Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Archivos Españoles de Urología (Ed. impresa)
versión impresa ISSN 0004-0614
Arch. Esp. Urol. vol.62 no.2 mar. 2009
Adenomatoid tumors of the epididymis and testicle: report of 9 cases and bibliographic review
Tumor adenomatoide de epidídimo e intratesticular: a propósito de nueve casos clínicos y revisión de la literatura
Mario Álvarez Maestro1, Raquel Tur González, José María Alonso Dorrego1, Jesús De la Peña Barthel1 and Manuel Nistal Martín De Serrano
1Urology and Anatomo Pathological Service. La Paz University Hospital. Madrid. Spain.
SUMMARY
Objective: To report the cases of adenomatoid tumors seen at Hospital Universitario La Paz in the last 15 years.
Methods: A clinical, pathological, and surgical study was conducted of males with testicular or paratesticular tumors with a histological report of adenomatoid tumor.
Results: Among the nine cases studied, seven had paratesticular and two intratesticular adenomatoid tumors. Treatment of choice was mass removal for epididymal tumors and orchidectomy for intratesticular tumors.
Conclusions: Adenomatoid tumors are uncommon benign neoplasms of a possible mesothelial origin. Because of their benign nature, the treatment of choice is local excision (conservative surgery), but orchidectomy was performed in two cases due to tumor location.
Key words: Benign paratesticular tumors. Epididymis. Adenomatoid tumors.
RESUMEN
Objetivo: Describir los casos de tumores adenomatoides del Hospital Universitario La Paz en los últimos 15 años.
Métodos: Se ha realizado estudio clínico, anatomopatológico y quirúrgico de los varones con tumoración testicular o paratesticular con resultado histológico de tumor adenomatoide.
Resultados: En total hay nueve casos; siete presentaron tumor adenomatoide de localización paratesticular y dos intratesticular. La exéresis de la masa fue el tratamiento de elección en los epididimarios y orquiectomía en los intratesticulares.
Conclusiones: Los tumores adenomatoides son neoplasias benignas, poco frecuentes, de posible origen mesotelial. Como consecuencia de su naturaleza benigna, el tratamiento de elección es la exéresis local (cirugía conservadora), aunque en dos casos se llevó a cabo orquiectomía debido a su localización.
Palabras clave: Tumores paratesticulares benignos. Epidídimo. Tumores adenomatoides.
Introduction
Paratesticular tumors are uncommon, accounting for less than 10% of intrascrotal neoplasms, and most of them (70%-80%) are benign (1). Adenomatoid tumors are the most common neoplasms in paratesticular tissue, accounting for approximately 30% of them. In males, these tumors occur in the epididymis, testicular tunics and, rarely, the spermatic cord. In females, tumors have been reported to occur in the uterus and Fallopian tubes, and rarely in the ovary (2). Cases have been reported in other locations, including pleura, adrenal gland, or liver (3,4).
These tumors are benign in character, and tumor excision is therefore the treatment of choice. However, they are recognized to have a minimum infiltrative behavior.
Materials and methods
All male patients with intratesticular or paratesticular tumors with a pathological report of adenomatoid tumor seen in the last 15 years at Hospital La Paz were eligible for the study. Age, physical examination, clinical signs, tumor markers, pathological characteristics, and surgical treatment were evaluated in all cases.
Results
A total of nine cases were analyzed. Patient age ranged from 21 and 65 years. As regards personal history, three patients had cardiovascular risk factors (smoking, dyslipidemia, or HBP), one patient had sustained multiple trauma at a young age and a malignant prostate tumor, one patient had essential thrombocytosis, and one patient suffered chronic kidney disease. An increased consistency mass in the testicular region was detected in all patients by palpation. The mass was located in the epididymis in seven patients and inside the testis in two patients. Tumor markers were negative in all patients (Table I).
