My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Enfermería Global
On-line version ISSN 1695-6141
Enferm. glob. vol.19 n.58 Murcia Apr. 2020 Epub May 18, 2020
https://dx.doi.org/eglobal.389381
Originals
Characterization of psychoactive drugs users residing in therapeutic communities in Brazil
1Federal University of Mato Grosso (UFMT), Araguaia University Campus (CUA) and Ribeirão Preto School of Nursing, University of São Paulo (EERP-USP). Brazil.
2Federal University of Mato Grosso (UFMT) Araguaia University Campus (CUA). Brazil.
3State University of Mato Grosso (UNEMAT) Campus Tangará da Serra. Brazil.
4Ribeirão Preto School of Nursing, University of São Paulo (EERP-USP). Brazil.
Introduction
The consumption of psychoactive drugs is increasing, precocious and abusive, causing chemical dependence. This dependence requires treatment and control. One of the places available in Brazil for this host is the therapeutic community service.
Methods
cross-sectional, quantitative descriptive study with drug users from three therapeutic communities, located in the interior of the Central-West region of Brazil. For data collection, a semi-structured questionnaire was used, whose responses were analyzed and analyzed in the BioEstat version 5.0 program, after ethical approval by the University of Sao Paulo, under opinion 2,487,000.
Results
21 men, young adults, single, low schooling, unemployed and with religion participated. The use of drugs was precocious, through alcohol, tobacco and marijuana, used by friends and curiosity. There was a history of multiple admissions to treat chemical dependence, with the therapeutic community being the most sought after service. Family conflict, loss of reemployment, and problems with mental health, as well as the way in which the user considers the treatment received and the willingness to use drugs during treatment have been strongly associated with drug use.
Conclusion
Knowing the profile of drug users can subsidize health actions aimed at meeting the integral demands of users, contributing to the elaboration of public policies and rehabilitation strategies that contribute to adherence to treatment.
Keywords: Drug Users; Mental Health; Substance Abuse Disorders
INTRODUCTION
Worldwide, it has been observed that drug use is increasingly crescent, early and abusive. Particularly, the illicit drugs are seen as a constant reason for research and intervention, however, other drugs, especially alcohol, which has the highest consumption recorded in the Americas and is consequently responsible for the greatest damage and complications1.
Increased consumption has been causing chemical dependency in various age groups, gender and family settings. Chemical dependency is considered a chronic and multifactorial disease, which causes brain changes, challenging the balance of social behavior and self-control to maintain sobriety. And it requires treatment and follow-up for a long period2.
In Brazil, the Therapeutic Communities (CT) are one of the existing places aimed at the treatment of this addiction, although researchers advise against this form of care3. They are understood as a model of collective / community care, aimed at users who abuse psychoactive drugs, however, in sTable clinical conditions and have the change of behavior and beliefs as therapy4.
Although therapeutic communities are spread across the world, it has become a challenge to take care of this profile of people, associated with the diversity of histories and contexts of life. For this care to meet the needs of its users, therapeutic projects need to be established and some aspects are necessary in directing personalized care to be performed, such as considering the profile of users5.
Thus, the study was developed according to the guiding question, which was “What is the profile of psychoactive drug users residing in therapeutic communities?” The objective of this research was to identify the profile of users of psychoactive drugs residing in therapeutic communities.
MATERIALS AND METHODS
Cross-sectional, descriptive study with a quantitative approach, carried out in three therapeutic communities located in the interior of the Central-west region of Brazil, from March to May 2018. The choice of these CTs was for convenience following the criteria, occurred due to the similarity in the modality of male recovery and because they are considered reference units for the Araguaia Valley region.
The research population was composed of 29 men residing in these CT. The sample was for convenience, having as inclusion criteria being over 18 years old, living at least one week in one of the three CTs. Individuals who were not in the CT in the last 24 hours were excluded due to treatment abandonment or temporary leave for medical and judicial consultations. After applying these criteria, a sample of 21 users was reached.
Data collection occurred through an interview with a semi-structured script, composed of objective questions about sociodemographic aspects (gender, age, marital status, education, ethnicity, family income, profession and religion) and which addressed the profile of psychoactive drug use, consequences consumption and the type of treatment received in the CT.
The data were organized and processed in the Microsoft Excel 2013 program and analyzed using descriptive statistics by the Bioestat version 5.0 program, through the correlation analysis “Contingency Coefficient C” (result of C = 0, determines that there is no association between the variables, when C ≠ 0, it determines that there is an association between two variables (0.1 weak, 0.1 to 0.3 moderate and> 0.3 strong), with a significance level of 5% (p= 0.05)6.
The study was approved by the Research Ethics Committee of the School of Nursing at the University of Sao Paulo, Ribeirão Preto, SP, Brazil, under CAAE: 68444017.8.0000.5393 and opinion No. 2,487,000, having strictly respected all ethical principles and guidelines research involving human beings, in compliance with Resolution 466/2012 of the National Health Council. All participants agreed to participate by signing the Free and Informed Consent Form (FICF).
