Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.12 Madrid dic. 2016
https://dx.doi.org/10.17235/reed.2016.3749/2015
Study of the expression of cathepsins in histological material from pancreatic lesions
Juan Martínez1, José Ramón Aparicio1, Gloria Peiró2, Antonio Cabezas2, Manuela Roger1, Francisco Ruíz1, Luis Compañy1 and Juan Antonio Casellas1
Departments of 1Digestive Endoscopy and 2Anatomic Pathology. Hospital General Universitario de Alicante. Alicante, Spain
This study has been funded by Fundación Navarro Trípodi.
ABSTRACT
Background and aims: To assess the expression levels of cathepsins in malignant and premalignant lesions.
Methods: We retrospectively included patients who underwent pancreatic surgery on pancreatic solid or cystic masses. The expression of cathepsin H, L, B and S was determined in both types of samples. Lesions were divided into three categories: malignant (pancreatic adenocarcinoma and malignant mucinous neoplasms), premalignant (mucinous neoplasms) and benign (other lesions).
Results: Thirty-one surgical resection samples were studied. The expression of cathepsins was significantly higher in malignant lesions than in premalignant and benign lesions (H 75%, 27%, 37% p = 0.05; L 92%, 36%, 37% p = 0.011; B 83%, 36%, 62% p = 0.069; S 92%, 36%, 25% p = 0.004, respectively).
Conclusions: Cathepsins are overexpressed in histological samples of malignant lesions compared to premalignant and benign lesions. However, the expression of cathepsins is similar in both premalignant and benign lesions.
Key words: Cathepsins. Pancreatic adenocarcinoma. Pancreatic mucinous neoplasms.
Introducción
Pancreatic ductal adenocarcinoma (PDAC) is the most lethal common cancer as it is usually diagnosed at an advanced stage (1). As seen in other tumors, this neoplasm progresses from a few initially atypical, benign intraepithelial lesions (2). On the other hand, other initially benign pancreatic tumors such as the mucinous cystic neoplasms (MCNs) and the intraductal papillary mucinous neoplasms (IPMNs) are potentially malignant lesions since they can progress to PDAC (3). Over the last few years, pre-operative diagnosis of these neoplasms has clearly improved thanks to endoscopic ultrasound (EUS) and the possibility of obtaining cytology samples.
The mechanisms of tissue aggression of a malignant tumor are quite diverse. The tumor may grow, invade or distantly metastasize due to the interaction with its microenvironment (4). Several protease families are involved in this process during carcinogenesis (5). One of these families is the cathepsin family. These proteases are lysosome enzymes that degrade proteins in the acidic environment of the lysosomes. They play key roles in different physiological processes (5-8). Cathepsins are encoded by several genes in the genome (cathepsin B, C, D, F, H, K, L, O, S, V, W, X/Z). By targeting the tumor cells, and specifically on the microenvironment, cathepsins play a key role in mitogenic activity, the degradation of the cellular matrix and the decrease of the antitumor immune response. Thus, tumor induction, growth, invasion and progression processes are allowed to progress (4,9-16). They also intervene in angiogenesis, apoptosis and the development of metastasis (4,5,10-12,14,16-18). Some of these cathepsins play an important oncogenic role in PDAC (14-16,19-21). Several experimental and human studies have shown expression of different cathepsins in tumor cells (22-30) as well as in serum and in pancreatic juice of patients with PDAC (31-35). The role of some cathepsins, especially H, L, B and S, has been studied in the development of cancer and their utility as prognostic markers has been assessed in different tumors although the results are controversial (22,24,25,27,28,31). Some cathepsins are not expressed in normal pancreatic tissue but they are in lesions considered as premalignant such as pancreatic intraepithelial neoplasias (PanINs) and in almost every adenocarcinoma. That is why they would be quite important as an early biomarker of this neoplasia (28-30,36). Unfortunately, some studies have shown expression of cathepsins in pancreatic inflammatory pathologies, so their role in the diagnosis of PDAC would be less specific (26-28). On the other hand, there are not so many studies of the expression and the role of cathepsins in other premalignant lesions such as the MCNs and the IPMNs. Moreover, their results are contradictory (27,36).
