INTRODUCTION
Obesity is a disease of rising prevalence now considered as one of the greatest public health problems in modern society. It is estimated that 65% of the world's population lives in countries where overweight and obesity kill more people than malnutrition 1.
Over the last 20 years, the prevalence of female obesity has risen from 8% to 16.9% 2. Of total primary healthcare users, 89.7% are women, and 30.6% of those women are overweight, while 19.5% are obese, testament to the enormity of the socioeconomic impact that obesity has in Brazil 3,4.
Obesity creates a predisposition to chronic, non-communicable diseases, which has a major impact on the health of the working-age population. There are well-established associations between a high BMI and increased morbidity, including from cardiovascular disease, type 2 diabetes mellitus, high blood pressure, stroke, and dyslipidemia 5. The key point is that obesity associated with insulin resistance is responsible for mechanisms that trigger the lipid abnormalities observed in individuals with obesity. These alterations may be responsible for increasing the risk of cardiovascular disease and also contribute to increasing oxidative stress in obesity 6.
There is evidence that vitamin A is involved in the regulation of body fat, which suggests that when vitamin A is deficient (VAD) there occurs an increase in the recruitment of preadipocytes into adipocytes, inhibition of apoptosis, and an increase of adaptive thermogenesis 7,8. Additionally, there are studies supporting that the increase of BMI can be associated with lowest concentrations of serum vitamin A, which suggests that VAD may play a part in the growth of obesity 9,10.
Using anthropometric indicators as predictors of antioxidant insufficiency, we found BMI and waist circumference to have an inverse association with retinol and β-carotene in humans 11. In some studies with adult participants, serum β-carotene was found to have a negative association with BMI, body fat percentage, waist circumference and waist-hip ratio 12,13.
There is also research assuming increased BMI to relate directly to oxidative stress, given that the greater the degree of obesity, the more intense the inflammatory condition to which these individuals are exposed, due to the intra-abdominal adipose tissue increasing production of proinflammatory cytokines, which leads to an increase in oxidative stress and consequently, to greater demand for nutrients with antioxidant action, such as vitamin A 14,15. However, there is a dearth of research comparing serum retinol and carotenoid concentrations and standards for vitamin A intake and their relation to BMI and body adiposity. Some studies have demonstrated lower serum retinol and carotenoid concentrations in individuals with obesity than in eutrophic individuals when their dietary intake of sources of these nutrients, as reported in food frequency questionnaires, is not significantly different 16,17.
The aim of this study was to analyze vitamin A nutritional status through biochemical and functional indicators and its association with anthropometric parameters in women from different BMI ranges with recommended intake of vitamin A.
MATERIAL AND METHODS
This is an analytical cross-sectional study with adult women, scheduled for nutritional care in a Nutrition Ambulatory in the referred Municipal Health Center of the city of Rio de Janeiro, in the period from January 2012 to October 2014. All women who attended inclusion criteria were invited to participate in the study. The research was previously approved by the Research Ethics Committee of the Hospital Universitário Clementino Fraga Filho of the Federal University of Rio de Janeiro (protocol of research no. 011/05).
After the initial approach and clarifications about the goals and procedures of the study, all the women who agreed to participate in the study gave a formal authorization by signing the informed consent, thus joining the first stage of the research that comprised an anthropometric assessment and a food intake survey.
The inclusion criteria were: female gender (aged 20-59 years), from all ethnic groups and social classes, scheduled for nutritional care of Health Unit. The following exclusion criteria were applied in the first phase of the research: inadequacy of vitamin A intake (evaluated in the first phase of research), pregnant women and/or nursing mothers, liver diseases (except for non-alcoholic liver disease), malabsorptive syndromes, acute infection, alcoholism, kidney insufficiency, HIV virus carriers, cancer, and use of vitamin A supplements over the last six months.
