Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO  Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.96 no.2 Madrid feb. 2004
| CLINICAL NOTES |
Recurrent Dieulafoy's disease with surgical management:
diagnosis by endoscopic ultrasonography
D. Martínez Ares, J. Souto Ruzo, J. Yáñez López, P. Alonso Aguirre, C. Gómez Mata2, L. Valbuena
Ruvira1 and J. L. Vázquez Iglesias
Service of Digestive Diseases, 1Pathology and 2General Surgery. Complejo Hospitalario Universitario Juan Canalejo.
A Coruña, Spain
ABSTRACT
Dieulafoy's disease is an uncommon but potentially significant cause of gastrointestinal bleeding caused by a large-caliber arterial vessel in the submucosa, which causes erosion and debilitation of the surrounding mucosa and may lead to massive gastrointestinal bleeding. Since endoscopy may prove insufficient, echoendoscopy may help in the diagnosis of this condition. Echoendoscopy may also help improve endoscopic management using mechanical techniques (hemoclips or band ligation) or a combination of thermal techniques and injection sclerotherapy, since this allows an accurate localization of the submucosal vessel.
We present a case illustrating this approach by endoscopic ultrasonography, and describe the morphological substrate of this condition.
Key words: Dieulafoy's disease. Endoscopic ultrasonography. Surgical management. Endoscopic management.
Martínez Ares D, Souto Ruzo J, Yáñez López J, Alonso Aguirre P, Gómez Mata C, Valbuena Ruvira L, Vázquez Iglesias JL. Recurrent Dieulafoy's disease with surgical management: diagnosis by endoscopic ultrasonography. Rev Esp Enferm Dig 2004; 96: 138-142.
Recibido: 23-04-03.
Aceptado: 04-09-03.
Correspondencia: David Martínez Ares. C/ Emilio González López, 11, 7º B. 15001 A Coruña. e-mail: dmartinez@sepd.es
INTRODUCTION
Dieulafoy's disease is an uncommon cause of gastrointestinal bleeding (1), which accounts for approximately 1% of all non-variceal upper gastrointestinal bleeding episodes (2). Most are cases of peptic ulcer (3). Nevertheless, the actual incidence of this disease is not accurately known, since misdiagnosis may occur in some cases (4). Most of these lesions are located in the stomach (1), although they may also appear in other parts of the gastrointestinal tract such as the duodenum, jejunum or rectum. Although fairly uncommon, this entity may be potentially severe and even have a fatal outcome.
It is also known as "caliber-persistent artery", and consists of a large caliber artery which protrudes through the submucosa and contacts the mucosa (5). Minute ruptures in this usually atrophied mucosa (6) lead to rupture of the vessel and cause subsequent bleeding. This bleeding may be recurrent or single. Diagnosis is difficult when no active bleeding is observed, since no apparent lesion in the mucosa can be seen (5). Initial treatment usually consists of endoscopic management: injection techniques combined with another modality of endoscopic hemostasis: thermocoagulation or mechanical methods (hemoclipping or band ligation). If the bleeding cannot be stopped by these techniques, a surgical resection of the affected segment is generally indicated.CASE REPORT
We present the case of a 39-year-old male with a history of two previous hospital admissions 9 and 4 years before, both for upper gastrointestinal bleeding secondary to Dieulafoy's disease, one of which required surgery. The patient did not report previous alcohol abuse, smoking or other unhealthy habits. There was no history of NSAID or other drugs ingestion.
