Introduction
Psoriasis is a systemic inflammatory disease of the skin whose global prevalence is between 0.51% and 11.43% (Puig et al., 2021), affecting 125 million people (Kelly-Sell & Gudjonsson, 2017). This disease’s characteristics are having an unknown etiology, being chronic, and showing significant clinical and evolutionary variability defined by the bilateral and symmetrical eruption of red plaques covered with well-defined scales, which form the basis of any diagnosis (Grimalt & Cotterill, 2002). Psoriasis has been considered one of the most stress-related skin diseases, and its onset or recurrence is connected with stress markers (Cannavò et al., 2019; Hunter et al., 2013) and the relationship between stress and the exacerbation of the symptoms (Rousset & Halioua, 2018). Psoriasis has been related to a more significant presence of alexithymic traits (Quinto et al., 2022), symptomatology related to higher levels of stress (Baker et al., 2013), and has been associated with depression (Pietrzak et al., 2017), anxiety (Fleming et al., 2017), and suicidal ideation (Cohen et al., 2016).
As a result, people living with psoriasis could be a target when contemplating interventions that deal with regulating emotions and could benefit from techniques such as mindfulness, which affects emotional regulation and stress management (Fordham et al., 2015; Kabat-Zinn, 1990). Introducing mindfulness in the health context (Kabat-Zinn, 1990) provides an ideal framework of approach to emotional experience through conscious attention to the “here and now.” Previous studies of mindfulness-based intervention programs have shown improvements in people with psoriasis (Fordham et al., 2015; Kabat-Zinn et al., 1998; Montgomery et al., 2016), found that those patients with psoriasis who took part in a mindfulness-based group intervention to complement their usual medical treatment showed significant improvements in the disease's severity and improved quality of life in relation to a control group.
As a tool, mindfulness could be a relevant approach to facilitate both the awareness and regulation of emotional states in psoriasis patients. In this line, one of the key points of the Gross emotion regulation model (2013) is how individuals respond to their emotional states, avoidance strategies being a very characteristic response to addressing emotional disorders. Thus, individuals develop non-adaptive attentional strategies (e.g., distraction, thought suppression, worry, and rumination), which despite being active, affect content beyond personal control or keep the individual distracted from their own emotional experience (Gross & Thompson, 2007). Recent literature has highlighted the relevance of employing emotional regulation and acceptance of emotional states as an adaptive coping style (Jimeno & López, 2019). In this sense, a growing number of studies show the relationship between the practice of Mindfulness-Based Interventions (MBI) and regulating emotions. It has been associated with a lower negative effect (Arch & Craske, 2006; Ramos et al., 2014) and an increase in the positive (Brockman et al., 2017), and less perceived stress (Delgado et al., 2010) and reduced symptoms related to anxiety (Jiménez et al., 2020; Shokooh et al., 2017), guilt (Friese & Hofmann, 2016) or emotional lability (Hill & Updegraff, 2012).
In recent years, an empirical research line examining the immediate effects of brief MBI in laboratory contexts has been developed. These brief MBIs exercised greater control over study variables and, as a result, have been able to be more conclusive about the effects of mindfulness (Keng et al., 2011). According to recent reviews, these brief interventions, either as instructions for adopting a mindful attitude or as a guided meditation, could prove to be an effective intervention to improve negative affectivity (Jiménez et al., 2020; Schumer et al., 2018), stress, anxiety, and resilience in a health context (Gilmartin et al., 2017) or to have an immediate positive effect on the level of emotional reactivity to aversive stimuli (Erisman & Roemer, 2010; Ramos et al., 2014; Schanche et al., 2020). Specifically in patients with psoriasis, these interventions have shown inconsistent results (D’Alton et al., 2019; Maddock et al., 2019). A recent metanalysis highlighted that these interventions need to improve, among other relevant aspects, follow up assessments and the usefulness evaluation for the participants (Zill et al., 2019).
