INTRODUCTION
An outbreak of pneumonic illness was first reported in Wuhan, China on December 31, 2019. It was recognized as coronavirus disease-2019 (COVID-19), caused by a novel coronavirus (2019-nCoV), renamed later as SARS-CoV-2. As of today, more than 12,315,542 people are infected and there are 554955 deaths worldwide (https://www.worldometers.info/coronavirus). COVID-19 is the 3rd coronavirus spread in 2 decades with a debatable origin. The incubation period of COVID-19 is 3-7-14 days [1, 2]. The disease usually affects adults although critical illness has also been reported in infants. Initial symptoms are fever and dry cough, followed by protracted deterioration to bilateral “Wuhan pneumonia”, breathlessness, and death from respiratory failure due to pulmonary intravascular coagulation (PIC) [3]. Consistent expression of ACE2R on various structures (e.g., lungs, gastrointestinal tract, liver, and blood vessels) renders these organs predisposed to cell entry by the virus resulting in diverse symptoms. The inflammatory response in COVID-19 is reflected by increased C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), lactic dehydrogenase (LDH), D-dimers & transaminases. There is hypoalbuminemia, leukopenia, and lymphocytopenia in 50-75% of cases [4, 5]. Typical radiologic features include: peripheral involvement, pulmonary infiltrates, bilateral pneumonia, and ground-glass opacity [1]. However, the final diagnosis rests on the rRT-PCR of respiratory samples, preferably obtained from the lower respiratory tract, nasopharynx, and oropharynx [2]. The diagnostic sensitivity of rRT-PCR is approximately 70% which usually confirms the diagnosis of COVID-19. Whereas false-positive rRT-PCR occurs due to sampling contamination and degraded/non-transmissible RNA [5, 6], the false-negative rRT-PCR exceeds 30% so that two consecutive negative RNA results are required before releasing the patient of COVID-19 [5, 7]. Serum and urine are often negative for SARS-CoV-2 RNA [5]. Serology is non-diagnostic in the acute phase of COVID-19 because seroconversion takes 7-11 days. About 15% of antibody tests are false positive. There is no recommended treatment for COVID-19. Various drugs are under trial as single or combinatorial therapy. Most of these agents are metabolized by the liver and demonstrate renal excretion (Table 1). Serious side-effects may occur in COVID-19 related hepato-renal injury [8].
COVID-19: IS FACE MASKING THE WAY OF LIFE IN THE FUTURE?
There are several unanswered questions about SARS-CoV-2 regarding viral transmission, host immune response, relapse/re-infection, treatment/prevention, and late complications. These are important issues from the standpoint of intra-familial transfer, community spread, need to quarantine, and duration of isolation. Pakistan is a densely populated, resource-deficient country where COVID-19 is slowly getting out of control because of several reasons mainly illiteracy, lack of coordination and non-compliance to SOPs. Wearing a face mask is the simplest rescue intervention in these circumstances because of the low cost, easy availability, filtering capability, and a critical role in the respiratory epidemic [9, 10]. By definition, the face mask is a therapeutic device, which protects the wearer and nearby individuals from large sprays, respiratory droplets, and coarse or fine aerosols (≥5μm in diameter) [11].
There are three broad categories of face masks: the Standard face masks (SFM)/Standard surgical masks (SSM)/Medical masks (MM), Respirator face masks (RFM)/ High-efficiency particulate air (HEPA) masks (e.g. KF 80; KF 94; N 95), and the Cotton/cloth masks (CM). RFM is available in the UK as filtering face-piece 1, 2, & 3 (FFP 1, 2, & 3), in the USA as N95 respirators (N95R: N=. not resistant to oil & solvents; 95= 95% filtration of airborne particles <0.3μm size) [12]. There is an overall consensus that N95R/ FFP3 masks are superior to all other types due to their high filtering capability (>99%) and tight fit on the face [11, 13, 14]. However, some researchers claim that SFM and RFM provide equal protection (80%) against SARS-CoV-2, especially during non-AGP care [10]. An ideal face mask is the one, which can block the emission of infective bio-aerosol. The overall filtering capacity of SFM and HEPA masks exceeds 90% for particles measuring 0.3-4.5μm and approaches 100% for that above 4.5μm [15]. Cotton masks demonstrate the lowest functional efficacy, which is nearly one-third of the SFM. In a study of 1607 individuals, the particle penetration through CM (97%) was twice higher than SFM (44%) [9]. The functional efficacy of SFM & CM can be upgraded by increasing the number of layers, finer weave [9], and double masking, which protects by an asymmetrical alignment of micropores.
