoses, low adherence to the recording of these diagnoses was found, with a level of compliance of less than one percent. When comparing these findings with the scientific evidence, it was found that the studies refer to levels of compliance in this area ranging from 0% to 100%12,18. The differences in the aforementioned studies are due to aspects such as the use of records that incorporate specific and mandatory sections for the incorporation of the nursing diagnosis, the measurement of compliance after staff training, the use of institutional protocols and guidelines for filling out nursing notes and the use of electronic medical records, which have proven to have a positive impact on the implementation of the nursing diagnosis in professional practice and in its reporting.
At a general level, we identified a level of compliance with the quality requirements of the registry of 71.95%, which is lower when compared with similar studies. In this regard, a study conducted in Mexico reported a level of compliance with the quality of the nursing clinical record of 95.59%18. This study analyzed quality by means of the dimensions of identification, assessment, diagnosis, activities, evaluation, and elaboration, and categorized the records as "excellent" when compliance was obtained in the 91-100% range of the checklist. However, it is worth noting that the study analyzed the level of adherence of the record to the legal regulations in Mexico but had a small sample (n:54). Another study by Lopez-Cocotle et al.19in Mexico, which included 105 nursing notes, it was found that the indicators with the greatest deficits were identification, rating, evaluation, and elaboration, while in our study the dimensions diagnosis, evaluation and planning were the worst evaluated.
On the other hand, Pokorski et al.12describe in their study that the physical examination was recorded in 3% of the observations of records made, while the patient's evolution reached 95% compliance. In our case, the assessment was recorded in 72.5% and the evolution in less than 40% of the cases, depending on the item analyzed.
From the review conducted, the concern and relevance of the analysis of the quality of the records is evident, and this is reiterated in studies such as those of Muinga et al. (8), Melo et al.14, Gaedke Nomura et al.20, and Akhu-Zaheya et al.21, which highlight the need to implement educational interventions aimed at improving the quality of record keeping, which also showed a significant impact on the mastery of nursing diagnoses as a process and product, as well as nursing interventions and outcomes. Other strategies reported to improve the quality of the records are the integration of the Nursing Process to the electronic medical record22. Based on this, the present study constitutes a starting point for the design of strategies aimed at improving the registry, beginning with the areas identified as priorities for intervention.
Finally, the literature agrees that the quality guidelines for registries differ between regions, countries and even institutions, so that specific tools must be designed to address the variability of aspects to be assessed, which supports the design and validation of specific instruments for each environment.
CONCLUSIONS
In our study, we found overall compliance levels of 71.95%, being the incorporation of nursing diagnoses and the evaluation of the patient's response to prescribed and applied nursing care, the areas that deserve prioritization for intervention.
It was found that, in the night shift, there was a higher level of quality of the records compared to other work shifts. The sex of the professional who filled out the registry showed no relationship with the quality of the record. The level of training was related to the quality of the record, with higher indexes being identified in those with undergraduate training.
It is necessary to implement strategies aimed at the systematic follow-up of the writing and training of nursing professionals for the correct filling out of clinical records, which also involves reinforcing knowledge of the nursing process with emphasis on the identification and recording of nursing diagnoses.
REFERENCIAS
1. Rodríguez Campos V, Paravic Klijn T. Enfermería basada en la evidencia y gestión del cuidado. Enferm Glob [Internet]. 2011 [Citado 18 diciembre 2021];10(24). Doi: https://dx.doi.org/10.4321/S1695-61412011000400020. [ Links ]
2. Ley 26529, Derechos del Paciente, Historia Clínica y Consentimiento Informado [Internet]. 2009 [Citado 13 enero 2022]. Disponible en: http://servicios.infoleg.gob.ar/infolegInternet/anexos/160000-164999/160432/norma.htm. [ Links ]
3. Hernández Cantú EI, Reyes Silva AK, García Pineda M. Cumplimiento de los registros clínicos, esquemas terapéuticos e intervenciones de enfermería en un hospital de segundo nivel de atención. Rev Enferm Inst Mex Seguro Soc [Internet]. 2018 [Citado 15 diciembre 2021];26(2):65-72. Disponible en: http://revistaenfermeria.imss.gob.mx/editorial/index.php/revista_enfermeria/article/view/336/828. [ Links ]
4. Cuevas Budhart M, González Martínez B, Álvarez Bolaños E, Barrera García MJ, de Almeida Souza A, González Jurado MA, et al. Diseño y validación de un nuevo registro clínico de enfermería, para la continuidad de los cuidados y seguridad del paciente en hemodiálisis. Enferm Nefrol [Internet]. 2019 [Citado 05 junio 2021];22(2):168-175. Doi: https://dx.doi.org/10.4321/s2254-28842019000200008. [ Links ]