Therefore, cathepsins are expressed in pancreatic adenocarcinoma as well as in premalignant lesions (PanINs) with low or high grade dysplasia. Moreover, they may have certain prognosis value. However, we do not know exactly if cathepsins are expressed in other premalignant lesions such as MCNs and IPMNs as well as in patients with inflammatory diseases that are potentially malignant such as chronic pancreatitis. We aim to assess the expression levels of cathepsins in malignant and premalignant lesions.
Methods
Patients
The study was designed as a case-control study. We included patients who underwent pancreatic surgery. Diagnosis was made from the pathological specimens.
Determination of the expression of cathepsins was performed in histological material of the surgical specimen. The lesions were divided into three categories: malignant (PDAC and malignant mucinous neoplasms), premalignant (mucinous neoplasms: MCN andd IPMN) and benign (the remaining lesions). The study was approved by the local Ethics Committee.
Determination of the expression of cathepsins
Material selection
All the histological preparations were examined and the most representative areas of the lesion were located in order to later perform the immunohistochemical study. Tissue microarrays (TMA) including two tissue punches of 1 mm of representative tissue of the pancreatic lesion were prepared. In addition, a TMA including normal and tumoral tissue from other organs, including the pancreas, were also prepared, and they were used to optimize (concentrations and adequate incubation time) the use of the commercial antibodies (Ab) (case-control TMA). Another three TMAs were prepared with the cases included in the study.
Immunohistochemical study
Optimization of commercial, primary Ab
The following commercially available antibodies were used in the study: mouse cathepsin H antibody (clone: Pol Goat IgG; dilution 1:80; supplier R&D; pretreatment: citrate buffer pH9; incubation 10 min, RT; method EnVisionFLEX); antihuman cathepsin L antibody (clone: Pol Goat IgG; dilution 1:80; supplier R&D; pretreatment: citrate buffer pH9; incubation 10 min, RT; method EnVisionFLEX); human cathepsin B biotinylated antibody (clone: Pol Goat IgG; dilution 1:40; supplier R&D; pretreatment: citrate buffer pH9; incubation 30 min, RT; method Streptavidin-HRP); human cathepsin S biotinylated antibody (clone: Pol Goat IgG; dilution 1:20; supplier R&D; pretreatment: citrate buffer pH9; incubation 30 min, RT; method Streptavidin-HRP). In the case of the primary Ab of cathepsins H and L, we applied a secondary Ab (polyclonal rabbit anti-goat/HRP; DakoCytomation) at 1:80 concentration during 10 minutes.
Immunohistochemical method and evaluation of the results
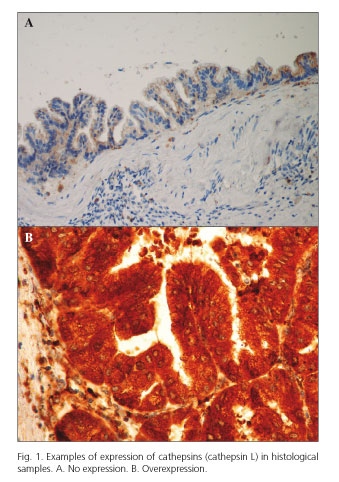
Immunohistochemical studies were performed with four-micron sections of the formalin-fixed and paraffin-embedded tissue of the TMAs with a staining system (DakoCytomation). The evaluation of the results of expression (cytoplasmic) was semi-quantitative according to the percentage (0-100%) of neoplastic epithelial cells and the staining intensity (0, 1+, 2+, 3+) of all the cathepsins (H, L, B and S). Staining intensity scores 0-1+ were considered as no expression and a score of 2+-3+ was considered as expression/overexpression (Fig. 1).