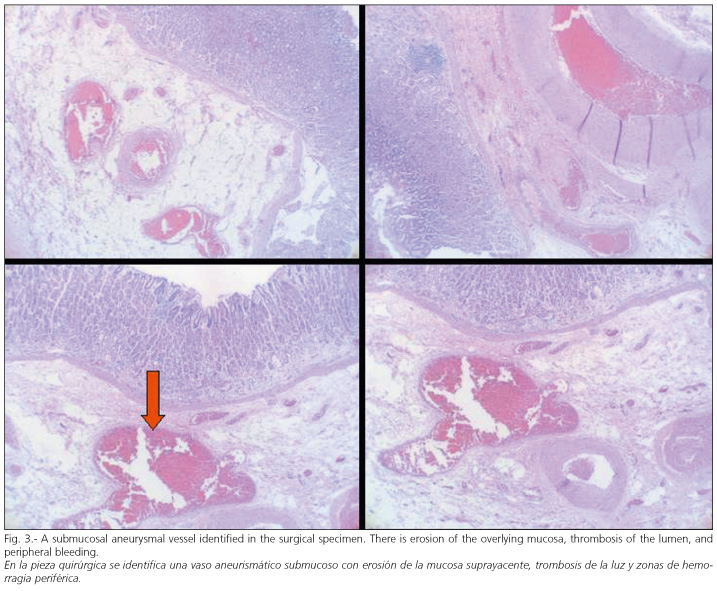
The patient presented with anemia and melenic stools at admission. Biochemistry revealed severe anemia with a hematocrit of 25% (38-50) and hemoglobin 7.5 g/dl (13.5-18). An emergency upper endoscopy showed a protruding lesion with preserved mucosa at the junction of the body and fundus, and no active bleeding at that time, a picture that apparently corresponded to the Dieulafoy's disease (Fig. 1). Endoscopic ultrasonography revealed the presence of a hypoechogenic tubular structure which corresponded to an arterial vessel with an abnormally large caliber and an ulceration in its apex in contact with the mucosa, which suggested the diagnose of Dieulafoy's disease (Fig. 2). An endoscopic sclerotherapy was performed and two hemoclips were placed on the lesion. Recurrent bleeding with hematemesis, rectal bleeding and hemodynamic instability developed in the days following this treatment, requiring the transfusion of six concentrates of red blood cells. Surgical management was then decided upon, and consisted of partial gastrectomy. The pathological study revealed the presence of an aberrant dilated submucosal vessel, erosion of the overlying mucosa, luminal thrombosis, and areas of peripheral bleed-ing (Fig. 3). The subsequent recovery of the patient was uneventful, and bleeding has not recurred.
DISCUSSION
The diagnosis of Dieulafoy's disease is not always easy, especially when no active bleeding is observed during endoscopy. For this reason, repeat examinations may be required. Norton et al. published in 1999 a series of 90 cases in which a mean of 1.9 explorations were required before a diagnosis was reached (7). In our study, the diagnosis appeared in the form of a nodular lesion with active bleeding, suggestive of Dieulafoy's lesion. Nevertheless, this entity may have a presentation not allowing diagnosis when there is no active bleeding, or it may have a form similar to that of gastrointestinal varices (8). When the diagnosis is difficult to reach, endoscopic ultrasonography and Doppler imaging may help locate the large-caliber arterial vessel in contact with the mucosa, which is characteristic of this lesion (9,10). In our case, this is illustrated by the images provided by echoendoscopy.
The initial management of Dieulafoy's disease should be endoscopic. Hemostasis may be equally achieved by mechanical and thermal methods, whether these are combined with injection sclerotherapy or not (1). However, endoscopic sclerosis cannot be considered the only therapeutic approach acceptable, since it does not offer the efficacy provided by the combination of sclerosis and thermal methods (2), or by mechanical treatments (11). As for mechanical options, both elastic band ligation (12,13) and hemoclipping (11,14) have proven to be safe, efficient and cost-effective techniques. These techniques may be combined with Doppler imaging and ultrasonography in order to better locate the vessel, thus allowing better outcomes especially in cases where the lesion is not apparent (15,16). In our case, endoscopic ultrasonography confirmed the diagnosis and was of help for the placement of two hemoclips. However, despite an apparently correct placement of hemoclips and the performance of an endoscopic sclerosing of the lesion, recurrent bleeding developed, and so surgical management was performed as the definitive solution.In conclusion, Dieulafoy's disease is an uncommon condition that is sometimes difficult to diagnose. In these cases, endoscopic ultrasonography may be helpful both to reach a diagnosis and perform a more precise endoscopic approach. Surgical treatment is generally the option of choice when endoscopy is unsuccessful and when there is recurrent bleeding.