There is little impact on breathing effort and gas exchange as long as the wearer gets adapted to the modified version of the face mask. Prolonged use of a single face mask is not recommended beyond 4 hours due to retention of moisture from exhaled breath. Excessive moisture results in the retention of pathogens, dust, and pollens. It causes rapid damage to mask filter besides aggravating thermal discomfort and suffocation. Ultraviolet germicidal irradiation (UVGI) can be performed for the decontamination of face masks to facilitate their reuse. A high dose of UVGI may weaken the polymers causing an increase in particle penetration [16]. More than 10,000 times reduction in contamination of N95R is reported with autoclave, moist steam, bleach, and benzalkonium [12]. There are several hospital and community situations wherein the use of face masks seems mandatory & even life-saving (Table 2). The face mask is perceived as a symbol of “hygiene” in Asia and a sign of “illness” in the West [17]. Lee et al. maintain that particles measuring 0.04-0.2μm can penetrate the SFM, meaning thereby that SFM cannot filter SARS-CoV-2 [18]. We need to recognize that majority of the past studies about face masks involve non-biological particles, artificial aerosolization, and acts of forced expiration e.g. sneezing and coughing. The protective efficacy of SFM is liable to increase if the velocity factor is eliminated during normal breathing and speaking, although the emission of aerosol will increase with a louder voice. These controversies account for a wide variation (10-84%) in rates of adherence to face masks amongst HCWs [17, 19].
Table 2. Situations which mandate the use of face mask during respiratory outbreakENT: Ear, nose and throat; AGP: Aerosol generating procedure.
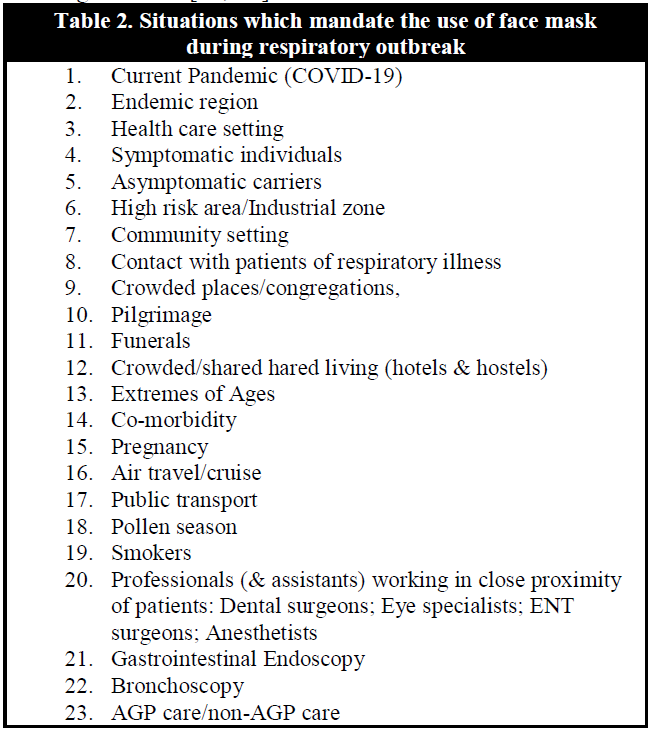
Fracastoro et al. were the first to give the concept in 1546 that tiny particles can cause epidemics by contact from a distance [15]. Face masks were introduced in the mid-19th century, primarily to prevent wound contamination [9]. The device is now extensively used in hospital and community settings for personal protection and source control to prevent onward transmission of infection (Table 2). The face mask has evolved into an essential component of PPE because of its ability to prevent contamination of the environment; microbial transmission, intra-familial/public transfer of communicable respiratory illnesses, hand-to-face contact, and during AGPs. The performance of face mask mainly depends on wearers' knowledge about its proper use: the white side facing in, nose, mouth, and chin covered, single use for <8 hours duration; function of mask layers; and the risk of auto-infection. Jagdesh Kumar et al. have assessed the awareness about correct use of face mask in 392 healthcare workers. The awareness was good in 35.2% while it was moderate in 45.4% and poor in 19.3% participants [20].