A specific brief MBI would be the Compassionate Emotional Accompaniment Technique (CEAT). The main aim of the CEAT is to facilitate a mindful attitude towards the emotional contents expressed by the person, facilitating its regulation and achieving a conscious emotional expression, which can be understood as a non-reactive experience of emotional acceptance and integration in an optimal zone of physiological activation (Ramos, 2019; Wilbarger & Wilbarger, 1997). This “margin of emotional tolerance,” advocated by Siegel (1999), postulates the need to establish an optimal state of activation to integrate emotions effectively. CEAT would expose the individual to bodily sensations consciously linked to the disturbing emotions. Specifically, to those emotions that they usually try to avoid or suppress, but in this case, they do so under the guidance of the therapist through conscious, compassionate touch, using the calming and relaxing effect of physical contact (Goldstein et al., 2018) and, at the same time, facilitating bodily awareness of the emotion in the body. In this way, the calming effect will enable those emotions above the margin of tolerance and hypoactive to decrease in intensity, and the attentional effect will enable those emotions below the margin of tolerance and hypoactive to increase in intensity and enter the individual's field of consciousness. This technique could also facilitate greater bodily awareness and greater identification with physical sensations and the emotions related to them, facilitating/leading to a better coping process.
Therefore, the aim of this study is to assess the effect of CEAT within a brief MBI for the management of emotions after the induction of negative affect in patients with psoriasis. This pilot intervention evaluated the changes after the application of CEAT, comparing it with an intervention in Emotional Disclosure (ED). A follow-up was carried out 48 hours and one week later to check whether the changes were maintained after the intervention. It was hypothesized that CEAT would be more effective than ED in improving emotional coping after induction and subsequent follow-up and that CEAT would report an improvement in mindfulness state, avoidance, intrusive thoughts, affect, and subjective discomfort.
Methods
Design
This pilot study is a prospective, single-center, randomized controlled trial that was approved by the Health Ethics Committee of the Costa del Sol Hospital (EXP:002sepMR2 / 56-09-2016), respecting the procedures required by the Declaration of Helsinki (World Medical Association, 2013), approved a pilot study with pre-post assessments with the control group.
The inclusion criteria were: a) being 18 years of age or older; b) willingness to participate and providing informed consent ; c) having a diagnosis of non-controllable plaque psoriasis with topical treatment; extensive psoriasis (Psoriasis Area and Severity Index (PASI)> 10); rapid worsening; compromise of visible areas; functional limitation (palmoplantar, genital) or perception of subjective severity (DLQI> 10); and d) completing the Psoriasis Quality of Life (PSO-LIFE; Dauden et al., 2012) questionnaire. The exclusion criteria were: a) being diagnosed with any mental illness that hinders the monitoring of the treatment or the evaluation of the results, or that could interfere with the participant’s ability to complete the study; b) using drugs or exhibiting cognitive problems; and c) patients who could not express themselves in writing or write to a sufficient standard; d) having previous mindfulness or meditation experience.
The dermatologist recruited a sample of 60 adult patients who attended the Dermatology Service of the Hospital and met the inclusion criteria. The estimation for the sample sized is based on García-García et al. (2013) for pilot studies.
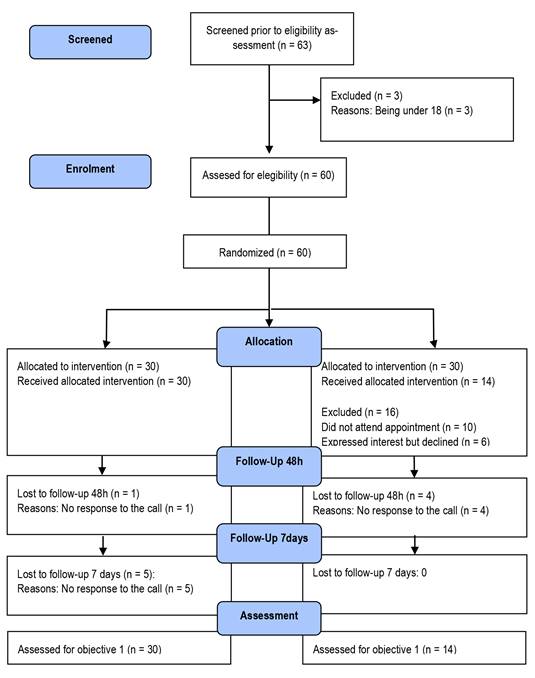
The dermatologist randomly assigned participants to both the CEAT intervention group and the ED intervention group, with 30 participants in each group. The dermatologist also executed the randomization using medical records. After randomization, several participants from control group did not attend to the appointment without reporting reasons for non-participation in the study. Because of that, the ED group sample was reduced to 14 participants (Figure 1). Guidelines for reporting a pilot trial is available as a supporting file in Supplementary file 1 (CONSORT checklist; Eldridge et al., 2016).