Statistical analysis
All the variables were collected in a spreadsheet designed for the purpose. To describe alterations in all clinical, histological and immunohistochemical variables, we used the relative frequency expressed as a percentage for the qualitative variables and the mean and standard deviation or median and the 25 and 75 percentiles according to the distribution type (parametric or non-parametric) for the quantitative variables. We used the Chi-squared test and Fisher's exact test to study the correlation between the immunohistochemical data and the clinical-pathological factors when applicable. The statistical significance cut-off was p < 0.05.
Results
Thirty-one patients were included in the study. The expression of cathepsins in the material obtained after surgical resection of pancreatic lesions was determined in all specimens. Table I shows the characteristics of patients.
Expression of cathepsins in histological material
The final diagnosis of these lesions was different, although most of them were identified as adenocarcinoma. Twelve lesions were considered as malignant, 11 as potentially malignant and 8 as benign (Table I). The location of the lesion in cases that were different from a chronic pancreatitis was as follows: 20 were located in the head of the pancreas, 2 in the body and 3 in the tail. The relationship between the expression of cathepsins and the malignancy of the lesions with histological material is shown in table II. Seventy-five percent of the malignant lesions expressed cathepsin H, whereas expression was detected in only 27% of premalignant lesions and in 37% of benign lesions (p = 0.057). The expression of cathepsin L was detected in 92% of the malignant lesions and only in 36% and 37% of premalignant and benign lesions, respectively (p = 0.011). The expression of cathepsin B was detected in 83% of the malignant lesions, 36% of premalignant and 62% of the benign lesions (p = 0.069). Finally, 92% of the malignant lesions expressed cathepsin S, as compared to 36% of the premalignant and 25% of the benign lesions (p = 0.004).
It is important to mention that the separate analysis of the three patients with malignant IPMN showed expression of all the cathepsins in every lesion. However, expression of cathepsins in the group of patients with premalignant lesions was low both in patients with IPMN and in the three patients with MCN as shown in table II.
Discussion
PDAC is a disease with a poor prognosis because it is often diagnosed at an advanced stage. Several imaging techniques have been used to improve early detection of this tumor. Over the last few years the determination of biomarkers thought to play a role in PDAC oncogenesis has been added to the conventional cytological techniques usually performed (4). One of these aspects is the expression of certain proteases such as the cathepsins (5). This family of proteases has been involved in the growth and invasion processes of some tumors such as PDAC (5-8). The expression of some cathepsins has been detected in both experimental (22,29,30) and human material ex vivo studies (24-28,37). In our study, the expression of cathepsin B in the tissue of patients with PDAC has been detected in 83% of cases. This data is in accordance with other studies (24,25,27) based in similar material. We also detected the expression of cathepsins S, L and H; the first two were expressed at a higher level than the other types.
With regard to early diagnosis of PDAC, a useful technique must be quite sensitive and specific, and it must avoid false positive malignant cases given the aggressiveness of this treatment. For this reason, we included patients with chronic pancreatitis or another pancreatic benign pathology in the material from the surgical specimens. In these lesions, the expression of cathepsins H, L, B and S is significantly lower (or tending towards statistical significance) than the expression described in patients with PDAC, although this expression ranged between 25 and 62% depending on the cathepsin type. The expression of cathepsins in pancreatic benign pathology has also been described by other studies (26,28), so its value in the diagnosis of PDAC is again restricted.