Compliance to the use of a face mask is related to wearers' comfort. The respirator masks have fibrous/rigid structure and fit tightly on the face causing significant discomfort, unlike SFM. The use of CM, extended use of face masks, and their reuse is common practice in low middle-income countries such as Pakistan. A cloth mask is one layered rectangular piece of cotton fitted with an ear loop. It is not approved by the FDA because of its low efficacy. Reinforced cotton masks are best suited for asymptomatic persons [21]. RFM/HEPA masks are functionally superior to SFM due to greater filtering capability (95-99% vs 80%) and lower leakage to the face (2-8% vs 22%), respectively [22]. The RFM is FDA approved, cup-shaped therapeutic device-32200, which is equipped with nose piece wire and headband or ear loop. It offers 80-95% protection to the wearer from large droplets and bio-aerosol. SFM is a 3 layered, pleated therapeutic device-32100, which is also FDA approved. It is rectangular in shape and functions by shortening the exhaled air dispersion distance (EADD) covered by an aerosol [23]. Thus, SFM protects patients from wearer-generated infectious droplets [21]. The outer layer of SFM is hydrophobic and repels particles whereas the inner hydrophilic layer absorbs moisture from the exhaled breath [20]. The middle layer (i.e. polypropylene filter) has micropores as small as 8μm so that respiratory viruses including SARS-CoV-2 are easily filtered out %) [24]. The filter layer also prevents wetting to the outer surface thus maintaining the structural integrity of the face mask. The latest evidence to the therapeutic advantage of face masks comes from a meta-analysis of 21 studies wherein authors have demonstrated a significant protective benefit of face masks in HCWs (80%), non-HCWs (47%), household settings (56%), non-household settings (40%), and against influenza virus (45%), SARS-CoV (74%), SARS-CoV-2 (96%) [24]. According to one Japanese survey of 3129 subjects, wearing a face mask is associated with several positive hygienic behaviours such as hand washing, gargling and avoidance of public gatherings/ contact with ill persons [25].
Referring to these improved social behaviours, if a single person adheres to an SOP in the public interest, the cumulative practice would render a far greater benefit to the society i.e. “prevention paradox” [26]. This principle is also applicable to the widespread use of face masks during the COVID-19 pandemic. However, WHO still recommends against mass masking (i.e. source control) (WHO: 19th February 2020) [13, 17] but admit the usefulness of face masks in various situations [19]. WHO recommendations include: SFM for non-AGP care; N95R for AGP care; alcohol-based hand rubs; & physical distancing [2]. N95R is also recommended if the mode of transmission remains unclear or droplet infection is expected to become fatal [9]. It is now proven that aerosol generation may even occur during non-AGP care [9]. The argument of WHO is based on a lack of supportive evidence, fear of global shortage of face masks, and panic buying, which may culminate in disruption of the health system [17]. WHO is also concerned about large scale reduction in mitigation due to a false sense of security provided by the public use of face masks. Frequent lockdowns, physical distancing, isolation, and round-the-clock disinfection of environmental surfaces appear to us as nearly infeasible measures on a long-term basis as compared with simpler interventions such as hand hygiene and face masks. We find poor adherence to this strategy worldwide, inclusive of the developed nations. Lapelletier et al. have proposed suspension of all non-emergent medico-surgical interventions at hospitals to conserve face masks for HCWs during the current pandemic [22]. This policy is also prevalent in many hospitals in Pakistan. In doing so as health care providers, we are ignoring the fundamental Divine principle that all lives matter! We agree that COVID-19 is an unprecedented event in the past 100 years [21]. But COVID-19 is also illness with very low mortality and spontaneous recovery in >95% of cases [27]. We perceive it as a simplistic view of the prevailing situation by denying the right of treatment to millions of non-COVID-19 cases. Many of them have already died on the waiting lists because the current system of on-line treatment is no substitute for clinical evaluation. In our opinion, lack of evidence in the past 200 years about the protective role or inefficacy of face masks is a proof per se for global acceptance of the therapeutic benefit furnished by face masks. Ma et al have recently compared the bio-aerosol blocking efficiency of various types of face masks: N95R (99.98%); SFM (97.14%); & reinforced cotton mask (95.15%), with a conclusion in support of mass masking during COVID-19 [28]. Universal truths do not require back up with scientific research.