RESULTS
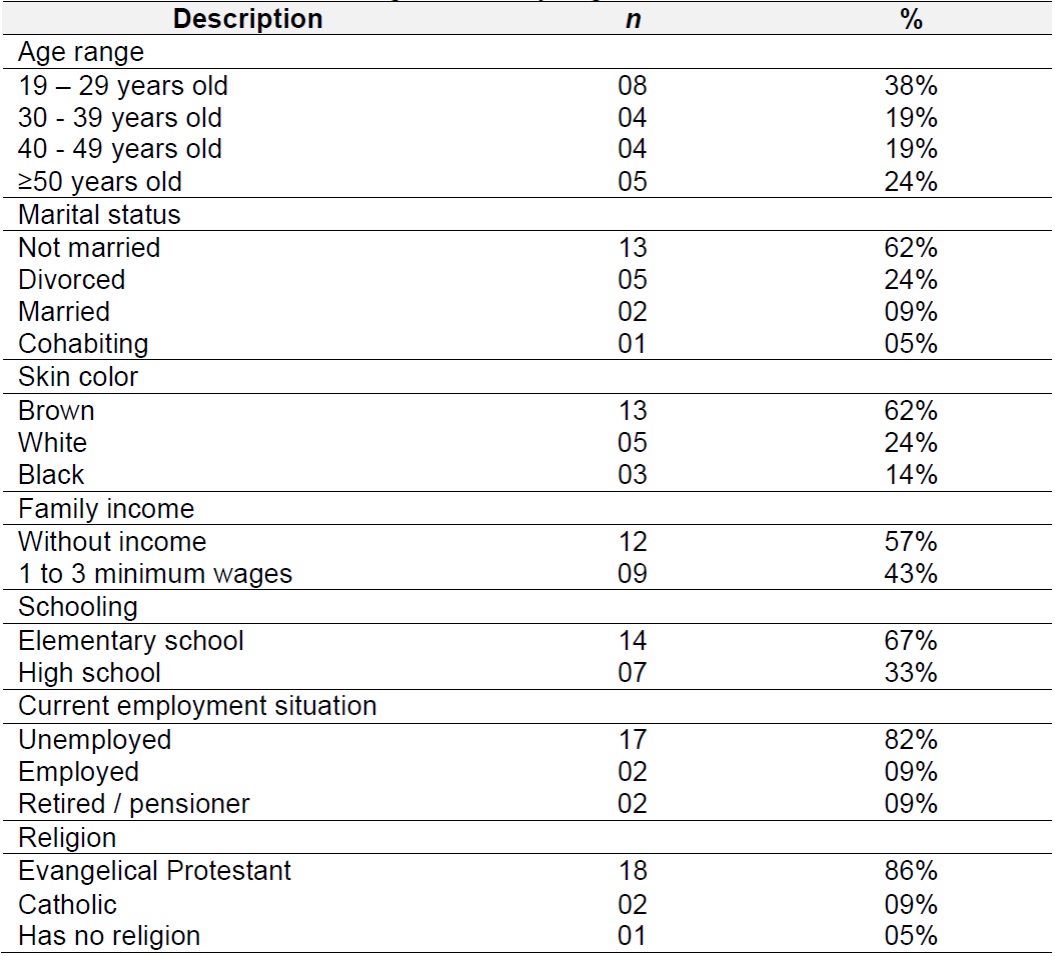
Table 1, shows that the study participants were aged between 19 and 61 years old, with an average age of 37.57 years old and who declared themselves to be brown (62%). There was a greater distribution of users aged between 19 and 39 years old (57%), single (62%), having completed complete / incomplete elementary school (67%), unemployed (82%), without family income (57%) and with religion (86%).
Table 1. Distribution of users according to sociodemographic characteristics. Araguaia Valley region, Brazil, 2018. n= 21
As for the consumption of psychoactive drugs, Table 2shows that 76% of the participants reported a family history of this consumption, occurring by a first-degree (8) and second-degree (8) relative. The consumption of psychoactive drugs started between 11 and 18 years old (84%), with alcohol (48%) being the drug of choice, followed by tobacco (24%) and marijuana (19%), used under the influence of friends (48%) and curiosity (43 Before treatment, the most consumed drug, that is, that contributed to the addiction process from the users' perspective, was crack cocaine (48%), followed by alcohol (28%).
As for the characteristics related to the treatment received, the sample was composed mainly of users who sought treatment voluntarily (67%), with a history of multiple hospitalizations to treat chemical dependence (67%), with more than two hospitalizations (67%), with the therapeutic community being the most sought service as a treatment resource (63%). When health care was needed, users were welcomed by services linked to the Psychosocial Care Network - RAPS (96%), including Family Health Strategy (ESF), Psychosocial Care Center (CAPS AD) and public hospital (Table 2).