5. McCarthy B, Fitzgerald S, O'Shea M, Condon C, Hartnett-Collins G, Clancy M, et al. Electronic nursing documentation interventions to promote or improve patient safety and quality care: A systematic review. J Nurs Manag [Internet]. 2019 [Citado 18 diciembre 2021];27(3):491-501. Doi: https://dx.doi.org/10.1111/jonm.12727. [ Links ]
6. Dal Sasso GT, Barra DC, Paese F, Almeida SR, Rios GC, Marinho MM, et al. Computerized nursing process: Methodology to establish associations between clinical assessment, diagnosis, interventions, and outcomes. Rev Esc Enferm USP [Internet]. 2013 [Citado 30 Abril 2021];47:242-9. Doi: https://dx.doi.org/10.1590/s0080-62342013000100031. [ Links ]
7. De Groot K, Triemstra M, Paans W, Francke AL. Quality criteria, instruments, and requirements for nursing documentation: A systematic review of systematic reviews. J Adv Nurs [Internet]. 2019 [Citado 14 octubre 2021];75(7):1379-1393. Doi: https://dx.doi.org/10.1111/jan.13919. [ Links ]
8. Muinga N, Abejirinde IO, Paton C, English M, Zweekhorst M. Designing paper-based records to improve the quality of nursing documentation in hospitals: A scoping review. J Clin Nurs [Internet]. 2021 [Citado 18 diciembre 2021];30(1-2):56-71. Doi: https://dx.doi.org/10.1111/jocn.15545. [ Links ]
9. Quevedo G. Evaluación de la calidad de los registros de enfermería en el área de trauma shock del servicio de emergencia. Hospital Regional Lambayeque 2015 [Internet]. 2017 [Citado 5 diciembre 2021]. Disponible en: http://hdl.handle.net/20.500.12423/1359. [ Links ]
10. Palomino Márquez SN. Nivel de cumplimiento de los registros de Enfermería en el Servicio de Emergencia del Hospital Vitarte nivel II-1 del MINSA, Lima 2018 [Internet]. 2018 [Citado 18 enero 2022]. Disponible en: https://hdl.handle.net/20.500.12692/23413. [ Links ]
11. Rojas J, Pastor P. Aplicación del proceso de atención de enfermería en cuidados intensivos. Invest Educ Enferm [Internet]. 2010 [Citado 17 noviembre 2021];28(3):323-335. Disponible en: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-53072010000300003. [ Links ]
12. Pokorski S, Moraes MA, Chiarelli R, Paganin A, Rejane E. Proceso de Enfermería: De la literatura a la práctica: ¿Qué estamos haciendo, de hecho? Rev Latino-am Enfermagem [Internet]. 2009 [Citado 7 septiembre 2021];17(3):302-7. Doi: https://doi.org/10.1590/S0104-11692009000300004. [ Links ]
13. Tajabadi A, Ahmadi F, Sadooghi Asl A, Vaismoradi M. Unsafe nursing documentation: A qualitative content analysis. Nurs Ethics [Internet]. 2020 [Citado 18 diciembre 2021];27(5):1213-1224. Doi: https://dx.doi.org/10.1177/0969733019871682. [ Links ]
14. Melo LS, Figueiredo LS, Pereira JM, Flores PV, Cavalcanti AC. Effect of an educational program on the quality of Nursing Process recording. Acta Paul Enferm [Internet]. 2019 [Citado 8 noviembre 2021];32(3):246-253. DOI: https://doi.org/10.1590/1982-0194201900034. [ Links ]
15. Shiferaw WS, Akalu TY, Wubetu AD, Aynalem YA. Implementation of Nursing Process and Its Association with Working Environment and Knowledge in Ethiopia: A Systematic Review and Meta-Analysis. Nurs Res Pract [Internet]. 2020 [Citado 5 diciembre 2021];2020:6504893. Doi: https://doi.org/10.1155/2020/6504893. [ Links ]
16. Ruíz-Cano LA, Gómez-Trujillo JN, Cuevas-Guajardo L, Martínez-Vega AL. Coherencia diagnóstico/intervención de enfermería en la hoja de registros clínicos y uso de lenguaje estandarizado. Rev CONAMED [Internet]. 2017 [Citado 16 agosto 2021];22(4):161-165. Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=79256. [ Links ]
17. Elera Peña E, Palacios Jacobo K. Registros de enfermería: Calidad de las notas en los servicios oncológicos. Rev Cienc y Arte Enferm [Internet]. 2019 [Citado 8 julio 2021];4(1-2):48-55. Doi: https://doi.org/10.24314/rcae.2019.v4n1.09. [ Links ]
18. López-Cocotle J, Moreno-Monsiváis M, Saavedra-Vélez C. Construcción y validación de un registro clínico para la atención asistencial de enfermería. Enfermería Universitaria [Internet]. 2017 [Citado 21 mayo 2021];14(4):293-300. Doi: https://doi.org/10.1016/j.reu.2017.08.001. [ Links ]
19. López-Cocotle J, Saavedra-Vélez C, Moreno-Monsiváis M, Flores de la Cruz S. Niveles de cumplimiento de calidad del registro clínico de enfermería. Revista Electrónica Medicina Salud y Sociedad [Internet]. 2015 [Citado 23 octubre 2021];6(1):65-77. Disponible en: https://www.researchgate.net/publication/318967258_Niveles_de_cumplimiento_de_calidad_del_registro_clinico_de_enfermeria. [ Links ]
20. Gaedke Nomura A, Barragan da Silva M, de Abreu Almeida M. Calidad de los registros de enfermería antes y después de la Acreditación Hospitalaria en un hospital universitario. Rev Latino-Am Enfermagem [Internet]. 2016 [Citado 14 julio 2021];24:e2813. Doi: https://doi.org/10.1590/1518-8345.0686.2813. [ Links ]
21. Akhu-Zaheya L, Al-Maaitah R, Bany Hani S. Quality of nursing documentation: Paper-based health records versus electronic-based health records. J Clin Nurs [Internet]. 2018 [Citado 20 enero 2022];27(3-4):e578-e589. Doi: https://doi.org/10.1111/jocn.14097. [ Links ]
22. Guadarrama-Ortega D, Delgado-Sánchez P, Martínez-Piedrola M, López-Poves E, Acevedo-García M, Noguera-Quijada C, et al. Integración del proceso enfermero en la historia clínica electrónica de un hospital universitario. Rev Calid Asist [Internet]. 2017 [Citado 20 enero 2022];32(3):127-134. Doi: https://doi.org/10.1016/j.cali.2017.02.004. [ Links ]
Received: January 20, 2022; Accepted: February 09, 2022











 text in
text in