After the first phase, the sample was divided into four groups according to BMI ranges 18: eutrophic group (EU), overweight group (OW), obesity class I group (OI) and obesity class II (OII) group.
SAMPLE SIZE
A sample size calculation was performed on the basis of the study. It estimated the prevalence of Brazilian adults inadequacy intake of micronutrients (POF 2008-2009) that demonstrated elevated inadequacy of vitamin A intake in women about 78,5% in urban and rural areas studied 19. Consequently, the prevalence of adequacy was 21.5%.
To obtain a sample size with 95% of confidence interval, considering an adequacy prevalence of 21.5% with a sampling error of 6%, 155 women would be needed with a recommended dietary intake of vitamin A, according to the Institute of Medicine at the end of research. Based on this calculation, the number of attendance evaluated in a period of 18 months, considering the average weekly attendance in the six months prior to the accomplishment of the present research, was 1,080 women (Fig. 1).
ANTHROPOMETRIC MEASURES
In this stage of the research, weight and height of the women participating in the study were measured and BMI was calculated according to the cut-off points recommended by the World Health Organization (WHO) 18. Additionally, waist circumference (WC) was measured, using inadequate the cut-off > 80 cm for women, as proposed by the International Diabetes Federation (IDF) 20.
FOOD FREQUENCY QUESTIONNAIRE FOR VITAMIN A
Women involved in the study were asked separately to recall all the dishes, snacks, or other foods eaten in the 24 hours prior to the survey, regardless of whether the food was eaten inside or outside the house. During data collection, each woman was prompted to make sure that no meal or snack was forgotten. Next, a detailed list of all the ingredients of the dishes, snacks or other foods mentioned in the reported consumed food were collected from each woman via interview. The study participants were then asked to recall how many days they had consumed each of the 15 locally available vitamin A rich foods in the past seven days 21. During training of data collectors, it was stressed that small quantities of food eaten less than one tablespoon should be excluded. This was important as foods eaten below the aforementioned quantities would not contribute significantly to nutrient adequacy but would inflate the score. Minimum consumption of one tablespoon of food was better correlated with probability of adequacy. Food frequency questions were double coded and entered into a custom built spreadsheet, which calculated an overall mean daily intake of vitamin A using the vitamin A content of foods as published in the table of the Instituto de Nutrición de Centro América y Panamá (INCAP) 22. Portion size was assessed using a Photographic Atlas of Food Portion Sizes 21.
Vitamin A intake was compared to the values of the daily intake recommended by the Institute of Medicine in 2001. The cut-off point adopted for the recommended dietary intake of vitamin A was 700 µg/day.
A month after the first procedure, all the women participating in the first stage of the study were again scheduled to receive information about the nutritional diagnosis, including intake of vitamin A, in addition to receiving the relevant dietary guidelines. Women who had reached the recommended dietary intake of this vitamin were invited to follow up the previously established research protocol and, to that aim, they were instructed to appear for the blood collection procedure after a 12-hour fast.
In the second phase of the research, only women who showed the recommended dietary intake of vitamin A were included in accordance with the results of the food intake survey conducted in the previous phase.
BIOCHEMICAL MEASURES OF VITAMIN A AND DIAGNOSIS OF NIGHT BLINDNESS (NB)
The nutritional status of vitamin A was assessed according to biochemical and functional parameters. For biochemical assessment of vitamin A, serum concentrations of retinol and β-carotene were quantified by high-performance liquid chromatography with ultraviolet detector (HPLC-UV), and the following cut-off points were used: < 1.05 µmol/l and 40 µg/dl to indicate inadequacy of retinol and β-carotene, respectively 23,24.
In the functional assessment of the nutritional status of vitamin A, the presence of NB was investigated through an interview standardized by the WHO 25.
The interview was composed of the following questions:
Do you have difficulty to see during the day?
Do you have difficulty to see in low light or at night?
Do you have NB?