Table 2: Distribution of the sample according to the consumption of psychoactive drugs and the treatment received. Araguaia Valley region, Brazil, 2018. n= 21
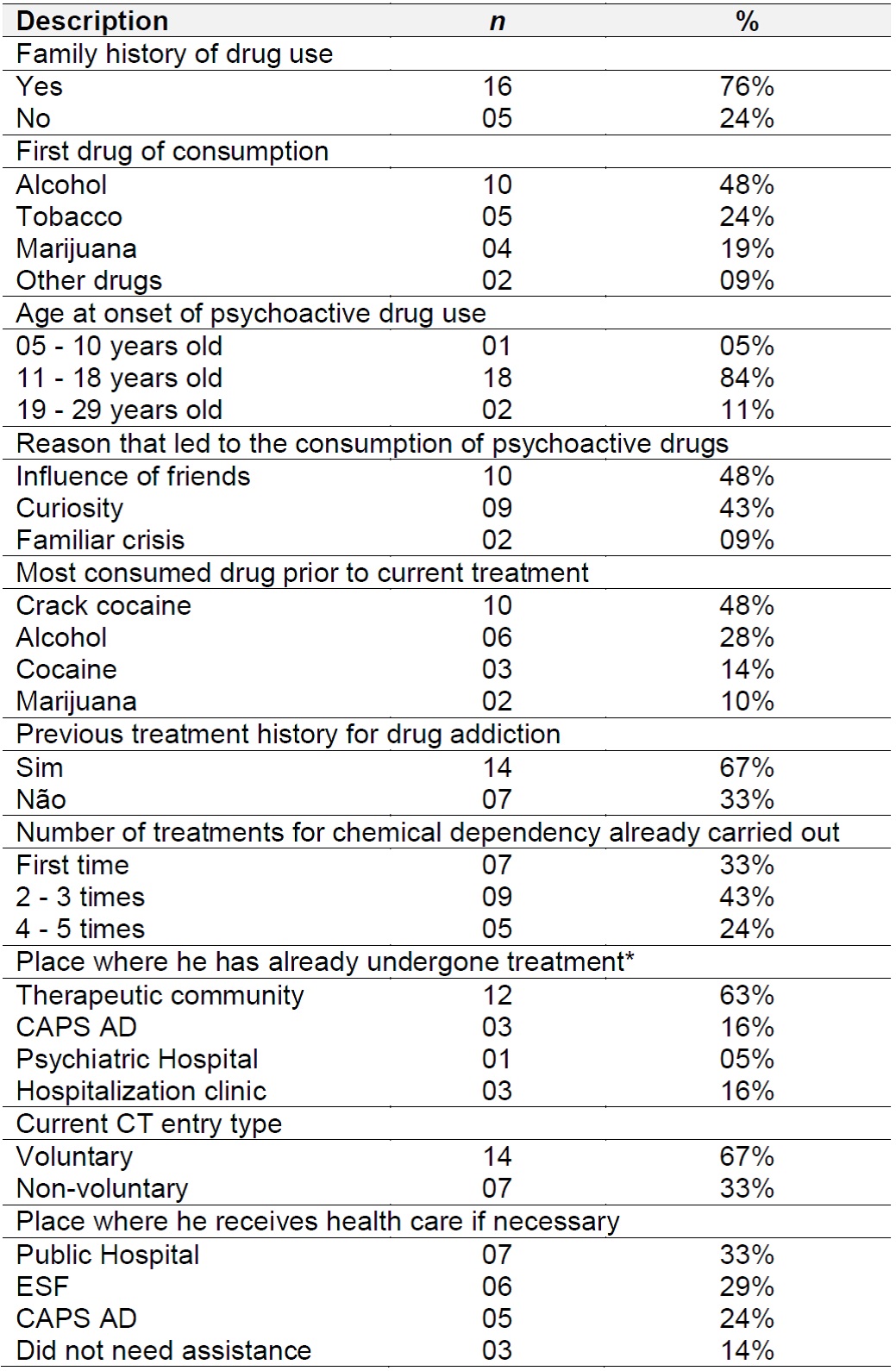
*Users could indicate more than one alternative referring to the place they have already sought to treat drug addiction (N=19). CAPS AD: Psychosocial Care Center for Alcohol and Drugs; PSF: Family Health Program
Regarding the consequences of drug use among the participants, the association test revealed a strong relationship between family conflict (C = 0.408), the loss of paid work (C = 0.417) and problems with mental health (C = 0.322), while the other tested variables pointed to a less expressive relationship (moderate or weak) between learning difficulties (C = 0.270), problems with justice (C = 0.152), dropping out of studies (C = 0.015) , material and financial losses (C = 0.195), involvement in fights (C = 0.015) and problems with physical health (C = 0.195).
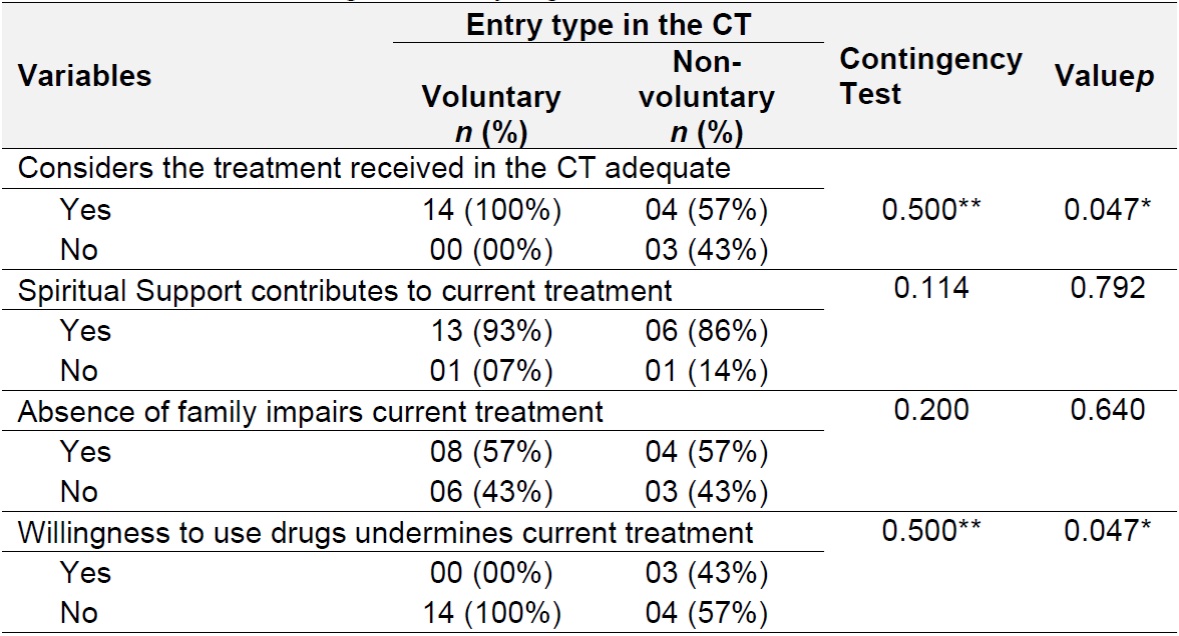
Table 3shows a strong relationship with the way the user considers the treatment received (C = 0.500, p = 0.047) and the desire to use drugs during the current treatment (C = 0.500, p = 0.047), association not identified with the same expressiveness between the other variables (Table 3).