Participants
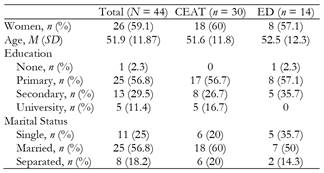
The average age of the sample population was 45.8 years (SD= 13.4), with primary studies (56.8%), and 40.9% were women (Table 1).
Instruments
Psoriasis Quality of Life(PSO-Life; Dauden et al., 2012): This questionnaire assesses the quality of life in patients diagnosed with psoriasis (e.g., “the appearance of my skin makes me sad”). It comprises 20 items with a 5-point Likert scale (from “always” to “never”) that assess the impact of symptoms on emotional well-being, relationships, work, and leisure. The scale showed a good level of internal consistency (Cronbach’s α = .94).
Positive and Negative Affect Schedule(PANAS; Sandín et al., 1999): This questionnaire is a 20-item self-report measure divided into two subscales that assess Positive Affect (PA) and Negative Affect (NA). Each subscale contains 10 items rated from 1 (Very slightly or not at all) to 5 (Extremely). Total score ranges from 10 to 50 by subscale, with higher scores representing higher levels of positive affect and lower scores representing lower levels of negative affect for Positive and Negative Affect subscales, respectively. PANAS showed good internal consistency in the positive affect subscale (Cronbach’s α = .87), negative affect subscale (Cronbach’s α = .78), and total scale (Cronbach’s α = .84).
Impact of Event Scale (IES; Báguena et al., 2001): IES-R is a self-report questionnaire to assess the frequency of intrusive thoughts and avoidance of thoughts and feelings regarding a given situation. Each item was rated on a 4-point frequency of occurrence scale for the past seven days (0 = Not at all, 1 = Rarely, 3 = Sometimes, 5 = Often), with higher scores representing higher levels of intrusive and avoidance symptoms. Total scores for intrusive symptoms and avoidance symptoms are calculated by summing the scores for the relevant items. It showed good internal consistency in the intrusion subscale (Cronbach’s α = .89), avoiding subscale (Cronbach’s α = .83), and total scale (Cronbach’s α = .91).
State Mindfulness Scale(SMS; Tanay & Bernstein, 2013; Spanish adaptation by Campos et al., 2015): It comprises 21 items on a Likert scale (from 1 “Not at all” to 5 “Very good”) designed to indicate how well the phrases describe the experience of the previous 15 minutes (e.g., “I noticed pleasant and unpleasant emotions”, “I was aware of different emotions that arose in me”). The SMS encompasses two factors: Mindfulness State of Mind and Mindfulness State of Body. It showed excellent internal consistency in the Mindfulness State of Body Subscale (Cronbach’s α = .90), in the Mindfulness State of Mind Subscale (Cronbach’s α = .72), and Total Scale (Cronbach’s α = .92).
Psychophysiological markers: A MD-3002 Pulse Oximeter recorded heart rates.
Procedure
The dermatology medical team was blinded about the allocation of participants to each of the intervention groups. A clinical psychologist therapist with expertise in CEAT and ED techniques agreed to deliver the pilot intervention and undertook 60-minutes of training to review intervention contents and strategies for delivery. All the participants were informed about the study's purpose, that they could withdraw from the study at any time without providing a reason, and, finally, they provided oral and written informed consent. Participants also permitted access to their clinical history - affiliation data, medical problems, and previous treatments. Finally, sociodemographic variables were recorded; sex, age, education level, and marital status.