Cases of NB were considered when the answer to question 1 was "No" and, at least, one answer to questions 2 or 3 was "Yes". If the interviewed had any ophthalmic problem corrected by glasses or contact lens, he/she was asked about the ability to see with them.
DIAGNOSIS OF DM2
The diagnosis of DM2 took place in accordance with the American Diabetes Association (ADA) 26 guidelines previously endorsed by the Brazilian Society of Diabetes, which classifies the levels of blood glucose into ≥ 126 mg/dl (fasting) or > 200 mg/dl (one-off).
OTHERS BIOCHEMICAL MEASURES
For biochemical evaluation, a blood sample was obtained by venipuncture after a 12-hour fast period. Laboratory tests were conducted to evaluate: lipid profile (total cholesterol, triglycerides, high-density lipoprotein cholesterol [HDL-c], low density lipoprotein cholesterol [LDL-c]) and the following concentrations were considered as normal values: total cholesterol < 200 mg/dl; triglycerides < 150 mg/dl; HDL-c > 50 mg/dl; LDL-c < 150 mg/dl. Determinations of triglycerides, total cholesterol and HDL-c were performed by the enzymatic colorimetric method. Reagents for these biochemical evaluations were purchased from Labtest Diagnóstica S.A., Minas Gerais, Brazil. LDL-c fraction was determined in accordance with the Friedewald's formula.
STATISTICAL ANALYSIS
In the statistical analysis, the measures of central tendency and dispersion were calculated and expressed as means and standard deviations for clinical, dietary and biochemical variables. The analysis of variance (ANOVA) and the Bonferroni test for multiple comparisons were used. Pearson correlation coefficient was applied for serum concentrations of retinol and β-carotene with variables related to markers of oxidative stress. The odds ratio was estimated to evaluate the strength of the association between serum concentrations of retinol and ß -carotene with biochemical, clinical and anthropometric variables, either the association of inadequacy of serum concentrations of both micronutrients according to BMI ranges. The significance level adopted was 5% (p < 0.05). Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) for Windows version 17.
RESULTS
The sample group comprised 200 adult women, who were divided into four groups according to their BMI. Their characteristics are described in Table 1.
Table I. General characteristics of the sample stratified by BMI groups

Mean and standard deviation. BMI: body mass index; DAIVA: daily intake of vitamin A; EU: eutrophic; OI: obesity class I; OII: obesity class II; OW: overweight; WC: waist circumference.
*p ≤ 0.005.
A statistically significant difference between the classes was observed when considering the variable BMI (EU/OW p = 0.04; EU/OI p = 0.02; EU/OII p = 0.03; OW/OI p = 0.02; OW/OII p < 0.00; OI/OII p = 0.01).
Even with the recommended daily intake of vitamin A, the percentage of vitamin A (retinol and β-carotene) inadequacy was, respectively, 7.5 and 8.8% in the EU, 12.5 and 17.5% in the OW, 17.5 and 25% in the OI and 22.5 and 27.5% in the OII.
When comparing the groups according to the occurrence of NB, a significant difference between them was found (p = 0.002). The breakdown for NB was as follows: 7.5% in overweight women and 12.5% and 20% in women with obesity class I and class 2, respectively. None noted in the eutrophic group of women. The number of women with NB increased in accordance with BMI: three women in the overweight group, seven in the OI group, and ten in the OII group.
The mean of serum retinol and ß -carotene concentrations of the groups is presented in Table 2.
