Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 no.1 Madrid ene. 2017
https://dx.doi.org/10.17235/reed.2016.4205/2016
Hemobilia due to intracholecystic papillary neoplasm
Hemobilia por neoplasia papilar intracolecística
Claudia Páez-Cumpa1, Alicia Erimeiku-Barahona1, M.a Antonia Payeras-Capó1, Isabel Amengual-Antich2 and Carmen Garrido-Durán1
Departments of 1Gastroenterology and 2Pathology. Hospital Universitario Son Espases. Palma de Mallorca, Spain
ABSTRACT
We report the case of a 39-year-old patient who presented an episode of upper gastrointestinal bleeding due to hemobilia. The imaging tests showed the gallbladder occupied by solid tissue, with a diagnosis of intracholecystic papillary neoplasm after the cholecystectomy. The intracholecystic papillary neoplasm of the gallbladder is a newly established entity and it is considered a subtype of intraductal papillary neoplasm of the bile duct. Its presentation in the form of hemobilia has barely been described in the literature.
Key words: Intracholecystic papillary-tubular neoplasms (ICPN). Gallbladder cancer. Papillary carcinoma. Hemobilia.
RESUMEN
Exponemos el caso de un paciente de 39 años que presentó un episodio de hemorragia digestiva alta secundario a hemobilia. Mediante las pruebas de imagen realizadas se objetivó ocupación de la vesícula biliar por tejido sólido, que tras colecistectomía se diagnosticó de neoplasia papilar intracolecística. Se trata una entidad recientemente establecida y se considera un subtipo de la neoplasia papilar intraductal de la vía biliar. La presentación en forma de hemobilia apenas ha sido descrita en la literatura.
Palabras clave: Neoplasia papilar intraductal de la vía biliar. Cáncer de vesícula. Neoplasia papilar. Hemobilia.
Introduction
Hemobilia is defined as a bleeding into the biliary tree and constitutes a rare or infrequent cause of upper gastrointestinal bleeding (UGIB) (1). The most common causes are related to recent history of instrumentation or traumatic damage to the liver and/or biliary parenchyma. Other causes of hemobilia include biliary lithiasis, cholecystitis, vascular abnormalities like aneurysms of the hepatic artery, hepatic abscesses or neoplastic disease. A classic triad of presentation of this disease has been described, which includes biliary colic, obstructive jaundice and UGIB or obscure gastrointestinal bleeding (OGIB), even though it only occurs in 22% of the cases (2). Obstructive jaundice would occur in the case of a clot forming that obstructs the bile duct. Its diagnosis requires a high level of suspicion, since bleeding may be intermittent, with its identification by endoscopy sometimes being difficult.
The data published in the literature about the pathological clinical characteristics of intraepithelial neoplasms of the gallbladder are limited, primarily because of the great variability in their definition and used terminology until recently (3). Intracholecystic papillary neoplasm (ICPN) is considered to be analogous to the intraductal papillary neoplasm of biliary tract (BilIN) and to the intraductal papillary mucinous neoplasms (IPMN), with both entities having an intraluminal growth associated to mucin hypersecretion as well as the four histological subtypes: pancreatobiliary, intestinal, gastric and oncocytic.
Case report
We present the case of a 39-year-old male patient, with no toxic habits, and a personal history of high blood pressure treated with losartan and amlodipine, and an admission to the ICU in 2014 after a traffic accident with multiple bone fractures and traumatic brain injury with secondary seizures, in current prophylactic treatment with levetiracetam.
He attended the emergency department with a clinical picture of asthenia, skin pallor and melena of 7 days of evolution, associated with epigastric pain in recent days. As recent history, he had been treated with ibuprofen and amoxicillin/clavulanic acid for a dental problem in the week prior to the onset of the clinical symptoms. Upon arrival to the emergency room, the patient presented tachycardia of 133 bpm, with normal blood pressure and low-grade fever. In the physical examination a muco-cutaneous paleness was noteworthy, but the rest of the physical examination was without interest, except for the digital rectal examination which turned out positive for melena. The laboratory studies showed a hemoglobin level of 3.5 mg/dl and an altered liver function test (AST 150 U/L and ALT 318 U/L), but the rest of laboratory values were normal. Six red cell concentrates were transfused and an upper endoscopy was performed, demonstrating an oozing bleeding in the duodenum which seemed to come from the ampulla of Vater.
