Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 no.10 Madrid oct. 2010
LETTERS TO THE EDITOR
Concomitant life threatening lesions in a cirrhotic patient: the value of endoscopic treatment
Lesiones concomitantes que ponen en peligro la vida en un paciente cirrótico: valor del tratamiento endoscópico
Key words: Histoacryl. Rectal varix.
Dear Editor,
In about 20 to 30% of the patients there is more than one lesion responsible for a gastrointestinal haemorrhage. Bleeding from rectal varices is present in 1-8% of cirrhotic patients. The histoacryl is a synthetic tissue adhesive that has been applied with success in the treatment of some particularly digestive haemorrhagic cases (gastric, duodenal or rectal varices). There have also been referred complications with histoacryl use, some of which, very serious and responsible for the patient's death (distance material embolization, abscess, strokes, haemorrhage by the injection histoacryl scar).
Case report
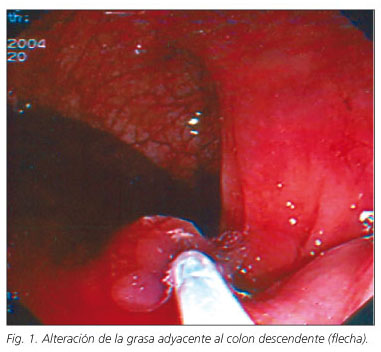
A 39-year-old man, with liver cirrhosis had two episodes of massive gastrointestinal bleeding with hypovolemic shock during the same hospitalization: first for gastric ulcer (Forrest IIa) treated with injection sclerotherapy (epinephrine and absolute alcohol); the second which occurred 24 hours later, was due to rectal varices and was treated with histoacryl (it was injected a total of 1.4 ml of the solution histoacryl mixed with lipiodol - 0.7:0.7) (Fig. 1). Both treatments achieved definite haemostasis in the acute phase. One week later, he presented with high fever, without other symptoms. The study demonstrated a sepsis by Pseudomonas aeruginosa, associated with a rectal abscess that responded to a large spectrum antibiotic and endoscopic drainage.
Discussion
The literature describes rates from 43 to 78% of rectal varices in patients with liver cirrhosis and portal hypertension (1). There are consensual treatments for the endoscopic management of ulcers and oesophageal varices (2). Some types of treatments have been referred to bleeding rectal varices (sclerotherapy, histoacryl, band ligation, double ballon-occluded embolotherapy, gel foam embolization, inferior mesenteric vein ligation, suture ligation, colectomy, surgical portosystemic shunt, transjugular intrahepatic portosystemic shunt (TIPS), intravenous infusion of vasoactive drugs); but because of the rarity of this entity, randomised controlled trials are missing, which compared the types of therapeutic modalities, to evaluate the most efficacious (1). But there are similarities demonstrating that conservative managements are associated with minor morbidity and mortality (3). There is the risk of distant embolization caused by the flow of a significant volume of histoacryl into systemic circulation. The bacteriostatic and haemostatic histoacryl activity offers an ideal superficie for bacteria colonization, which in this case was helped by the local conditions. In this case the fact of there not being any distance embolization along with the abcess being in the puncture place, allowed an easy treatment with good results.
E. Cancela, P. Ministro, P. Peixoto, A. Sadio, A. Castanheira, A. Silva, A. Caldas
Gastroenterology Department, São Teotónio Hospital, Viseu, Portugal
References
1. Chen WC, Hou MC, Lin HC, et al. An endoscopic injection with N-butyl-2-cyanoacrylate used for colonic variceal bleeding: a case report and review of the literature. Am J Gastroenterol 2000; 95: 540-2. [ Links ]
2. Wahl P, Lammer F, Conen D et al. Septic complications after injection of N-butyl-2-cyanoacrylate : report of two cases and review. Gastrointest Endosc 2004; 59: 911-6. [ Links ]
3. Shudo R, Yazaki Y, Sakurai S, et al. Combined endoscopic variceal ligation and sclerotherapy for bleeding rectal varices associated with primary biliary cirrhosis: a case showing a long-lasting favorable response. Gastrointest Endosc 2001; 53: 661-5. [ Links ]