Both assessment and intervention were carried out individually. After the initial assessment, participants received an individual negative affect mood induction with the following instruction based on Ramos et al. (2014):
“We would like you to identify a stressful situation that, in your opinion, is related to the emergence of the psoriasis outbreak, and that arouses a disturbing emotion. For example: if it affects intimacy with your partner, the reaction to other people observing your appearance, fear of criticism, problems at work, etcetera. Now, briefly describe the chosen situation.”
After the 2-minutes induction, the first evaluation was carried out on: (a) a subjective, estimate of the discomfort caused in the present moment (scored from 1 to 5; from “no discomfort” to “much discomfort”); (b) positive and negative affect; (c) the participant’s cognitive coping; and (d) the heart rate. Finally, the participants took part in the intervention group previously assigned. The abovementioned therapist provided an individual intervention that lasted 15 minutes to every member of both groups.
Intervention group
After the negative mood induction and following the proposal by Ramos (2019), CEAT technique was employed. For the intervention group, the therapist accompanied the participant by facilitating conscious breathing and mindful attention to the emerging discomfort through the CEAT (Ramos, 2019). The therapist delivered the intervention in the following essential steps: 1) focusing on the breathing for 3 minutes; 2) focusing on the situation “In the next 15 minutes, I would like you to visualize the chosen situation and identify in your body the physical signs or sensations that the emotion awakens.”; 3) following instructions given at the same time as the therapist and the participant placed their hands on the area of the body where the participant reported feeling the emotional distress; 4) shifting between physical sensations evoked by the instructions and the breathing; 5) finishing the exposition with 3 minutes conscious breathing. During the intervention, patient and therapist are sitting close to each other.
Control group
The control group was an active group comprising ED instruction. The protocol used in other similar studies was applied (Pennebaker, 1990; 1995; Petrie et al., 2004) in order to achieve a specific active intervention that has been effective in a population with psoriasis (Lavda et al., 2012; Zill et al., 2019). The participant is invited to take a seat in front of the therapist with a table disposed for that purpose and the following instruction accompanied the intervention:
“In the next 15 minutes, I would like you to write freely about the situation evoked. Express all the feelings, sensations, and emotions related to that situation.”
The therapist asked to the participant to write down in a piece of paper the feelings, emotions and/or physical sensations evoked by the instruction. After 15 minutes, the task is finished by the therapist. When the intervention is over, in an approximately 5 minutes assessment, the following variables were evaluated: (a) subjective discomfort caused in the present moment (scored from 1 to 5; from “no discomfort” to “much discomfort”); (b) positive and negative affect; (c) state of mindfulness; and (d) heart rate.
There were two follow-up assessments, one after 48 hours and another after seven days. A telephone interview was conducted to assess the following variables: (a) a subjective discomfort caused in the present moment (scored from 1 to 5; from “no discomfort” to “much discomfort”); and (b) the cognitive coping strategies (e.g., intrusive and avoidance of feeling and thoughts). The subjective perception of the intervention’s efficacy was assessed only once during the 48-hour follow-up call.
Data Analysis
All statistical analyses were conducted using SPSS (18th edition). A prior descriptive analysis of the sociodemographic variables was performed. Since the data do not satisfy the assumptions required for parametric tests, and since it is a small sample (Pett, 2015), a non-parametric Wilcoxon range test was performed to test whether the interventions were effective, and a non-parametric Mann-Whitney U test was performed to test whether there were differences between the interventions. A level of statistical significance was established at p < .05 for all analyses.
Results
Since all the measures were self-reported, common method bias was established using Harman’s single factor test. We found a single factor contributing less than 50% in variance (χ2 = 17.25) (Podsakoff et al., 2003). A Wilcoxon Range Test analysis was performed in order to know if the interventions were effective. A Mann-Whitney U test followed this to check if there was a difference between the CEAT and ED interventions.
Intragroup results
Table 2 displays intragroup results. The CEAT intervention showed significant intragroup differences after the intervention compared to the pre-test; with a decrease in negative affect (T = 20.5,z = -4.15,p = .000,r = .54), in the frequency of intrusive thoughts 48 hours later (T = 18,z = -3.65,p = .000,r = .52), in avoidance of thoughts and feelings 48 hours later (T = 65,z = -2.22,p = .02,r =. 32) and after one week (T = 28.50,z = -2.04,p = .04,r = .34).
