Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 no.9 Madrid sep. 2015
PICTURES IN DIGESTIVE PATHOLOGY
Jejunal plasmablastic lymphoma presenting as obscure overt gastrointestinal bleeding: Diagnosis by wireless capsule endoscopy
Pedro Magalhães-Costa, Miguel Bispo, Leopoldo Matos and Cristina Chagas
Gastroenterology Department. Hospital Egas Moniz. Centro Hospitalar Lisboa Ocidental. Lisboa, Portugal
Case report
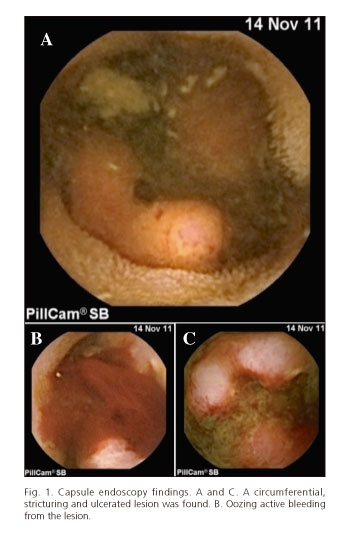
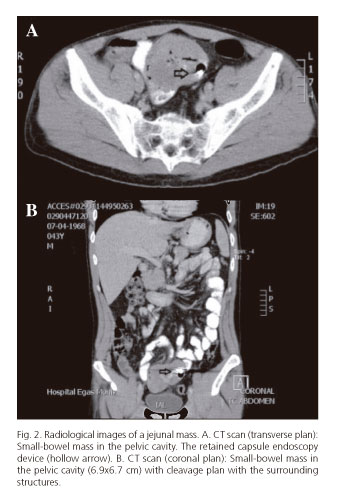
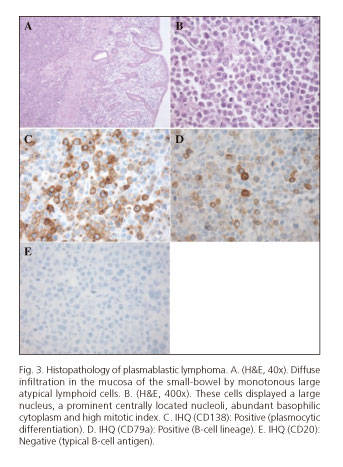
A 43 year-old male, diagnosed with acquired immune deficiency syndrome (under highly active antiretroviral therapy), presented with intermittent and recurrent melena. Physical examination was unremarkable. Labs revealed a severe microcytic anemia -serum hemoglobin (Hb) = 5.1 g/dL. Upper gastrointestinal endoscopy and ileocolonoscopy disregarded any potentially bleeding lesion. In the ward the patient kept the clinical picture, thus a wireless capsule endoscopy (WCE) was performed. The examiner noted in the mid-jejunum, a circumferential, stricturing and ulcerated lesion (Fig. 1A and C), with active oozing bleeding (Fig. 1B). An abdomino-pelvic computed tomography (CT) (Fig. 2A and B) scan revealed a small-bowel mass in the pelvic cavity. Also, a round and hyperintense image with many artefactual effects associated with the previously described mass was noted (the retained WCE device). The patient developed severe obstructive symptoms and an urgent surgical approach was deemed necessary. The resected specimen consisted of a 16 cm long segment of jejunum centered by a neoplastic mass, stricturing and ulcerated with 8 cm of larger longitudinal axis. Mesenteric ganglia were not committed and the surgical margins were free (R0 resection). Microscopy (Fig. 3A-E) visualized a diffuse lymphoma with large cell nucleus. The immunohistochemistry stain (IHQ) profile was positive for (cluster of differentiation) CD138 and CD79a; negative for CD30, CD20, CD19, CD10, (B-cell lymphoma) BCL2, BCL6, anaplastic lymphoma kinase (ALK), CD3, EMA (MUC1): Epithelial membrane antigen (AE1AE3) and EMA. On the basis of these morphologic and IHQ characteristics, the pathological diagnosis of plasmablastic lymphoma was made. The patient received 6 cycles of cyclophosphamide, doxorubicin, vincristine and prednisolone (CHOP) and, after 32 months of follow-up, his disease is in remission.
Discussion
There are few case reports of plasmablastic lymphoma (PBL) which had occurred in extra-oral locations like the small-bowel (1-3). Although PBL is usually typified as being an high-grade malignant lymphoma and known by their diffuse infiltrative growth, high mitotic rate and a dismal prognosis, in this case, an appropriate multidisciplinary approach allowed to an early diagnosis and subsequent treatment of the neoplasm.
Acknowledgments
Presented as a poster at RICE 2013 (XI Reunión Ibérica de Cápsula Endoscópic), 12 January 2013, Valencia, Spain.
References
1. Cha JM, Lee J Il, Joo KR, Jung SW, Shin HP, Lee JJ, et al. A case report with plasmablastic lymphoma of the jejunum. J Korean Med Sci 2010;25:496-500. [ Links ]
2. Bahari A, Jahantigh M, Mashhadi A, Bari Z, Bari A. Plasmablastic lymphoma presenting as small intestinal polyposis: A case-report. Iran Red Crescent Med J 2012;14:669-75. [ Links ]
3. Wang H-W, Yang W, Sun J-Z, Lu J-Y, Li M, Sun L. Plasmablastic lymphoma of the small intestine: Case report and literature review. World J Gastroenterol. 2012;18:6677-81. [ Links ]