DISCUSSION
To start the discussion, a survey was made in the Scielo database (www.scielo.org) in search of finding articles that could contribute to this phase of the research that addressed therapeutic communities and users of the therapeutic community. 109 articles considered potentially relevant were found and appreciated through their titles and abstracts, regardless of the year, country and language published. Of this total, six were included to compose charts 1 and 2 for comparison, as they present data on the participants' profile in their content. Other studies have also been used to support this discussion.
The comparisons of this research with other studies are approximate, since there was no standardization regarding the variables investigated. It is necessary to consider that it was not possible to find an investigation that indicated an outline close to the results presented here, regarding the type of participating institution, the number of institutions investigated and the sample size.
It was also observed an absence of standardization among the categories that define the age group, schooling and skin color. Therefore, there are many differences and because of that, an attempt was made to make approximations with the data from the present study and to make it more evident, a chart Table was elaborated with the main verified results of this and other researches (Chart 1).
Chart 1: Summary of the main sociodemographic results found among the studies available for consultation in the 2014-2018 period in the Scielo database.
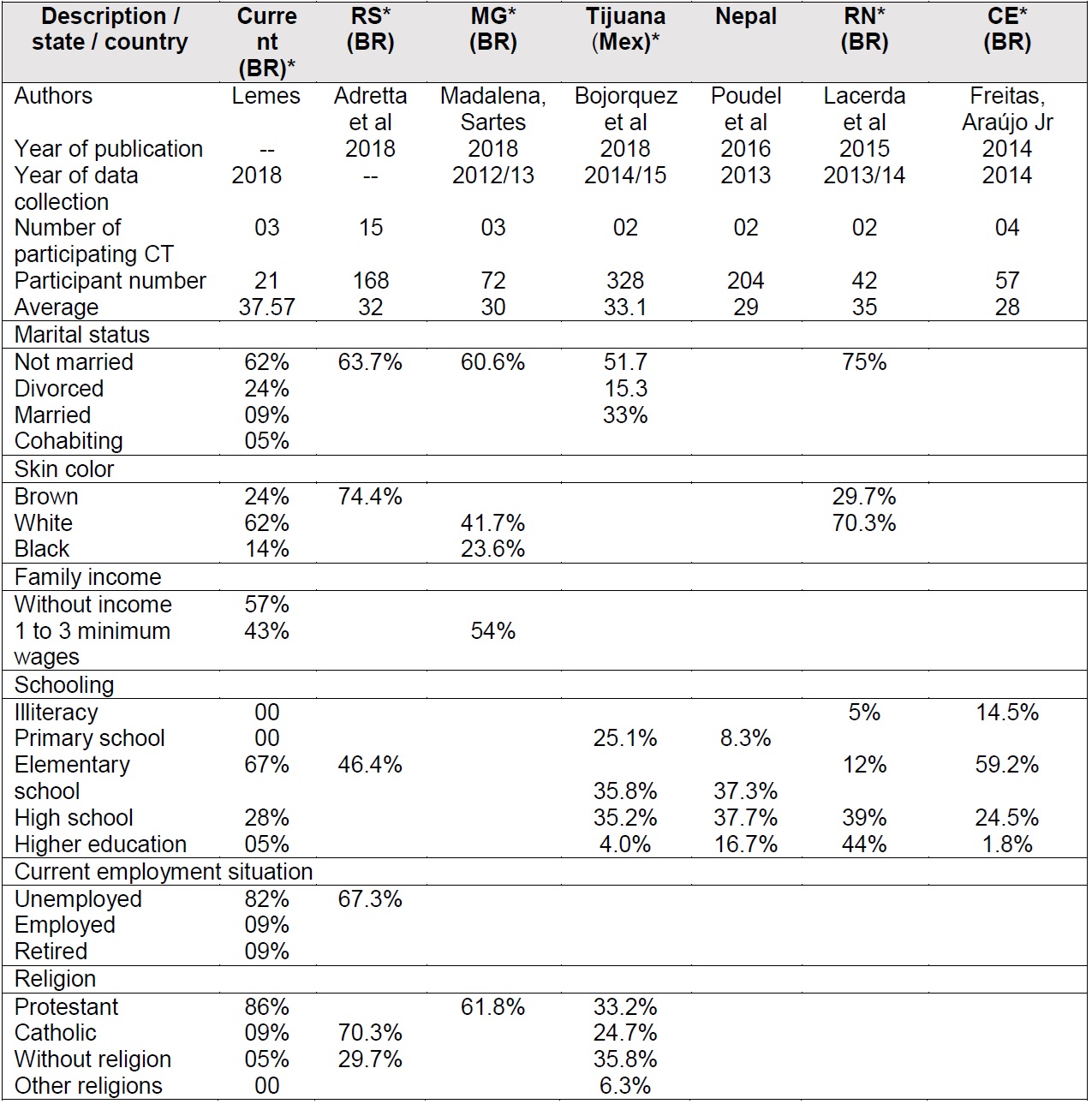
*Brazil (BR); Rio Grande do Sul (RS); Minas Gerais (MG); México (MEX); Rio Grande do Norte (RN); Ceará (CE).