The collection of supportive evidence for universal masking is almost impracticable. A palpable lack of clarity in WHO policy about public masking is inadvertently resulting in massive asymptomatic transmissions and intra-familial spread of COVID-19 worldwide. One reflection of this uncertainty was witnessed during recent ethnic protests in the USA and Europe. The majority of protestors did not wear face masks in public and still do not use it despite a surge in new cases of COVID-19 in their countries. The controversial policy of WHO is followed by the CDC, Public Health England (PHE), European Center for Disease Prevention & Control, several western countries, and their leaders. For her population of 1.4 billion, China manufactures 20 million face masks per day i.e. 50% of global production. Between 24th January-29th February 2020, China imported 2 billion face masks to contain the respiratory outbreak. Based on their experience with SARS-CoV (2003) & MERS-CoV (2012), South Korea, Hong Kong, and Singapore set an example by releasing stockpiles of PPE to gain successful control of COVID-19. The orders for compulsory public use of face mask in S. Korea reduced the number of COVID-19 cases to <100/day in 3 weeks [28]. These countries (unlike the west) did not resort to lockdowns, mass testing, isolation, and contact tracing. The results of the stark difference in the preventive strategy are quite obvious today. Huai-Liangwu et al. have calculated daily shortage of face masks in China under three hypothetical scenarios: 589.5 million masks (with uniform masking throughout mainland China); 49.3 million masks (with masking in the epicenter of COVID-19); 37.5 million masks (with no face mask policy) [29]. We know that the cottage industry is very strong in China, South East Asia, Far East, Latin America, and Africa. With proper technical input, they have the potential to compensate for a shortage of face masks world over. This will create an opportunity for the developing nations amidst adversity.
The burden on manufacturing face mask is further reduced by promoting their re-use after sterilization. A household remedy for re-use of face masks is by microwave irradiation, which prevents cell entry by damaging the viral gene A due to microwave generated steam lethality for the virus [15]. Nevertheless, some damage to the mask structure and functional efficiency is expected with these methods. The patient of active COVID-19 contaminates the environment by emitting sprays and infectious droplets during exhalation, sneezing, coughing, and speaking. Large droplets soon evaporate to form fine (virus-containing) aerosol (<1μm size). A poorly ventilated space will promote the spread of the virus by atmospheric dispersion of polluted (ambient) air and progressive sedimentation of virus on the environmental surfaces. Recirculation of fresh air dilutes viral concentration whereas use of face masks will minimize the dose of microbial exposure in closed environments. These measures are aimed at reducing the survival and transmissibility of SARS-CoV-2. They can be reinforced by making use of adjustable environmental factors: raised ozone level (48.83-94.67 micrograms/cubic mm); increased temperature [4]; & low relative humidity (23.33-82.67%). Administered ozone (33-75 micrograms/cc) will have an antiviral effect by the release of tumor necrosis factor (TNF), interferons (IFNs), and interleukin-2 (IL-2). Temperature >56*C is lethal to SARS-CoV-2 [15]. The overall protective efficacy of face mask will depend on its: type; duration of use/reuse; use with/without PPE; & use in AGP/non-AGP care. Any type of face mask should be changed after prolonged wearing especially if there is an accumulation of moisture, structural damage, or loose fit [14]. The technique of donning & doffing a face mask is critical to the wearer for avoiding self-contamination by re-aerosolization of virus from the mask surface. To effectively control the future waves of COVID-19, WHO should soon come up with clear guidelines about the public use of face masks and which type of face mask for use in particular settings.