Due to the poor effectiveness of the indicated treatments for PDAC and its poor prognosis, prevention becomes a relevant aspect. Currently, two types of lesions have been identified as precursors of this tumor. One is the pancreatic intraepithelial neoplasm (PanIN) that cannot be detected by imaging techniques at the present time (2). Expression of cathepsins has been also described in this lesion (22,28-30,38). The other premalignant lesions are the mucinous tumors, both MCN and IPMN. Fortunately, these lesions can be detected by imaging techniques even when they are small, especially by EUS. The premalignant potential of the MCNs and the IPMNs that affect the main pancreatic duct is high, thus they must be surgically resected. However, the morbidity associated with pancreatic surgery is not insignificant and many of the removed lesions do not present dysplastic changes at this stage. On the other hand, the possibility that a branch duct IPMN develops into PDAC is lower, so those cases without mural nodules, asymptomatic and smaller than 3 cm may be monitored at regular intervals (3). Cytology specimens may be obtained by EUS to diagnose solid and cystic lesions of the pancreas. However, the sensitivity of cytology is limited so the search for other diagnostic markers is required. Only two studies have researched the expression of cathepsins in IPMN. One of them showed that the cathepsin E gene is overexpressed in more than half of patients with these neoplasms (36). This finding suggests that these lesions share a genetic profile with PDAC. However, the other study did not observe expression of cathepsin B in any of the three patients (27). In our study, the expression of cathepsins was generally low in 8 patients with this neoplasm; cathepsin L was expressed in half of patients. No data has been published about the expression of cathepsins in MCN. Cathepsins H, B and S expression was observed in one of the three neoplasms in our three patients with MCN (although each one was not expressed in the same patient). Cathepsin L was not expressed in any neoplasm. Thus, we observed expression of the different cathepsins studied in between 27 and 36% of patients with potentially malignant lesions. These data are significantly lower than the data from patients with PDAC, but similar to the patients with a benign pathology. This questions the physiopathological role of cathepsins in the non-malignant pancreatic mucinous neoplasms and restricts its diagnostic value in these lesions. However, the sample was small because only three patients had a malignant IPMN, and it is surprising that expression of all cathepsins was detected in all of them. This suggests that these proteases may play an oncogenic role in these neoplasms.
In conclusion, in the material obtained from surgical specimen, cathepsins are overexpressed in the malignant lesions compared to the premalignant and the benign lesions. Unfortunately, expression of cathepsins is similar in premalignant and benign lesions, so it does not allow discrimination between both types of lesions.
References
1. Ryan DP, Hong TS, Bardeesy N. Pancreatic adenocarcinoma. New Engl J Med 2014;371:1039-49. DOI: 10.1056/NEJMra1404198. [ Links ]
2. Koorstra JBM, Hustinx SR, Offerhaus GJA, et al. Pancreatic carcinogenesis 2008;8:110-25. DOI: 10.1159/000123838. [ Links ]
3. Tanaka M, Fernández del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MQN of the pancreas. Pancreatology 2012;12;183-97. DOI: 10.1016/j.pan.2012.04.004. [ Links ]
4. Gocheva V, Wang HW, Gadea BB, et al. Il-4 induces cathepsin protease activity in tumor-associated macrophages to promote cancer growth and invasion. Genes Dev 2010;24:241-55. DOI: 10.1101/gad.1874010. [ Links ]