In terms of age, as a standardization was not found, it was decided to use the average age between 287and 37.57 years, a time interval in which people are considered as young-adult, full of strength and vitality.
Regarding marital status, there was a predominance of single users in Tijuana (MEX)8, Rio Grande do Sul (BR)9, Minas Gerais10and Rio Grande do Norte (BR)11, which corroborates the findings of this research. Both data reveal the difficulty of these users to establish or maintain relationships, the difficulty of these users in forming affective bonds, which compromises their social bonds.
Regarding the skin color, the similarities are also partial since they categorized this information into different types. Among the studies that reported this data, there were similarities with research from Minas Gerais10and Rio Grande do Norte11, pointing to a predominance of self-declared people as brown race.
Regarding schooling, although the data presented a similar pattern, it can be said that they corroborate with the present study by revealing a predominance of little education among users from Rio Grande do Sul (BR)9, Ceará7, México8and Nepal12. Both data show that the investigated samples consist of people with low education, which ends up reflecting on the low professionalization and, consequently, on better job opportunities.
Most users of psychoactive drugs showed an absence of monthly income, as well as an absence of fixed employment. A study carried out in Rio Grande do Sul9mentioned that this population is not in a position to contribute economically to society, which hinders the country's growth and on the contrary, this raises the costs of the health sector as a result of spending on treatment of addiction and comorbidities.
As for the religiousness belief, only three studies mentioned this data8 9 10, showing that the Protestant religion was the most self-reported, as in the present study. It is inferred that such information may be related to the belief professed by the therapeutic communities in which the participants are treated, so it cannot be said that these users practice their beliefs.
Regarding sociodemographic characteristics, it is clear that regardless of the region and country, the profile of users was maintained. This scenario points to people who suffer losses of various kinds. This is due to the fact that the abuse of drugs use brings harm not only in the social aspect, as frequently mentioned by authors in documents that mention public policies13.
In addition to understanding who the users are, based on their life context, identifying the profile of this population can facilitate the understanding of sociodemographic conditions and the social context where they are inserted, to think about implementing auspicious alternatives for rehabilitation, interfering in the planning of assistance and treatment outcome, which can contribute to their adherence9 14.
The summary chart 2, reveals that regarding the consumption of drugs, the comparison of the present study with other studies, demonstrated that none or few of them investigated the presence of family history for drug use, and / or the first drug to be used and / or the reason that led to consumption7 8 9 10 12.
Chart 2: Summary of the main results found among the studies available for consultation in the 2014-2018 period in the Scielo database.
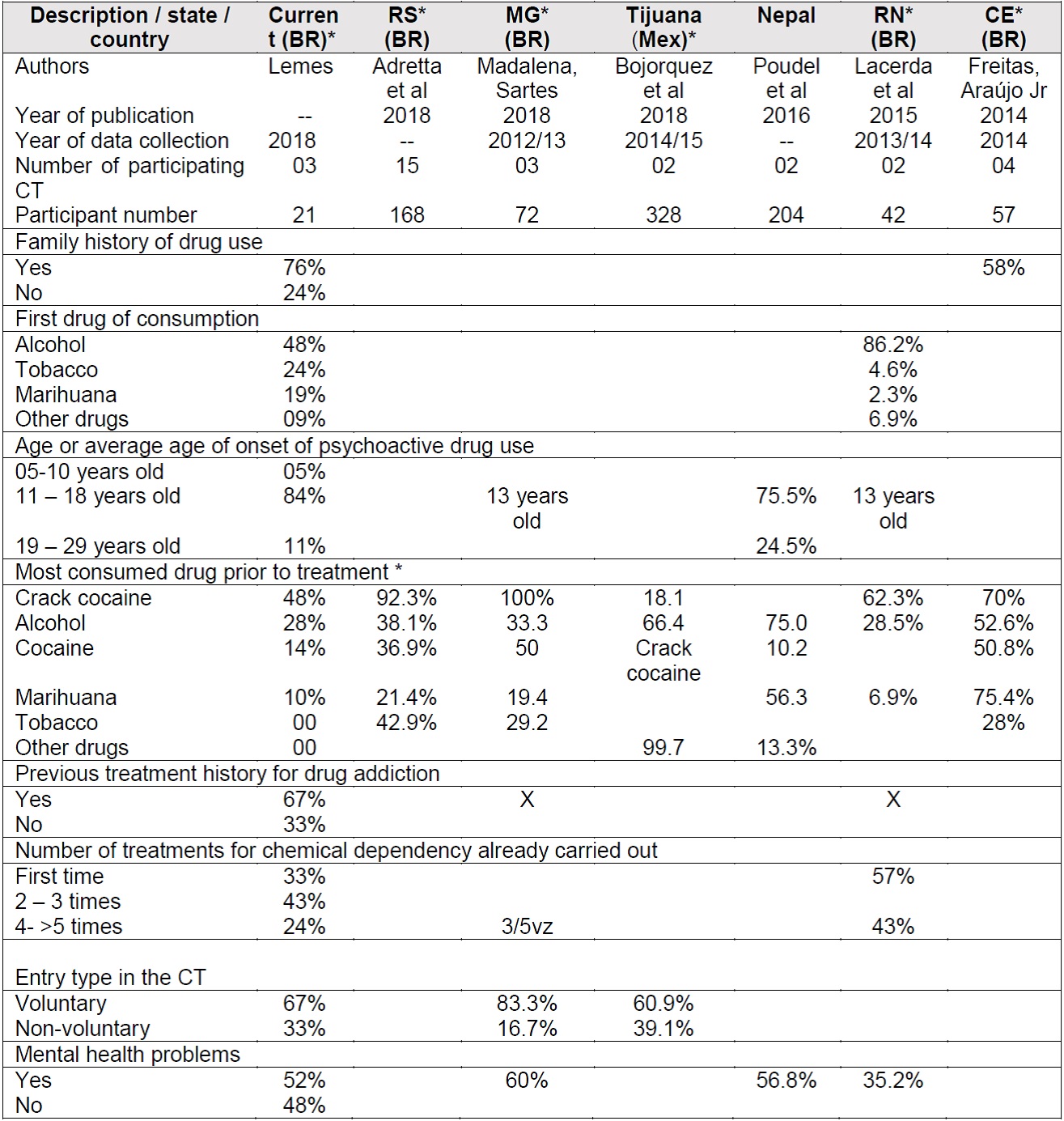
*Brazil (BR); Rio Grande do Sul (RS); Minas Gerais (MG); México (MEX); Rio Grande do Norte (RN); Ceará (CE).