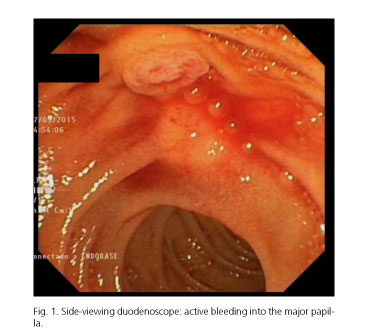
The examination with the side-viewing duodenoscope showed an active bleeding into the major papilla, which had a normal endoscopic appearance (Fig. 1). Subsequently an angio CT was performed, detecting at that time no signs of active bleeding and observing slight dilation of the intra and extrahepatic bile duct, with slightly thickened gallbladder walls. The endoscopic ultrasound revealed gallbladder occupation by a hyperechoic lesion of irregular appearance, with no posterior acoustic shadowing, ruling out the presence of choledocholithiasis. A new imaging study was requested (ultrasound and CT) to study these findings, and it showed the gallbladder occupied by solid tissue, with enhancement compatible with tumoral pathology and no signs of local or remote invasion.
With these findings, the patient underwent a laparoscopic cholecystectomy. The macroscopic examination of the surgical specimen (Fig. 2) showed a gallbladder of 5 x 2.5 cm with a 3 cm villous polypoid lesion completely occupying its lumen, having the implantation basis in the gallbladder fundus. The microscopic examination (Fig. 3) showed a biliary type of ICPN of 3 cm, with foveolar and intestinal focal gastric differentiation, with low grade of focal dysplasia and without invasive component. The adjacent biliary mucosa presented a focal pyloric metaplasia and chronic cholecystitis changes. Resection margins were free. The immunohistochemical study was positive for CK7, MUC1 and MUC 5AC; and isolated focal positive for CDX2, MUC 2 MUC 6. At the 6-months follow-up after surgery, the patient remains asymptomatic, with no new episodes of gastrointestinal bleeding.
Discussion
NPIC is a newly established entity, first described in 2010 in the World Health Organization (WHO) (3) classification. It was previously known as adenoma/papillary carcinoma. This is a rare tumor that forms a papillary or intramucosal polypoid mass often associated with different amounts of mucin. Subsequently in 2012, Adsay et al. described it as an intramucosal exophytic mass in the gallbladder, larger than 1 cm, composed of dysplastic cells forming a lesion with different surrounding mucosa. It is considered as a precursor lesion in the development of invasive gallbladder carcinoma, like BilIN (3). This neoplasia is considered to be analogous to IPMN.
This entity occurs most often in women, with an average age of 60 years. It is often asymptomatic, but compared to BilIN, it is more frequently associated with early symptoms of intermittent pain, jaundice or cholangitis (4).
Otherwise, hemobilia is a low incidence disease by itself, with ICPN being one of their less common causes. After a bibliographic search in PubMed with the keywords "papillary adenocarcinoma and hemobilia" or "adenoma and hemobilia", we found very few reported cases. One of them reported the case of a 25-year-old woman with hemobilia secondary to papillary adenoma of the gallbladder without dysplasia who developed acute cholecystitis, and the other one described the case of a 60-year-old man with upper gastrointestinal bleeding due to papillary adenocarcinoma of the gallbladder with extension to the muscularis propria (6).
ICPN is found in 0.3-0.5% of removed gallbladders due to cholelithiasis or cholecystitis and is usually an incidental finding (7). Occasionally, it appears in association with Peutz-Jeghers syndrome (8) or Gardner syndrome (9).
Four types of histologic subtypes have been described, analogous to IPMN: pancreatobiliary (the most frequent), intestinal, gastric and oncocytic (with a worse prognosis). ICPNs usually show a mixture of papillary and tubular areas, but if the predominant growth pattern is considered, almost 50% of the ICPNs exhibit a papillary pattern. This usually has a biliary phenotype, while the gastric phenotype is mostly associated with tubular cases. High grade dysplasia is more common in papillary and mixed tubulopapillary cases. The pancreatobiliary subtype typically shows CK7 and MUC1 expression, while the gastric subtype usually expresses MUC5AC y MUC6, the intestinal expresses MUC2, CDX2 and CK20, and the oncocytic MUC1. Immunohistochemical staining MUC1 has been described as a marker of poor prognosis in ICPN (3).