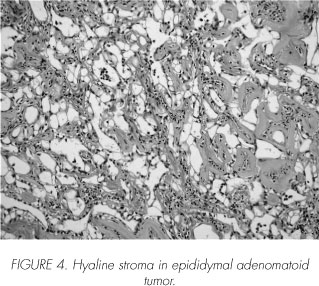
The pathological report confirmed the condition in all nine patients. Adenomatoid tumors with a glandular and alveolar pattern were reported in eight and one patients respectively. Lymphoid proliferation was found in all cases. A hyalinized stroma and smooth muscle hyperplasia were seen in two patients each. One patient showed dysgenetic tubular hyalinization and rete testis pseudo-hyperplasia (Table II). The surgical procedure was tumor removal in all cases except intratesticular tumors, in which orchidectomy was performed.
Discussion
Paratesticular tumors account for 7%-10% of intrascrotal masses. Seventy-five to 90% of all these tumors originate from the spermatic cord, and most of them are benign (70%). Epididymal and testicular tunic neoplasms are next in frequency (though the latter are very rare). Epididymal tumors may be primary or, more rarely, secondary. A review by Beccia et al. (5) reported that 75% of 341 epididymal tumors were benign in nature. Among these, adenomatoid tumor (73%), leiomyoma (11%), and papillary cystadenoma (9%) were the most common. The remaining neoplasms (7%) were benign tumors of a diverse histological origin (angioma, lipoma, dermoid cysts, fibroma, hamartoma, teratoma, and cholesteatoma).
Malignant tumors account for 25% of all epididymal neoplasms. Of these, 44% are sarcomas, 27% metastatic tumors, and 24% primary epididymal carcinomas.
As a group, adenomatoid tumors account for approximately 30% of all paratesticular neoplasms. In males, adenomatoid tumors are more common in epididymis, but may also occur in the testicular albuginea or vaginal tunic and spermatic cord. Other potential locations include the deferent ducts, prostate, and adrenal glands. In females, adenomatoid tumors have been reported to occur in uterus, Fallopian tubes and, rarely, ovary. Like most intrascrotal tumors, adenomatoid tumors are more common in Caucasians.
There are several theories about their histogenesis: mesothelial, Müllerian, mesonephric, and endothelial origin. The hypothesis of a mesothelial origin is the most widely accepted, and is supported by electron microscopy (6) (showing cells very similar to those in normal mesothelium and mesothelioma) and immunohistochemical studies (high hyaluronic acid levels, as in mesotheliomas) (7). In some publications, these tumors are reported as benign mesotheliomas. The reason for their preferential genital location has not been adequately explained.
Some authors think that they represent a reaction to aggression or inflammatory processes.
Tumors are diagnosed in adulthood, with the greatest incidence occurring between the third and fifth decades of life, but neoplasms have been reported in patients aged 20 to 80 years. Clinically, the condition occurs as a painless mass discovered by chance by the patient, though pain may occur more rarely. A small, slow-growing lesion 2 cm to 5 cm in size, predominately located in the left side, is usually found. Most tumors originate from the lower or upper poles of epididymis or in their vicinity. A slightly higher incidence in the lower pole has been reported. The neoplasm sometimes causes pain or mild discomfort. It is occasionally associated to hydrocele. An ultrasound examination reveals the solid nature (hyperechogenic homogeneous mass, though it may adopt any morphology) of the lesion and its location (8). MRI may be of value for differentiating these lesions from other pathological conditions (Figure 1).