Table II. Mean of serum retinol (μmol/l) and ß-carotene (µg/dl) concentrations in the groups studied
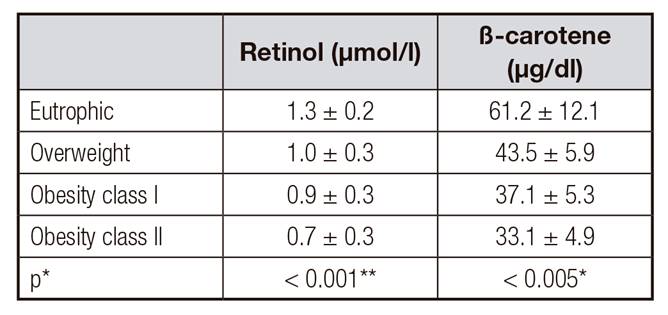
Mean and standard deviation. ANOVA test
*p ≤ 0.005
**p ≤ 0.001.
Overweight women were found to be 14.0, 5.1 and 3.5 times more likely to have inadequate retinol, β-carotene concentrations and NB, respectively. The odds ratio increased to 35.3, 17.0 and 7.4, respectively, in OI, and to 65.4, 26.7 and 9.2, respectively, in OII. Women in the overweight, OI and OII groups were 5.1, 7.2 and 8.0 times more likely to have an inadequate WC, respectively (Table 3).
Table III. Multiple logistic regression analysis of serum retinol and β-carotene deficiency, night blindness and inadequate waist circumference (> 80 cm) in the groups studied

O1/EU: obesity class I/eutrophic; O2/EU: obesity class II/eutrophic; OW/EU: overweight/eutrophic.
†OR: odds ratio
†OR: odds ratio
*OR 95%: confdence interval of 95%
NB: night blindness; WC: waist circumference.
A negative correlation was found between the serum retinol and β-carotene concentrations with inadequate WC in the OW groups (r = -0.32/-0.46; p < 0.001), OI (r = -0.56/-0.70; p < 0.001) and OII (r = -0.68/-0.85; p < 0.001), respectively.
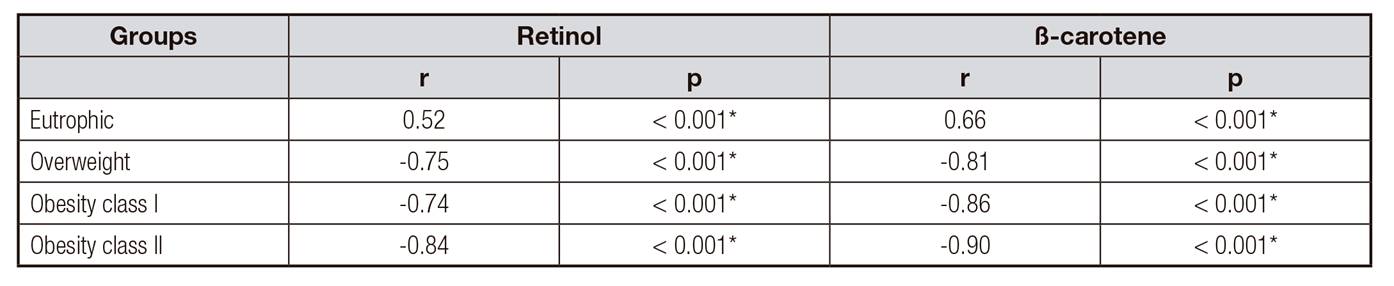
A strong correlation was found between serum retinol and β-carotene concentrations in all the groups studied. Proportionately to the increase in BMI, the negative correlation with serum retinol and β-carotene levels increased (Table 4).
DISCUSSION
Our research showed an inverse relationship between an increase in BMI and alterations in vitamin A nutritional status, as identified in the women assessed to have lower levels of serum retinol and β-carotene, as well as through the diagnosis of NB. Researchers suggest an inverse association between intake and serum concentrations of antioxidant nutrients, such as vitamin A, in the presence of obesity 27,28. Our findings showed that the biochemical and functional vitamin A profiles of overweight and women with obesity are in a much worse state than those of eutrophic women, even if their vitamin A intake falls within the recommended dietary guidelines. The findings draw attention to an important facet of VAD on which to reflect, by demonstrating that even while ingesting the recommended daily vitamin A allowance, the increased demand for the nutrient was found to relate to an increase in BMI and body adiposity, and in the midst of such weight increases, nutritional vitamin A requirements can be much higher than current recommended allowances.
