INTRODUCTION
Described in 1846 by French doctor Joseph Honoré Simon Beau, Beau’s lines (BL) are transversal depressions in the nail plate that extend from side to side of the nail, which occur after an acute stress event. These lines are a consequence of the pause in cell growth in the proximal nail matrix (1), usually, all nails are affected and become noticeable after 4 to 8 weeks of the acute event (2).
The etiology is unknown, but BL are related to several factors, such as acute febrile syndromes, trauma, pemphigus, Raynaud’s disease, Kawasaki’s disease, chemotherapy and severe malnutrition (3).
Recently, this nail manifestation in COVID-19 was described as a response to inflammation with symptoms of fever, diarrhea and mild hypoxemia (4). However, the reports describe the clinical situation prior to the appearance of BL, but no study describes the assessment of nutritional adequacy during this period.
Thus, the aim of this study is to report the occurrence of BL in a patient with severe COVID-19, addressing nutritional adequacy during the prolonged ICU stay for the first time.
CASE REPORT
The case report was approved by the Ethics Committee under the code CAAE -42673321.3.0000.0096.
A 58-year-old male, obese and previous hypertensive patient presented fatigue, nausea, hyporexia, coryza, dry cough, fever (38.6 ºC) and the diagnosis of COVID-19 was confirmed by the RT-PCR method 8 days after the onset of symptoms. Chest tomography showed multifocal opacities with attenuation in ground glass and peripheral consolidations with perilobular conformation and inverted halo sign. He evolved with progressive dyspnea, respiratory failure and moderate acute respiratory distress syndrome, presenting an arterial pressure of oxygen by the fraction of inspired oxygen (PaO2/FiO2) of 106. A prone position was necessary and also a prolonged protective ventilation in an anesthetic plane with neuromuscular blocker, which culminated in ventilation-associated pneumonia, tracheostomy and ICU length of stay for 33 days.
Exemplifying the laboratory profile of the 3rd, 14th and 27th day of admission to the ICU, high levels of inflammatory markers were observed throughout the hospitalization: CPR, ferritin, D-dimer, in addition to lymphocytopenia and hypoalbuminemia (Table I).
Table I. Laboratory results.
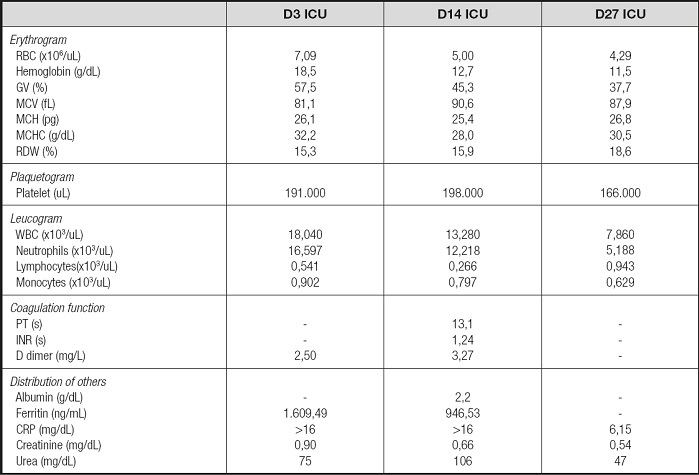
CRP: C reactive protein; D: admission day; GV: globular value; ICU: Intensive Care Unit; INR: international normalized ratio; MCH: mean corpuscular hemoglobin; MCHC: mean corpuscular hemoglobin concentration; MCV: mean corpuscular volume; PT: prothrombin time; RBC: red blood cells; WBC: white blood cells.
In nutritional screening at the admission, the patient had nutritional risk (3 points by Nutritional Risk Screening - NRS 2002) (5), classified as “well nourished” by the Subjective Global Assessment (SGA), and without malnutrition according to the Global Leadership Initiative on Malnutrition (GLIM) (6). Patient with current weight reported in hospital of 112 kg and reported height of 170 cm (body mass index – BMI 38,75 kg/m2), using an ideal weight of 72 kg (maximum BMI for age), according to the institutional protocol, to calculate energy and protein intake requirements.
During the ICU length of stay for 33 days, the patient was on oral nutrition for 2 days, fasting for 1 day and exclusive Enteral Nutrition (EN) support for 30 days.
The patient didn´t show any significant gastrointestinal complications that might had interfered in the intestinal absorption, the only complications were obstipation and abdominal distension, being necessary pharmacological management with rectal glycerin solution in two occasions during the ICU stay.
In the 30-day follow-up of EN, there was a complete infusion record of 27 days, and 4 days were necessary to reach energy target (20 kcal/kg ideal weight) and protein (1.6 g/kg ideal weight). The total energy infused average (1505.6 ± 437.1 kcal) was 86.6 % of prescription (1738.0 ± 304.2 kcal; 18.8 ± 8.6 kcal/kg). As for protein, the average infused corresponded to 90.6% of the prescribed (129.6 ± 40.7 g vs. 143 ± 36.3 g/kg, respectively).
Regarding the micronutrients usually associated with nail manifestations (7), the B vitamins -niacin and biotin- reached the recommendation of the Estimated Average Requirement (EAR) and Adequate Intake (AI) (8)for the patient’s age group, as well as the iron, zinc, copper and selenium. On the other hand, the supply of calcium (94.5 %) and magnesium (61.8 %) was inadequate during the ICU stay (Table II).