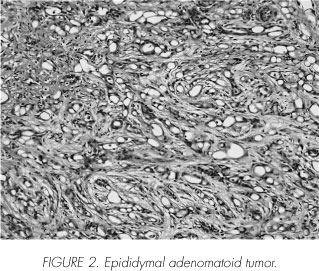
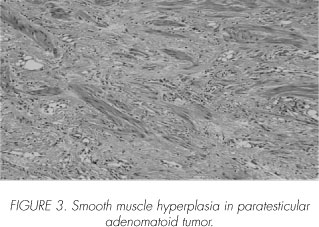
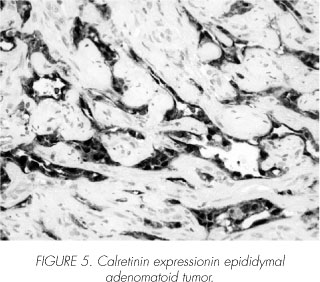
Gross examination reveals a small, round, solid tumor of an elastic consistency. On sectioning, a white, yellow, or brown surface of a fibrous appearance is seen. Microscopically, the tumor is characterized by a series of more or less irregular spaces coated by a layer of flat or cubic epithelial cells surrounded by collagenous stroma and even muscle fibers (Figure 2). Epithelial cell arrangement allows for recognizing three patterns: plexiform, glandular, and angiomatoid. Nuclei have a uniform size and chromatin distribution and are usually spherical and central, with a single nucleolus (Figure 3). Cytoplasm is acidophilic and finely granular. Stroma may consist of loose or dense collagen tissue with hyalinization, and is found in variable amounts (Figure 4). A relatively common feature is the presence of vacuoles inside epithelial cells. Vacuoles may be tiny or large, and sometimes eventually occupy most of the cell cytoplasm. Immunohistochemically, these tumors are characterized by their consistent expression of cytokeratin AE1/AE3 and EM. However, they do not express epithelial markers of factors VIII and CD34. Their mesothelial origin is confirmed by the immunohistochemical method for calretinin (Figure 5). Calretinin is a calcium binding protein from the protein S100 family that is located both in cytoplasm and cell nucleus. It was initially identified in neural tissue. Calretinin has a high sensitivity for identifying mesotheliomas and mesothelial cells, and its expression in malignant tumors is very rare.
These neoplasms behave as benign tumors. Nuclear atypia and local invasion have sometimes been seen, particularly in epididymal head tumors, but no cases of malignization, metastasis, or relapse after removal have been reported.
As for other benign lesions in the same location, treatment consists of surgical removal, i.e. enucleation or total or partial epididymectomy when the tumor is well outlined and an intraoperative biopsy leaves no doubt about its benign nature (9).
Montero (10) reported the first case of this type of tumor in Spanish urological literature in 1968. Since then, 35 cases of this rare lesion have been reported.
 Correspondence:
Correspondence:
Mario
Álvarez Maestro
Valderrey, 35 7o dcha.
28039 Madrid. (Spain).
malvarezmaestro@hotmail.com
Accepted for publication: September 3rd, 2008
References and recomended readings (*of special interest, **of outstanding interest)
*1. Moyano Calvo JL, Giraldez Puig J, Sánchez de la Vega J et al. Tumor adenomatoide de epidídimo. Actas Urol Esp 2007; 31: 417-19. [ Links ]
2. Tammela TLJ, Karttunen TJ, Makarainen HP et al. Intrascrotal adenomatoid tumors. J Urol 1991; 146:61. [ Links ]
3. Timonera ER, Paiva ME, Lopes JM, Eloy C, van der Kwast T, Asa SL. Composite adenomatoid tumor and myelolipoma of adrenal gland: report of 2 cases. Arch Pathol Lab Med 2008; 132:265-7. [ Links ]
4. Nagata S, Aishima S, Fukuzawa K, Takagi H, Yonemasu H, Iwashita Y et al. Adenomatoid tumour of the liver. J Clin Pathol 2008; 61:777-80. [ Links ]
5. Beccia DJ, Krane RJ, Olsson CA. Clinical management of nontesticular intraescrotal tumors. J Urol 1976; 116:476. [ Links ]
**6. Nistal M, Contreras F, Paniagua R. Adenomatoid tumour of the epididymis: Histochemical and ultrastructural study of 2 cases. Br J Urol 1978; 50:121. [ Links ]
7. Delahunt B, King JN, Bethwaite PB et al. Immuno-histochemical evidence for mesothelial origin of para-testicular adenomatoid tumour. Histopathology 2000; 36:109-15. [ Links ]
8. Woodward PJ, Schwab CM, Sesterhenn IA. From the archives of the AFIP: extratesticular scrotal masses: radiologic-pathologic correlation. Radiographics 2003; 23:215-240. [ Links ]
**9. Sánchez Merino JM, Parra Muntaner L, García Alonso J. Tumores Paratesticulares. Actualidad en Urología. Acción Médica. 1999. [ Links ]
*10. Montero J. Tumor adenomatoide de epidídimo. Arch Esp Urol 1968; 21:425-28. [ Links ]











 texto en
texto en