5. Garcea G, Neal CP, Pattender CJ, et al. Molecular prognostic markers in pancreatic cancer: A systematic review. Eur J Cancer 2005;41:2213-36. DOI: 10.1016/j.ejca.2005.04.044. [ Links ]
6. Vasiljeva O, Reinheckel T, Peters C, et al. Emerging roles of cysteine cathepsins in disease and their potential as drugs targets. Curr Pharm Des 2007;13:387-403. DOI: 10.2174/138161207780162962. [ Links ]
7. Turk V, Turk B, Guncar G, et al. Lysosomal cathepsins: Structure, role in antigen processing and presentation, and cancer. Adv Enzyme Regul 2002;42:285-303. DOI: 10.1016/S0065-2571(01)00034-6. [ Links ]
8. Turk B, Stoka V, Rozman-Pungercar J, et al. Apoptotic pathways: Involvement of lysosomal proteases. Biol Chem 2002;383:1035-44. [ Links ]
9. Nomura T, Katunuma N. Involvement of cathepsins in the invasion, metastasis and proliferation of cancer cells. J Med Invest 2005;52:1-9. DOI: 10.2152/jmi.52.1. [ Links ]
10. Vasiljeva O, Papazoglou A, Krüger A, et al. Tumor cell-derived and macrophage-derived cathepsin B promotes progression and lung metastasis of mammary cancer. Cancer Res 2006;66:5242-50. DOI: 10.1158/0008-5472.CAN-05-4463. [ Links ]
11. Aggarwal N, Sloane BF. Cathepsin B: Multiple roles in cancer. Proteomics Clin Appl 2014;8:427-37. DOI: 10.1002/prca.201300105. [ Links ]
12. Joyce JA, Hanahan D. Multiple roles for cysteine cathepsins in cancer. Cell Cycle 2004;3:1516-19. DOI: 10.4161/cc.3.12.1289. [ Links ]
13. Reinheckel T, Peters C, Krüger A, et al. Differential impact of cysteine cathepsins on genetic mouse models of the novo carcinogenesis: Cathepsin B as emerging therapeutic target. Front Pharmacol 2012;3:133. [ Links ]
14. Sulpizio S, Franceschini N, Piatelli A, et al. Cathepsins and pancreatic cancer: The 2012 update. Pancreatology 2012;12:395-401. DOI: 10.1016/j.pan.2012.07.011. [ Links ]
15. Hwang JH, Lee SH, Lee KH, et al. Cathepsin B is a target of hedgehog signaling in pancreatic cancer. Cancer Lett 2009;273:266-72. DOI: 10.1016/j.canlet.2008.08.028. [ Links ]
16. Zhang C, Sun J, Liu D, et al. Preliminary research on the pathological role of cathepsin-B in subcutaneous heteroplastic pancreatic carcinoma in nude mice. Chin Med J 2009;122:2489-96. [ Links ]
17. Joyce JA, Baruch A, Chehade K, et al. Cathepsin cysteine proteases are effectors of invasive growth and angiogenesis during multistage tumorigenesis. Cancer Cell 2004;5:443-53. DOI: 10.1016/S1535-6108(04)00111-4. [ Links ]
18. Gocheva V, Chen X, Peters C, et al. Deletion of cathepsin H perturbs angiogenic switching, vascularization and growth of tumors in a mouse model of pancreatic islet cell cancer. Biol Chem 2010;391:937-45. [ Links ]
19. Dumartin L, Whitwman HJ, Weeks ME, et al. AGR2 is a novel surface antigen that promotes the dissemination of pancreatic cancer cells through regulation of cathepsins B y D. Cancer Res 2011;71:7091-102. DOI: 10.1158/0008-5472.CAN-11-1367. [ Links ]
20. Ogbomo SN, Shi W, Wagh NK, et al. 177Lu-labeled HPMA copolymers utilizing cathepsin B and S cleavable linkers: Syntesis, characterization and preliminary in vivo investigation in a pancreatic cancer model. Nucl Med Biol 2013;40:606-17. DOI: 10.1016/j.nucmedbio.2013.01.011. [ Links ]
21. Whiteman HJ, Weeks ME, Dowen SE, et al. The role of S100P in the invasion of pancreatic cancer cells is mediated through cytoskeletal changes and regulation of cathepsin D. Cancer Res 2007;67:8633-42. DOI: 10.1158/0008-5472.CAN-07-0545. [ Links ]
22. Gopinathan A, De Nicola G, Frese K, et al. Cathepsin B promotes the progression of pancreatic ductal carcinoma in mice. Gut 2012;61:877-84. DOI: 10.1136/gutjnl-2011-300850. [ Links ]