In the present study, users reported the use of psychoactive drugs by a family member. Having a family member involved with drugs can predispose to an increase in consumption by other family members, which makes it an aggravating factor15 16. On the other hand, the family has also been considered as a protective factor against drug use, as long as it develops a role of monitoring its members, providing support, participating in collective activities and having a healthy daily life17 18.
Drug use in this research was motivated by peers, as well as this influence was present in a study conducted in northern Brazil, which considered that this initial consumption was due to the interaction of groups that people were part of, a linked to acceptance in social groups and in this way, apparently exercising a direct influence on the process of socio-cultural interaction between the individuals that make up a group17.
The early onset of drug use was common in this and other studies10 11. As reported by users of three therapeutic communities in Minas Gerais19(BR), where the first drug used was alcohol at 14.3 years old, followed by marijuana at 21.6 years old. The use of alcohol as the drug of first choice has also been reported among users of drug rehabilitation centers in Nepal12, followed by the use of marijuana (56.3%) and opioids (47.6%), with onset consumption between 15 and 19 years old (53.9%).
Alcohol was the first drug of choice present in this and other studies11 12 19. In Brazil, harmful alcohol consumption was registered with a higher prevalence in a quarter of the population20. Increasingly, research has reported the damage caused by its early onset, which suggests the need to review control, inspection, prevention and treatment15 18.
It can be seen that among users of therapeutic communities, crack cocaine was the drug that most contributed to their hospitalization, consequently contributing to chemical dependence, as observed in other studies7 8 9 10 11 12 16 17. This drug has been considered to have a high addictive power, being present among the population of greatest social vulnerability, as evidenced in this and in another study16. Most people who use crack cocaine have the desire and, a priori, put themselves on a voluntary basis to experience a treatment process, which can justify the demand of these users for treatment in these health services21.
The information presented so far, leads us to think that the lives of psychoactive drug users who frequent CT, regardless of the differences in the results presented by the set of research consulted in some aspects, show a similarity of individuals These are people who have a life history in a cascading effect of vulnerability, in relation to close contact with drug users or having users in their surroundings, the early consumption of alcohol or tobacco, a consumption that with age has been other drugs such as marijuana, cocaine and crack cocaine are added, leading to an end to chemical dependency.
As expected, users had a previous history of treating drug addiction, as well as multiple hospitalizations, in particular they resorted to the therapeutic community service to treat themselves, similar to what was found in other studies7 10 11.
It is noteworthy that CT is the treatment modality most sought after by users who have a disorder resulting from dependence on some psychoactive substance in Brazil and in other parts of the world. This demand is demarcated by the form of treatment that aims at coexistence for social reintegration and physical and psychological rehabilitation22, although not all have specialized professionals, and can still be answered by users' notes regarding the difficulty of access to treatment in public health services and their low quality and resolvability23.
The CT participating in this study did not have health professionals in their staff, so according to the records, they sought health support in services linked to RAPS, with emphasis on care in public hospitals and ESF. It cannot be said that this characteristic is being repeated in other therapeutic communities, due to the absence of this information among the national researches evaluated.
The guarantee of this service is based on the guidelines of the Brazilian health legislation24, providing public care by the Unified Health System (SUS), which is protected by the National Policy on Drugs, which describes the structure of access to health offered within the scope of the SUS by RAPS, such as the CAPS AD offer.
As in this study, the consequences arising from the consumption of psychoactive drugs were observed in other studies17 18 19, which highlighted physical and mental illnesses, learning difficulties, social losses, material losses, emotional losses, physical death and problems with justice, as the main consequences mentioned by their participants.
One of the highlights among the consequences found was the family conflict, which was also reported among users in Rio de Janeiro and Sao Paulo16, Mato Grosso13and Asia12. It is important to highlight that the existence of these family conflicts can be associated with loss of family contact, often caused by compulsive drug use16. Other researchers mention that the existence of these conflicts changes the consumption pattern among users, either increasing or restarting use, at the same time that it contributes to the beginning of consumption18.
Family problems end up contributing to the absence of family involvement in the treatment of the user, impairing adherence to the care and rehabilitation process, permeated by feelings of loneliness, abandonment and consequently social isolation. Authors point out that when the family adheres with the user to the proposed therapeutic plan to treat drug addiction, he is also respected in his pain, welcomed and treated, which contributes significantly to his improvement and the improvement of the relationship with his peers25.