A COST-EFFECTIVE APPROACH TO COVID-19: AUTHOR'S VIEWPOINT
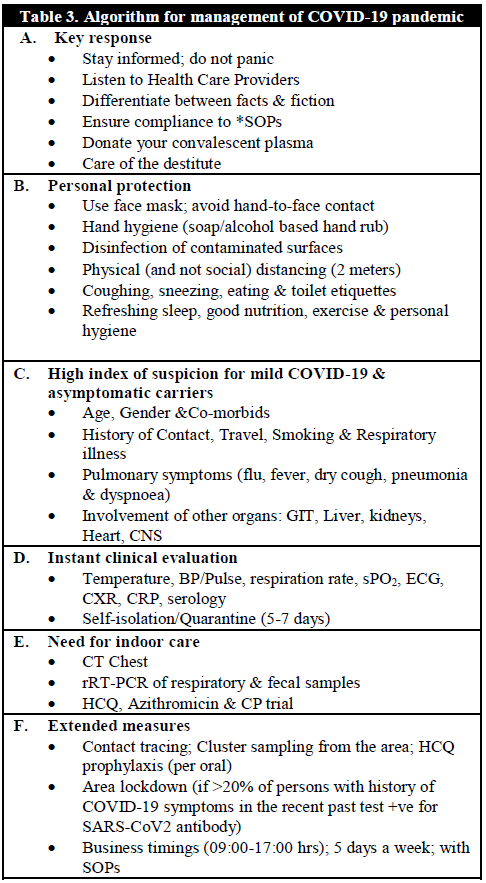
COVID-19 is still on the rise in every continent. With gradual adaptation to the pandemic scenario, more and more people avoid now reporting to the public health authorities. The cost of evaluation with multiple rRT-PCRs is high. There is a fear of follow-up by local police after registration as COVID-19 patient. Compliance to compulsory isolation and stay home orders are a challenging tasks especially for the daily wagers. Lockdowns and travel restrictions have seriously impacted our economy. The education is brought to a near halt. Psychological issues and stigma of the disease are adversely impacting our social fabric to an extent that “social distancing” is transforming into “social cut off”. There is growing perception that COVID-19 is “just another flu” which is “man-made conspiracy for economic gains and reduction in world population”. In this situation of rumor-mongering, the key response to the pandemic is closely linked with our attitudes and behaviours as responsible citizens of a country (Table 3). Despite high infectivity of COVID-19, the glimmer of hope lies in its mild course and spontaneous resolution in the majority [27]. Using “SIR” (“susceptible, infected, recovered”) model, 26th of May, 2020 was expected to be the peak infection day in Pakistan with anticipated number of COVID-19 patients reaching 59211209, followed by slow decline on 24th June to reach 3698192 cases and cure rate exceeding 90% [30]. However, true burden of disease cannot be calculated from these numbers because rRT-PCR testing in Pakistan is restricted to overtly symptomatic persons only due to reasons of low affordability. With evolution of COVID-19 in the past 9 months, we have learned that both genders and all ages are equally affected [31]. The co-morbids occur in >20% of patients with COVID-19: cerebrovascular disease (>50%); arterial hypertension (14.9%); diabetes mellitus (7.4%); coronary artery disease (4.2%). More than 87% of the elderly with co-morbids develop serious disease and 72.2% require intensive care [32]. Although non-specific features such as fever and radiologic abnormalities are absent in >50% of confirmed COVID-19 patients [31, 33], thermal scanning (i.e. detection of fever >38*C) [1] is surprisingly the most popular screening method adopted at all domestic and international portals of exit/entry. In our opinion, a brief history and combinational use of tachycardia, arterial hypertension, tachypnoea (>30/minute), and hypoxia (sPO2 <93% on pulse oximetry), supported by ECG, chest X-ray and serology can detect active disease more frequently than thermal scanning alone. Chest x-ray demonstrates bilateral pulmonary infiltrates in 14% of COVID-19 patients [32]. Serology identifies past exposure to SARS-CoV-2 and helps trace contacts or convalescent plasma donors [6, 27]. We suggest that all these parameters should be summed up in a COVID-19 Proforma as one of the SOPs for domestic and international travelling (Table 3). Detection of COVID-19 antibodies is a cost-effective albeit underestimated method for screening and diagnosis. We suggest to: isolate the suspect for 7 days; test for IgM at 7-10 days from symptom onset; test for IgG at 12-14 days from symptom onset or after the disappearance of symptoms; screen asymptomatic individuals with IgG testing; & reserve rRT-PCR for patients with equivocal results. Further disposal of infected persons depends on the information contained in (Table 3).