23. Paciucci R, Berrozpe G, Torà M, et al. Isolation of tissue-type plasminogen activator, cathepsin H, and non-specific cross-reacting antigen from SK-PC-1 pancreas cancer cells using substractive hybridation. FEBS Letters 1996;385:72-6. DOI: 10.1016/0014-5793(96)00352-3. [ Links ]
24. Niedergethmann M, Wostbrock B, Sturm JW, et al. Pancreatic impact of cysteine proteases cathepsin B and cathepsin L in pancreatic adenocarcinoma. Pancreas 2004;29:204-11. DOI: 10.1097/00006676-200410000-00005. [ Links ]
25. Niedergethmann M, Hildenbrand R, Wolf G, et al. Angiogenesis and cathepsin expression are prognostic factors in pancreatic adenocarcinoma after curative resection. Int J Pancreatol 2000;28:31-9. DOI: 10.1385/IJGC:28:1:31. [ Links ]
26. Chen R, Brentnall T, Pan S, et al. Quantitative proteomics analysis reveals that proteins differentially expressed in chronic are also frequently involved in pancreatic cancer. Mol Cell Proteomics 2007;6:1331-42. DOI: 10.1074/mcp.M700072-MCP200. [ Links ]
27. Ohta T, Terada T, Nagakawa T, et al. Pancreatic trypsinogen and cathepsin B in human pancreatic carcinomas and associated metastasic lesions. Br J Cancer 1994;69:152-6. DOI: 10.1038/bjc.1994.25. [ Links ]
28. Cruz-Monserrate Z, Abd-Elgaliel W, Grote T, et al. Detection of pancreatic tumours and precursor lesions by cathepsin E activity in mouse models. Gut 2012;61;1315-22. DOI: 10.1136/gutjnl-2011-300544. [ Links ]
29. Eser S, Messer M, Eser P, et al. In vivo diagnosis of murine pancreatic intraepithelial neoplasia and early-stage pancreatic cancer by molecular imaging. PNAS 2011;108:9945-50. DOI: 10.1073/pnas.1100890108. [ Links ]
30. Von Burstin J, Eser S, Seidler B, et al. Highly sensitive detection of early-stage pancreatic cancer by multimodal near-infrared molecular imaging in living mice. Int J Cancer 2008;123:2138-47. DOI: 10.1002/ijc.23780. [ Links ]
31. Leto G, Tumminello FM, Pizzolanti G, et al. Lysosomal aspartic and cysteine proteinases serum levels in patients with pancreatic cancer or pancreatitis. Pancreas 1997;14:22-7. DOI: 10.1097/00006676-199701000-00004. [ Links ]
32. Tumminello FM, Leto G, Pizzolanti G, et al. Cathepsin D, B and L circulating levels as prognostic markers of malignant progression. Anticancer res 1996;16:2315-9. [ Links ]
33. Park HD, Kang ES, Kim JW, et al. Serum CA 19-9, cathepsin D, and matrix metalloproteinase-7 as a diagnostic panel for pancreatic ductal adenocarcinoma. Proteomics 2012;12:3590-7. DOI: 10.1002/pmic.201200101. [ Links ]
34. Uno K, Azuma T, Nakajima M, et al. Clinical significance of cathepsin E in pancreatic juice in the diagnosis of pancreatic ductal adenocarcinoma. J Gastroenterol Hepatol 2000;15:1333-8. [ Links ]
35. Azuma T, Hirai M, Ito S, et al. Expression of cathepsin E in pancreas: A possible tumor marker for pancreas, a preliminary report. Int J Cancer 1996;67:492-7. DOI: 10.1002/(SICI)1097-0215 (19960807)67:4<492::AID-IJC5>3.0.CO;2-N. [ Links ]
36. Terris B, Blaveri E, Crnogorac-Jurcevic T, et al. Characterization of gene expression profiles in intraductal papillary-mucinous tumors of the pancreas. Am J Pathol 2002;160:1745-54. DOI: 10.1016/S0002-9440(10)61121-2. [ Links ]
37. Mizuno N, Hara K, Hijioka S, et al. Current concept of enscopic ultrasound-guided fine needle aspiration for pancreatic cancer. Pancreatology 2011;11(Suppl 2):40-6. DOI: 10.1159/000323502. [ Links ]
38. Abd-Elgaliel W, Cruz-Monserrate Z, Wang H, et al. Pancreatic cancer-associated cathepsin E as a drug activator. J Control Release 2013;167:221-7. DOI: 10.1016/j.jconrel.2013.02.007. [ Links ]
![]() Correspondence:
Correspondence:
Juan Martínez Sempere.
Department of Digestive Endoscopy.
Hospital General Universitario de Alicante.
C/ Pintor Baeza, s/n.
03010 Alicante, Spain
e-mail: juanmtzsempere@gmail.com
Received: 04-03-2015
Accepted: 04-08-2016