REFERENCES
1. Mumtaz R, Shaukat M, Ramírez FC. Outcomes of endoscopic treatment of gastroduodenal Dieulafoy's lesion with rubber band ligation and thermal/injection therapy. J Clin Gastroenterol 2003; 36 (4): 310-4. [ Links ]
2. Kasapidis P, Georgopoulos P, Delis V, Balatsos V, Konstantinidis A, Skandalis N. Endoscopic management and long-term follow-up of Dieulafoy's lesions in the upper GI tract. Gastrointest Endosc 2002; 55 (4): 527-31. [ Links ]
3. Palmer KR. Ulcers and nonvariceal bleeding. Endoscopy 2000; 32 (2): 118-23. [ Links ]
4. Schmulewitz N, Baillie J. Dieulafoy lesions: a review of 6 years of experience at a tertiary referral center. Am J Gastroenterol 2001; 96 (6): 1688-94. [ Links ]
5. Vázquez Iglesias, JL. Alteraciones Vasculares. En: Endoscopia Digestiva Alta. Volumen I. Galcia Editorial, SA, 1992: 228-9. [ Links ]
6. Owaki T, Kusano C, Ojiro M, Aikou T. Massive bleeding from Dieulafoy's lesion of the small intestine in a child - therapy for the bleeding from gastrointestinal tract out of endoscopic observation. Dig Surg 2002; 19 (4): 321-4. [ Links ]
7. Norton ID, Petersen BT, Sorbi D, Balm RK, Alexander GL, Gostout CJ. Management and long-term prognosis of Dieulafoy lesion. Gastrointest Endosc 1999; 50 (6): 762-7. [ Links ]
8. Pohle T, Helleberg M, Menzel J, Diallo R, Vestring T, Senninger N, et al. An extraordinary Dieulafoy's lesion presenting as varices of the gastric fundus. Gastrointest Endosc 2001; 54 (6): 776-9. [ Links ]
9. Fockens P, Meenan J, van Dullemen HM, Bolwerk CJ, Tytgat GN. Dieulafoy's disease: endosonographic detection and endosonography-guided treatment. Gastrointest Endosc 1996; 44 (4): 437-42. [ Links ] 10. Nesje LB, Skarstein A, Matre K, Myking AO, Odegaard S. Dieulafoy's vascular malformation: role of endoscopic ultrasonography in therapeutic decision-making. Scand J Gastroenterol 1998; 33 (1): 104-8. [ Links ]
11. Chung IK, Kim EJ, Lee MS, Kim HS, Park SH, Lee MH, et al. Bleeding Dieulafoy's lesions and the choice of endoscopic method: comparing the hemostatic efficacy of mechanical and injection methods. Gastrointest Endosc 2000; 52 (6): 721-4. [ Links ] 12. Matsui S, Kamisako T, Kudo M, Inoue R. Endoscopic band ligation for control of nonvariceal upper GI hemorrhage: comparison with bipolar electrocoagulation. Gastrointest Endosc 2002; 55 (2): 214-8. [ Links ]
13. Nikolaidis N, Zezos P, Giouleme O, Budas K, Marakis G, Paroutoglou G, et al. Endoscopic band ligation of Dieulafoy-like lesions in the upper gastrointestinal tract. Endoscopy 2001; 33 (9): 754-60. [ Links ]
14. Lee YJ, Oh JM, Park SE, Park JH. Successful treatment of a gastric Dieulafoy's lesion with a hemoclip in a newborn infant. Gastrointest Endosc 2003; 57 (3): 435-6. [ Links ]
15. Folvik G, Nesje LB, Berstad A, Odegaard S. Endosonography-guided endoscopic band ligation of Dieulafoy's malformation: a case report. Endoscopy 2001; 33 (7): 636-8. [ Links ]
16. Ribeiro A, Vázquez-Sequeiros E, Wiersema MJ. Doppler EUS-guided treatment of gastric Dieulafoy's lesion. Gastrointest Endosc 2001; 53 (7): 807-9. [ Links ]











 texto en
texto en