Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 no.6 Madrid jun. 2014
LETTERS TO THE EDITOR
Coloduodenal fistula in a patient with Crohn's disease
Fístula coloduodenal en un paciente con enfermedad de Crohn
Key words: Crohn's disease. Coloduodenal fistula.
Dear Editor,
Coloduodenal benign fistulas are less common than the malignant counterpart (1). The most prevalent benign cause is the Crohn's disease, which is commonly related to internal fistulas (between 5 and 10 % of the patients), with a challenging management for surgeons and gastroenterologists (2).
Case report
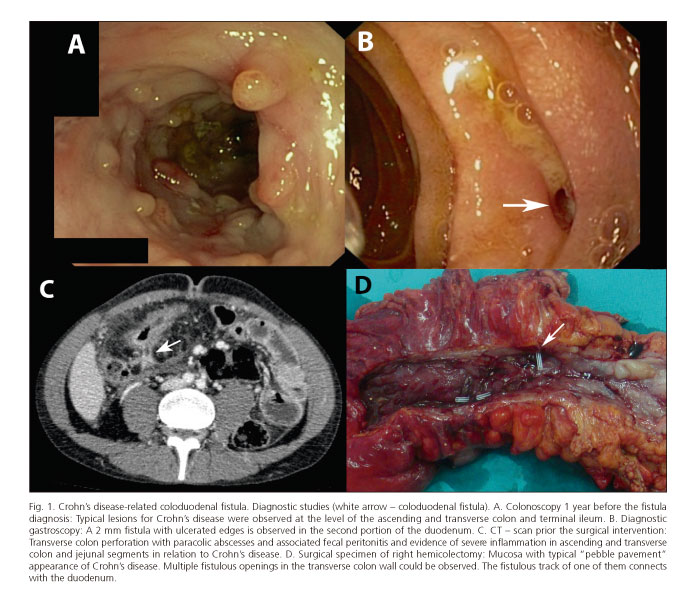
We report a case of a 25-years-old male with a 13-years history of Crohn's disease (Fig. 1A). He had been initially treated with corticoids and maintenance treatment with mesalazine and azathioprine, with no further flare-ups. Three months prior the episode of interest, he referred a colic mesogastric pain, bloody stools with mucus and weight loss (6 kg). Induction doses of infliximab were added to the treatment with no improvement and he required a hospital admission for intravenous corticoid treatment. The GI series showed a coloduodenal fistula that was confirmed endoscopically (Fig. 1B). He was discharged with improvement, continuing the infliximab therapy.
A month later, the patient presented a feverish sensation, hypotension and stabbing, progressive and diffuse abdominal pain. Physical examination showed a diffuse abdominal tenderness with peritoneal irritation. CT-scan showed transverse colon perforation and multiple paracolic abscesses (Fig. 1C).
Urgent laparotomy revealed a coloduodenal fistula and a ruptured peripancreatic abscess with acute peritonitis. A fistulectomy with EndoGIA, right hemicolectomy (Fig. 1D) with latero-lateral ileocolic anastomosis and proximal diverting ileostomy were performed.
The postoperative period was uneventful. He continued azathioprine treatment and three months later, the ileostomy was closed without complications. Three years later, the patient remains stable, without flare-ups.
Discussion
Crohn's disease is the most common benign cause (1) for coloduodenal fistula and even though it is extremely rare, with only 53 cases reported so far (3). The fistula typically involves the proximal colon and the second or third part of duodenum due to their proximity (4) and the diagnosis is reached by imaging studies including upper and lower gastrointestinal series, CT-scan and endoscopy (3).
The symptoms are caused mainly by the passage of hydrochloric acid and bile salts to the colon, resulting in diarrhoea that is aggravated by bacterial overgrowth and mechanical bypass (4). The most important features are diarrhoea, weight loss and fecal vomits (3). Reflux of stools in the duodenum leads to jejunitis (with decreased iron, folic acid and glucose absorption) and alteration of the intestinal flora (causing vitamin B12 malabsorption) (1).
In Crohn's disease, the medical treatment, whenever possible, should be preferred as it does not eradicate the disease. In cases of coloduodenal fistula, there are only single cases effectively managed conservatively (with tacrolimus, metronidazole or 5-ASA) (5), mainly extrapolating the results from other Crohn's-related fistulas. A stent placement has been recently reported (6), but it provides only mechanical barrier, and therefore we do not recommend it for patient in flare-up. In symptomatic fistulas, especially in those with high debit or fecal vomiting, it is likely that patients require an emergency or prompt elective surgery, in order to eliminate the fistula tract and part of the affected bowel.
In our patient, partial control was achieved only with intravenous corticoids and even though the patient required an urgent surgery. Therefore, patients not responding to the anti-TNF treatment could be candidates for prompt surgical evaluation, as the symptomatic control seems to be achievable only with far more aggressive treatments and cannot be maintained overt time.
Tihomir Georgiev-Hristov, Fernando Tone-Villanueva, Jacobo Trébol,
Susana Ayuela-García, José Tomas Castell-Gómez and Damián García-Olmo
Colorectal Surgery Unit. Hospital Universitario La Paz. Madrid, Spain
References
1. Xenos E, Halverson J. Duodenocolic fistula: Case report and review of the literature. J Postgrad Med 1999;45:87-9. [ Links ]
2. Levy C, Tremaine WJ. Management of internal fistulas in Crohn's disease. Inflamm Bowel Dis 2002;8:106-11. [ Links ]
3. Pichney LS, Fantry GT, Graham SM. Gastrocolic and duodenocolic fistulas in crohns-disease. J Clin Gastroenterol 1992;15:205-11. [ Links ]
4. El-Hajj II, Abdul-Baki H, El-Zahabi LM, Barada KA. Primary coloduodenal fistula in a patient with Crohn's disease. Dig Dis Sci 2007;52:59-63. [ Links ]
5. Fukuda A, Nakase H, Seno H, Nabeshima M, Sawada M, Chiba T. Refractory enterovesical and duodenocolic fistulas in Crohn's disease successfully managed with tacrolimus. J Gastroenterol 2005;40:433-5. [ Links ]
6. Kulkarni S, Hay C, Moss JG, Chandramohan S. Covered stent placement for duodenocolic fistula: A novel use of the "body floss" technique. J Vasc Interv Radiol 2011;22:729-30. [ Links ]