As in other studies13 15 19, problems of an economic nature were raised as a negative consequence in the lives of their participants, which also corresponded to the one verified here. This is because the indiscriminate use of psychoactive drugs does not only cause losses of a family nature, also resulting in losses of a financial nature. These losses can contribute even more to the increase in violence, social vulnerability and crime, as pointed out by a research carried out in a CT in the interior of Minas Gerais19.
Another consequence seen among the participants in this study is the presence of a subsequent mental illness or concomitant with involvement with psychoactive drugs. The use of drugs alters the individual's organic conditions, contributing to his physical and mental disorder. Harmful drug use contributes to the presence of psychiatric comorbidities, highlighting anxiety, depression, schizophrenia, delusions or hallucinations, suicidal thoughts and attempted suicide7 9 10 11 12 14, as well as aggravating existing diseases, further damaging the health of these users and consequently their quality of life.
In this way, what is perceived is the need to offer a treatment related to mental health capable of meeting the needs not only focused on abstinence or reduction of consumption, but also the needs involving physical and psychic comorbidities.
The comparison between the studies allowed us to verify that regarding the treatment received, most users entered the therapeutic community willingly, as reported in México8and Porto Velho-BR26, which was similar to the data presented here, as well how the type of entry was directly associated with the way users considered the treatment of CT.
The fact that the participants consider the treatment received to be adequate is in line with what the authors describe that often these users resort to this service in search of finding an alternative housing that offers protection, security, and at the same time solidarity27.
Despite the criticisms suffered as a mental hospital model28, it is necessary to report, here that CTs need to be seen as one of the systems that welcome drug users within their peculiarities, and sought by most users as a treatment modality, as identified in the present study.
This welcoming can be seen among users who, after entering the CT, had better expectations to develop a new lifestyle and skills for coping with issues related to drug addiction29. The CT needs to be seen by the professionals who welcome these users, as a representative place for the rescue of citizenship, emancipator in search of a better future perspective30.
The communities participating in the study are of a religious nature and do not have a health or social assistance team to care for users, relying only on tutors and pastors, who are often ex-drug addicts. The absence of specialized support hinders the abstinence process expected by the CT, as part of the users in rehabilitation have a desire to use drugs7, which ends up compromising the treatment.
To manage this behavior of returning to drug use promoted by abstinence, many therapeutic communities need assistance from the local health service, such as basic health units and CAPS AD, in search of obtaining clinical and psychiatric medical care for their users, in addition to the service and reception of the entire multidisciplinary team available.
As limitations, stand out the same as some of the studies consulted, that is, the sample of therapeutic communities and the insufficient number of participating users to characterize a group of hospitalized people who consume psychoactive drugs, so there is no intention to generalize the findings. Given the relevance of the subject, it is suggested that further research be carried out to expand knowledge.
CONCLUSION
This study delimited the profile of users of three reference therapeutic communities for the interior of the Central-West region of Brazil, revealing a sociodemographic profile, consumption of psychoactive drugs, consequences of consumption and treatment received that follow in their general characteristics similar to those found in other national and international research, allowing to infer that the consumption of psychoactive drugs causes significant losses in the users' lives.
It should, be noted that the profile that this and other studies reveal is that of young adult users, already quite committed to their health and social insertion, leading to the question of what the future expectations will be in relation to the continuity of human societie as it has been known in the last decades and presupposes a great challenge for nursing.
Such concerns should sensitize the creators of public policies, to invest in the health care of this population, as well as encourage other researchers, to investigate in depth the motivations that are leading to uncontrolled consumption of psychoactive drugs, as this consumption has caused damage to all sectors of society.
In addition, these data can contribute to nursing practice, since they can subsidize health actions aimed at meeting the integral demands of users, improving the quality of care provided, and can contribute to the development of public policies and rehabilitation strategies that contribute to treatment adherence.
REFERENCIAS
1. Cui C, Noronha A, Warren KR, Koob GF, Sinha R, Thakkar M, et al. Brain pthways to recovery from alcohol dependence. Alcohol. 2015;49(5):435-52. [ Links ]