A smart lockdown approach is always preferable to the incapacitating complete lockdown of a city. We suggest regional lockdown if more than 20% of previously symptomatic albeit misdiagnosed cases from a cluster of 100 inhabitants test positive for COVID-19 IgM or IgG antibody (Table 3). One intriguing feature of SARS-CoV-2 is the subtle transmission by conjunctival & oral routes through hand-to-face contact [2]. This mode of transfer may occur inadvertently during repeated adjustment of face mask, use of PPEs, and by touching virus-laden inanimate objects. Hand-to-face contact is estimated to occur about 23 times per hour whereas a contact of 5 seconds can transfer >31% of viral load to our hands [2]. SARS-CoV-2 can travel for 4 meters (13 feet) away from the source and remains viable for 3 hours in aerosols [34]. However, SARS-CoV-2 can persist on latex gloves (8 hrs), paper (1 day), medical gowns (2 days), and metal, wood, plastic, and glass (9 days) [2, 13, 35]. The environmental surfaces are amenable to complete disinfection with 60-70% ethanol, 70% 2-propanol, or sodium hypochlorite [2]. The aforementioned observations indicate the significance of frequent hand sanitization [31]. We do not support the use of gloves (Table 3), which are more prone to contamination after they become soft and crumpled by the moisture of hands. SARS-CoV-2 appears in saliva, gastric mucosa, stools and urine long before its detection in the airways [33]. Of more than 50% RNA positive stool samples, 20% or more are RNA negative in the respiratory swabs [36]. It is proven that faecal shedding of SARS-CoV-2 occurs during the acute phase of illness [5]. Do these unusual features suggest that oral route constitutes the dominant route of viral entry? Fact of the matter is that we still need to learn about several unresolved aspects of COVID-19. There is another controversy growing amongst our people if SARS-CoV-2 could spread from the body surface of a deceased. The bereaved families are often resentful of not being permitted to bury their dead. The stigma of COVID-19 certainly adds to this emotional side of the pandemic, which deserves to be explored.
CONCLUSIONS
Face masks, hand hygiene and stringent SOPs (e.g. COVID-19 Proforma for air travel can effectively prevent future a wave of COVID-19 provided the threat of a pandemic is genuinely perceived by the general public.
WHO guidelines about universal masking during respiratory outbreaks deserve priority and clarity.
Thermal scanning for COVID-19 should be complemented by other clinical parameters for more accurate instant evaluation.
Regardless of race, ethnicity and religion, the UNO, WHO and rich countries have a huge responsibility to share their expertise, knowledge and resources with developing nations in the larger interest of mankind.