Table 2. Pre-post intragroup differences.
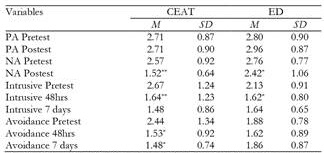
PA: Positive Affect; NA: Negative Affect; Intrusive Pretest: Frequency of intrusive thoughts pretest; Intrusive 48hs: Frequency of intrusive thoughts 48hrs later; Intrusive 7 days: Frequency of intrusive thoughts in the follow up; Avoidance pretest: Avoidance of feelings and thoughts pretest; Avoid ance 48hrs: Avoidance of feelings and thoughts after 48hrs; Avoidance 7 days: Avoidance of feelings and thoughts after follow-up;
*p < .05
**p <.001.
The ED group also showed significant intragroup differences after the intervention compared to the pre-test; with a decrease in negative affect (T = 12,z = -2.35,p = .01,r = .44) and a reduction in the frequency of intrusive thoughts 48 hours later (T = 1,z = -2.38,p = .01,r = .56). There were no differences in the rest of the variables.
Intergroup results
Regarding the intergroup differences before the intervention, PASI scores were lower in the CEAT group compared to the ED group (U = 129.5, p = .04, r = .38). PSO-Life was higher in the ED group compared to the CEAT group (U = 125.5, p = .03 r = .30), indicating that the ED group showed higher quality of life when compared to the CEAT group. There were no significant differences between groups in the rest of the outcomes assessed; subjective discomfort (U = 144, p = .06), heart rate (U = 137.5, p = .16), positive affect (U = 194.5, p = .69), negative affect (U = 177.5, p = .50), the frequency of intrusive thoughts (U = 163.5, p = .40), or the avoidance of thoughts and feelings (U = 166.5, p = .27).
After the intervention, significant differences were found in several variables. Compared to the ED group, CEAT group participants showed lower heart rate (U = 75, p = .002, r = .60), and less subjective discomfort (U = 72.5, p = .00, r = .65), and higher Total SMS (U = 95, p = .005, r = .54), SMS Body (U = 81, p = .001, r = .61), and SMS Mind (U = 115, p = .02, r = .43).
Regarding the 48 hours follow-up, compared to the ED group, the CEAT group showed less negative affect (U = 103.5, p = .004, r = .50) and less subjective discomfort (U = 64, p = .03, r = .46). In the seven days follow-up, significant differences were found in the subjective discomfort (U = 30, p = .005, r = .64) and avoidance of thoughts and feelings (U = 50.50, p = .04, r = .59), being lower in both cases in the CEAT intervention group compared to the ER intervention group. Finally, in the subjective perception of efficacy (U = 60, p = .01, r = .53), CEAT intervention was better rated than the ER intervention for participants (Table 3)
Table 3. Pre-post intergroup differences.

MR: Mean Rank; PASI: Psoriasis Area and Severity Index; PSO-Life: Psoriasis Quality of Life; HR: Heart Rate; SD: Subjective discomfort; Efficacy: Perceived efficacy of the intervention; SMS: State Mindfulness Scale; PA: Positive Affect; NA: Negative Affect; Intrusive Pretest: Frequency of intrusive thoughts pretest; Intrusive 48hs: Frequency of intrusive thoughts 48hrs later; Intrusive 7 days: Frequency of intrusive thoughts in the follow-up; Avoidance pretest: Avoidance of feelings and thoughts pretest; Avoidance 48hrs Avoidance of feelings and thoughts after 48hrs; Avoidance 7 days: Avoidance of feelings and thoughts after follow-up;
*p < .05
**p <.001.
Discussion
The present pilot study is the first to assess the impact of a brief MBI compared to a specific active group of ED in people with psoriasis. These patients suffer an exacerbation of their disease symptoms when they present high stress levels, so interventions focused on the disease's psychological aspect would be very relevant and necessary. The results of this pilot study show that CEAT could be beneficial for this population. Following the hypotheses raised, the participants who received CEAT in the brief MBI showed significant emotional coping improvements after emotional induction and more significantly than the ED intervention. Because CEAT is a specific technique used in an MBI brief, a more significant increase in mindfulness has been found than in the ED group. The CEAT group also experienced a significant reduction in heart rate, whereas the ED group did not. This result is in line with the results of a recent literature review (Sampaio et al., 2017), which highlighted that the practice of mindfulness generated a reduction in heart rate, which could relate to a relaxed body, a calm state of mind, and reflected autonomic nervous system regulation with less effort.