Table II. Adequacy of micronutrient infusion according to EAR and AI.
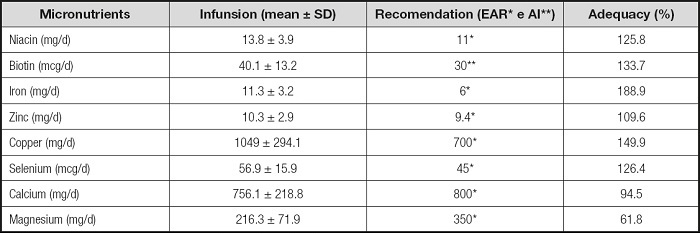
AI: adeaquate intake; EAR: estimated average requirement; SD: standard deviation.
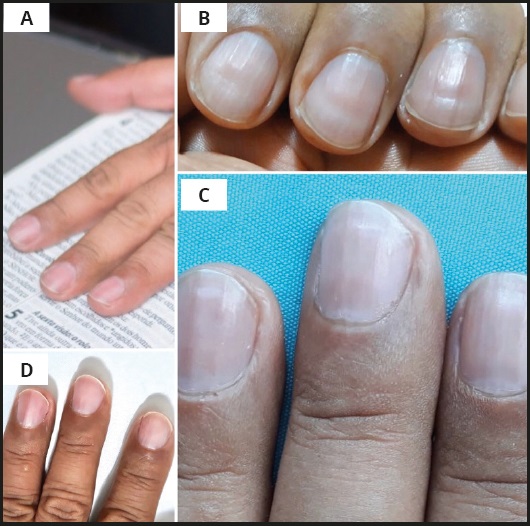
In the first outpatient appointment, two months after hospital discharge, the patient had a measured weight of 89.7 kg (19.9 % weight loss, compared to the weight at the time of admission), showing malnutrition during the ICU stay and after COVID, according to GLIM (8), but without symptoms: gastrointestinal or related to COVID-19, such as anorexia, ageusia or anosmia. The oral intake was similar to the usual, requiring adjustment such as increased protein intake. On the second appointment, after four months of hospital discharge, measured weight was 91.7 kg, remaining without gastrointestinal symptoms and with no reduction in oral intake. In this appointment, the patient complained about transverse linear depressions in the nail plate (Fig. 1) of all fingernails, that suggests BL.
The lines appear first on the lunula and then progress with the growth of the nail. In the referred patient, after 5 months of the acute condition, nail changes were disappearing and in 10 months they disappeared completely (Fig. 1).
DISCUSSION
The probable explanation for the BL in our patient is the acute injury characterized by an important pro-inflammatory cytokine storm (9). The manifestation on the nail coincides with the COVID-19 period of hospitalization.
The nails grow 1 mm in approximately six to ten days, therefore, the measurement of the distance from the transversal depression to the proximal nail fold, allows to estimate the date of the insult, as well as the width of the depression represents the duration of the disease that affected the activity of matrix mitotic (10). In this case, a slightly below expected growth of 10 mm in four months and 2 mm of depression was observed with a period of acute illness of three weeks. A possible explanation is the one described by Dawber (1981) who proposes the influence of immobilization on the performance of nail growth (11). Another possibility is Beau’s pioneering observation in 1846 regarding the implication of serious diseases in nail development, due to the decrease in nutritional supply for the nail matrix (1).
Moreover to the immobilization situation, Guhl et al. (2008) also associate hypoxemia with BL, in a patient with the need for orotracheal intubation and mechanical ventilation for 16 days (12). Similar situation to the case reported in this paper.
As for nutritional deficits, already hypothesized by Beau (1), skin abnormalities are commonly observed in patients with a deficiency of a certain vitamin, mineral or other trace element, and this distinction is delineated by which part of the nail unit was affected. Characteristic of the BL, the change in the nail plate is the last part affected by nutritional imbalances, which are generally associated with a lack of protein, niacin and low serum levels of minerals, such as calcium, magnesium and zinc (7).
The inadequacy in the infused EN protein (90.6 %) and calcium (94.5 %) does not seem to be significant to justify these changes, in addition, calcium does not contribute significantly to nail strength, as it represents only 0.2 % in its composition. Magnesium, with 61.8 %, is associated to weak nails and reduced plasma levels of the mineral (7).
However, it should be considered that critical illness with systemic inflammation and organ dysfunction is characterized by high energy, protein, vitamins and trace elements demands, which are not suppressed by nutrition (13). In this case, attention is drawn to the decrease in the patient’s serum creatinine (Table I), possibly related to the loss of muscle mass characteristic of the critical period (14). Thus, frequent individualized assessment is necessary, as well as studies aiming at the route of administration, doses and their relationship with favorable outcomes (13).
The recommendation of micronutrients to patients with COVID-19 currently follows the requirements established for critically ill patients in general.
This report is the first to show that the BL is manifested after severe COVID-19 in a patient who malnourished during the ICU stay, even with the infusion of nutritional therapy following the current recommendations. However, new clarifications regarding this management have already been published, showing that the metabolic phenotype COVID-19 may be unique, with a longer hypermetabolic phase compared to the previously described models (15).
The implementation of adequate nutritional care in the management of COVID-19 is a challenge due to the lack of evidence, especially regarding to the ideal dose and the need for micronutrient supplementation and protein.