We found serum retinol and β-carotene concentrations to be significantly higher in eutrophic women compared to women with overweight, obesity class I and obesity class II. In addition, the odds ratio were more elevated for serum retinol and ß -carotene deficiency, night blindness and inadequate waist circumference in women with obesity class II. There is a research that compared eutrophic women with those with obesity and the last one had lower concentrations of ß -carotene in the blood, a higher concentration of endothelial adhesion molecules and greater concentrations of blood sugar and insulin, confirming that a rise in body fat leads to increased resistance to insulin, endothelial dysfunction and oxidative stress, and these relate to the processes involved in obesity 29,30. Retinol binding protein 4 (RBP4), which has been referred to as an adipokine that is positively associated with BMI, when analyzed in overweight women confirmed prior research that serum RBP4 is higher relative to ''normal'' levels in lean adults 31. Relatively high serum RBP4 in overweight subjects despite lower retinol levels suggested that some of the serum RBP4 in overweight individuals may be functioning unbound to retinol. Elevated RBP4 with excess body fat has been associated with insulin resistance mediated through suppressed GLUT4 transporter expression 32.
Otherwise, in a study developed by Nuss et al. (2017) 33, β-carotene was not significantly associated with any indicator of body composition (BMI, fat mass and lean mass) in a group of women. Although body composition influences serum nutrient profiles, parameters related to high body-fat mass, such as oxidative stress and inflammation may influence such changes in nutrient levels 33.
There is a study reporting low vitamin A intake as a factor causing VAD in overweight individuals 28. Indeed, inadequate vitamin A consumption was noted in 70% of the 738 women assessed during the first phase of our research, and these findings are in line with the most recent nationwide dietary survey, which revealed a 78.0% magnitude of inadequate vitamin A intake across all the regions studied, both in urban and rural Brazil. Such findings are a cause for concern, given the important role this nutrient plays in cellular metabolism.
We found that the percentages of β-carotene insufficiency were higher than those of retinol, and we also noted a moderate positive correlation between serum retinol and β-carotene concentrations in EU, and a negative strong one in the other groups (OW, OI and OII). Our findings corroborate those of Mecocci et al. (2008) 34, as they show a drop in serum β-carotene concentrations and, at the same time, a drop in circulating retinol values, suggesting more β-carotene is being mobilized for conversion to retinol. These findings may be related to the greater mobilization of β-carotene for conversion into retinol, since β-carotene is known to be a potent precursor to retinol. This finding is noteworthy given how a drop in serum β-carotene concentrations leads to a rise in oxidative stress 34, suggesting that this antioxidant could be being rerouted to other important functions, like combatting oxidative stress, in order to maintain an adequate retinol nutritional status. It is thus important to maintain serum retinol concentrations in order to keep β-carotene functioning as an antioxidant.
There are also studies showing that a buildup of visceral fat and increase in BMI are linked to an increase in lipid peroxidation and decrease in serum retinol and β-carotene concentrations, and thus accompanies a negative antioxidant system 35,36. Furthermore, existing research into vitamin A consumption shows, in such circumstances, vitamin intake to be below the recommended daily allowances 37,38-39.
The main limitation of this study is related to the assessment of dietary intake, the same limitations presented by all studies based on self-reported dietary recall, in particular, underestimation of consumption. Nevertheless, we see no reason to believe that underreporting could have been different between the groups we assessed.
This study demonstrated that even with the recommended intake of vitamin A, a biochemical and functional inadequacy of vitamin A nutritional status associated with overweight, obesity and body adiposity was found. The findings support the hypothesis that vitamin A deficiency in these individuals could arise from the higher metabolism of this nutrient, to which they are more exposed than eutrophic individuals. Demonstrating that these conditions may represent an important cause of vitamin A depletion, as well as aggravating factors for vitamin A deficiency.