Approximately 6% of gallbladder adenocarcinomas arise in association with ICPN. The rate of invasive carcinoma is about 60%. Patients with noninvasive ICPN have a five-year survival rate of almost 80%, which drops to 60% in the case of associated invasive carcinomas. It has been reported in some studies that invasive carcinoma associated with ICPN has a better prognosis than that associated with BilIN (7).
Surgical resection is the final treatment, requiring follow-up for early detection of associated lesions. Although there are no guidelines protocoling the follow-up (5), it is recommended that patients with ICPN are followed up in the same way as those with the classic type of gallbladder adenocarcinoma, as there is at least one case of development of liver metastases 16 months after the diagnosis in a patient with ICPN with no vascular or lymphatic invasion on surgical resection described in the literature (10).
Finally, we would like to highlight the importance of remembering that OGID after upper endoscopy with the presence of blood in duodenum could come from the papilla of Vater. In these cases a side-viewing duodenoscope examination may reach a diagnosis and with this we could avoid other procedures in the diagnostic algorithm of OGID such as wireless videocapsule endoscopy exploration.
In summary, we present a case of hemobilia due to ICPN in a young patient, causing gastrointestinal bleeding with a very infrequent etiology. As is normal, in our case it was confirmed with the pathological examination of the surgical specimen after cholecystectomy, which ruled out the presence of invasive carcinoma and high grade dysplasia, and presented a favorable prognosis despite being MUC1-positive.
References
1. Vañó D, García-Cano J, Gómez-Ruiz CJ, et al. Hemobilia. Rev Esp Enferm Dig 2006;98:216-7. DOI: 10.4321/S1130-01082006000300008. [ Links ]
2. Bloechle C, Izbicki JR, Rashed MY, et al. Hemobilia: Presentation, diagnosis, and management. Am J Gastroenterol 1994;89:1537-40. [ Links ]
3. Adsay V, Jang KT, Roa JC, et al. Intracholecystic papillary-tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are >= 1.0 cm): Clinicopathologic and immunohistochemical analysis of 123 cases. Am J Surg Pathol 2012;36:1279-301. DOI: 10.1097/PAS.0b013e318262787c. [ Links ]
4. Bennett S, Marginean EC, Paquin-Gobeil M, et al. Clinical and pathological features of intraductal papillary neoplasm of the biliary tract and gallbladder. HPB (Oxford) 2015;17:811-8. DOI: 10.1111/hpb.12460. [ Links ]
5. Wani NA, Kosar T, Gojwari T, et al. Hemobilia due to papillary adenoma of gallbladder: Imaging findings. Eur J Radiol 2010;74:e51-4. DOI: 10.1016/j.ejrex.2010.04.001. [ Links ]
6. John A, Ramachandran TM, Ashraf S, et al. Carcinoma gallbladder presenting as hemobilia. Indian J Gastroenterol 1999;18:88-9. [ Links ]
7. Klöppel G, Adsay V, Konukiewitz B, et al. Precancerous lesions of the biliary tree. Best Pract Res Clin Gastroenterol 2013;27:285-97. DOI: 10.1016/j.bpg.2013.04.002. [ Links ]
8. Foster DR, Foster DB. Gall-bladder polyps in Peutz-Jeghers syndrome. Postgrad Med J 1980;56:373-6. DOI: 10.1136/pgmj.56.655.373. [ Links ]
9. Walsh N, Qizilbash A, Banerjee R, et al. Biliary neoplasia in Gardner's syndrome. Arch Pathol Lab Med 1987;111:76-7. [ Links ]
10. Hashimoto S, Horaguchi J, Fujita N, et al. Intracholecystic papillary-tubular neoplasm of the gallbladder presenting with jaundice. Intern Med 2014;53:2313-7. DOI: 10.2169/internalmedicine.53.2778. [ Links ]
![]() Correspondence:
Correspondence:
Claudia Páez Cumpa.
Department of Gastroenterology.
Hospital Universitario Son Espases.
Ctra. de Valldemossa, 79.
07010 Palma de Mallorca, Spain
e-mail: claudiaisabel.paez@ssib.es
Received: 22-01-2016
Accepted: 06-02-2016











 texto en
texto en