2. Dafny N, Rosenfeld GC. Chapter 33 -Neurobiology of Drugs of Abuse. Conn's Translational Neuroscience. 2017;715-22. [ Links ]
3. Lopes HP, Gonçalves AM. A política nacional de redução de danos: do paradigma da abstinência às ações de liberdade. Pesqui prát psicossociais. 2018; 13(1):1-15. [ Links ]
4. Ronzani TM, Mota DB, Costa P, Laport TJ. Redes de Atenção aos usuários de drogas: políticas e práticas. São Paulo: Cortez; 2015. 248 p. [ Links ]
5. Laurito JAS, Nascimento VF, Lemes AG. Proposta de instrumento para projeto terapêutico singular em saúde mental. Cadernos UniFOA. 2018;37:115-122. [ Links ]
6. Ayres M, Ayres DL, Santos AAS. BioEstat: aplicações estatísticas nas áreas das ciências bio-médicas. Versão 5.0; 2007. 380 p. [ Links ]
7. Freitas JAS, Araújo Junior CMP. Perfil de usuários das comunidades terapêuticas do município de Aracati. Socializando. 2014;1(2): 9-21. [ Links ]
8. Bojorquez I, Rodríguez D, Odgers O, Jaimes R. Factors associated with retention in Faith-based drug treatment centers in the Mexican-American border. Salud mental. 2018;41(4):169-77. [ Links ]
9. Madalena TS, Sartes LMA. Usuários de crack em tratamento em Comunidades Terapêuticas: perfil e prevalência. Arq Bras Psicol. 2018;70(1):21-36. [ Links ]
10. Andretta I, Limberger J, Schneider JA, Mello LTN. Sintomas de depressão, ansiedade e estresse em usuários de drogas em tratamento em comunidades terapêuticas. Psico-USF. 2018;23(2):361-73. [ Links ]
11. Lacerda BM, Pinto GMQV, Pinto SMQV, Salomão MAAO. Perfil de usuários de drogas em centros terapêuticos do estado do Rio Grande do Norte. Rev Ciênc Saúde Nova Esperança. 2015;13(1):54-65. [ Links ]
12. Poudel A, Sharma C, Gautam S, Poudel A. Psychosocial problems among individuals with substance use disorders in drug rehabilitation centers, Nepal. Subst abuse treat prev policy. 2016;11(28):1-10. [ Links ]
13. Lemes AG, Nascimento VF, Rocha EM, Moura AAMM, Luis MAV, Macedo JQ. Terapia Comunitária Integrativa como estratégia de enfrentameto às drogas entre internos de comunidades terapêuticas: pesquisa documental. SMAD, Rev eletrônica saúde mental álcool drog. 2017;13(2):101-108. [ Links ]
14. Raimundo MFRA, Pegoraro NPJ, Domingos JBC, Gonçalves AMS, Santos JAT, Pillon SC. Consumo de álcool no padrão binge e suas consequências em usuários de drogas em tratamento. Rev eletrônica Enferm. 2016;18:e1158. [ Links ]
15. Silva DLS, Torrezan MB, Costa JV, Garcia APRF, Toledo VP. Perfil sociodemográfico e epidemiológico dos usuários de um centro de atenção psicossocial álcool e drogas. Rev enferm atenção saúde. 2017;6(1):67-79. [ Links ]
16. Krawczyk N, Veloso Filho CL, Bastos FI. The interplay between drug-use behaviors, settings, and access to care: a qualitative study exploring attitudes and experiences of crack cocaine users in Rio de Janeiro and São Paulo, Brazil. Harm reduct j. 2015;12(24):1-12. [ Links ]
17. Lima DWC, Ferreira LA, Vieira AN, Azevedo LDS, Silva AP, Cunha BMC, et al. Ditos sobre o uso abusivo de álcool e outras drogas: significados e histórias de vida. SMAD, Rev eletrônica saúde mental álcool drog. 2018;14(3):151-58. [ Links ]
18. Barros BA, Lemes AG, Bauer TX, Moura AAM, Carrijo MVN, Siqueira MFC, et al. Desvelando o universo das drogas entre adolescentes. Interdisciplinar: Rev eletrônica da UNIVAR. 2016;15(1):189-94. [ Links ]
19. Singulane BAR, Silva NB, Sartes LMA. Histórico e Fatores associados à Criminalidade e Violência entre Dependentes de Crack. Psico USF. 2016;21(2):395-407. [ Links ]
20. Taylor B, Rehm J, Aburto JTC, Bejarano J, Cayetano C, Kerr-Correa F, et al. Alcohol, género, cultura y daños en las Américas: reporte final del estudio multicéntrico. Washington, D.C: OPS; 2007. 70 p. [ Links ]
21. Almeida RBF, Santos NTV, Brito AM, Silva KSB, Nappo SA. O tratamento da dependência na perspectiva das pessoas que fazem uso de crack. Interface. 2018; 22(66):745-56. [ Links ]
22. Perrone PAK. A comunidade terapêutica para recuperação da dependência do álcool e outras drogas no Brasil: mão ou contramão da reforma psiquiátrica? Ciênc Saúde Colet. 2014;19(2):569-80. [ Links ]
23. Ribeiro FML, Minayo MCS. Religious therapeutic communities in recovering drug users: the case of Manguinhos, state of Rio de Janeiro, Brazil. Interface comun Saúde educ. 2015;19(54):515-26. [ Links ]
24. Brasil. Portaria n. 3588, de 21 de dezembro de 2017. [Acesso em 09/07/2019]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2017/prt3588_22_12_2017.html [ Links ]
25. Sanches LR, Santos TGC, Gomes TB, Vecchia MD. Meanings of Family Support in the Treatment of Drug Dependence. Paidéia. 2018;28(e2824):1-8. [ Links ]
26. Felix Junior IJ, Calheiros PRV, Crispim PTB. Motivação para mudanças no uso de substancias entre usuários de drogas encaminhados pela justiça. Trends Psychol. 2018;26(3):1363-78. [ Links ]
27. Nascimento VF, Moll MF, Lemes AG, Cabral JF, Cardoso TP, Luis MAV. Percepción de las mujeres en situación de dependencia química dentro de Mato Grosso, Brasil. Cult cuid. 2017;21(48):33-42. [ Links ]
28. Pacheco AL, Scisleski A. Vivências em uma comunidade terapêutica. Rev Psicol Saúde. 2013;5(2):165-73. [ Links ]
29. Scaduto AA, Barbieri V, Santos MA. Adesão aos Princípios da Comunidade Terapêutica e Processo de Mudança ao Longo do Tratamento. Psicol ciênc prof. 2015;35(3):781-96. [ Links ]
30. Damas FB. Comunidades Terapêuticas no Brasil: expansão, institucionalização e relevância social. Rev Saúde Públ Santa Cat. 2013;6(1):50-65. [ Links ]
Received: July 12, 2019; Accepted: January 16, 2020











 text in
text in