The negative affect has been reduced following the implementation of the CEAT within the brief MBI group. This reduction in the CEAT group is in line with the results provided by previous reviews, which indicated that the brief MBIs affected this variable by decreasing mind-wandering and rumination, increasing the tolerance for negative emotional content, in line with previous studies (Huffziger & Kuehner, 2009; McClintock & Anderson, 2015; McKie et al., 2017; Ramos et al., 2014).
While changes in the rest of the variables were in the expected direction, positive affect did not significantly change from pre- to post-intervention in the CEAT group. This result may be because of the technique's very nature since it would be difficult to expect an increase in positive affect by inducing a negative emotional state. These results are in line with a recent review of a brief MBI brief in a laboratory context in which these types of mood-inducing interventions did not report significant improvements in positive affect post-intervention (Jiménez et al., 2020). Similar to the study carried out by Ramos et al., (2014), no significant differences were found in the frequency of intrusive thoughts after the intervention, either. However, one of the innovative contributions of this pilot study was to find that, after 48 hours, there was a reduction in the frequency of intrusive thoughts. This could point to the fact that a brief MBI does not generate cognitive coping changes immediately, although it could be thought that the emotional changes that occur immediately could be the direct antecedent of short-term cognitive changes. Some studies have shown how trait mindfulness is associated with higher adaptive coping (Feldman et al., 2007; Garland et al., 2010), in contrast to the passive coping that is usually shown in patients with psoriasis (Maddock et al., 2020).
Furthermore, changes in avoidant coping were maintained in the follow-up a week later. Similar to previous studies (Pepping et al., 2015; Ramos et al., 2014), these results could indicate the existence of an improvement after time, even though after the intervention, there were no significant changes in this variable found. CEAT group participants reported a significant reduction in subjective discomfort when asked 48 hours and seven days later and reported that their CEAT intervention was more useful, when compared to ED group participants.
However, there are some limitations to note related to the current pilot trial that need to be considered. First, one the scales, the SMS (Tanay & Bernstein, 2013; Mira et al., 2016) has only been adapted but not validated in Spanish population. Second, this intervention trial was an unfunded pilot, and the enrolled sample was small. Approximately one-third of participants did not attend an appointment or did not complete questionnaires at follow-up appointments, and resources were not available to track people down. Although most post-intervention and follow-up changes were in the expected direction, the study did not carry enough statistical power to detect significant results. Future research could include a third group with a waiting list control group and a larger sample, using different hospitals to make the sample more representative, allowing for a generalization of results and checking which type of psoriasis patient would benefit most from the intervention. For this line of future studies, it could be explored whether another type of clinical population with similar characteristics could benefit from the application of CEAT. It would be of interest to include a long-term follow-up in future studies to determine this type of MBI brief's effectiveness.
Conclusion
Although this is a pilot study and contains several limitations, the results provided are relevant for future research about CEAT. Despite, it provides a new field of investigation based in brief Mindfulness interventions. Firstly, it would be interesting to go deeper into the benefits of the role of the psychologist as a mediator and facilitator in the application of an intervention of these characteristics, especially in populations with no previous Mindfulness training. In second place, it would be interesting to check if populations with a previous Mindfulness training would benefit most from the application of CEAT for managing disturbing emotions.
Finally, it would be necessary to check the effects of the intervention of CEAT in longer follow-up assessments, with a larger number of health centers and in other populations with psychosomatic characteristics. In a way that both individuals with no previous experience in Mindfulness could be monitored in this regard in order to keep a state of conscious attention, as well as those with previous experience could be benefited from the presence of a therapist facilitating the exposure to experiment disturbing emotions.