Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.105 no.10 Madrid nov./dic. 2013
https://dx.doi.org/10.4321/S1130-01082013001000005
ORIGINAL PAPERS
Evaluation of the implementation of Galician Health Service indications and priority levels for colonoscopy in symptomatic patients: Prospective, cross-sectional study
Evaluación de la implantación de las indicaciones y niveles de prioridad del Servizo Galego de Saude para la colonoscopia en pacientes sintomáticos: estudio prospectivo y transversal
Pablo Vega-Villaamil1, María Salve-Bouzo1, Joaquín Cubiella1, Fátima Valentín-Gómez1, Eloy Sánchez-Hernández1, Isabel Gómez-Fernández2 and Javier Fernández-Seara1
1Department of Gastroenterology. Complexo Hospitalario Universitario de Ourense. Ourense, Spain.
2Dirección de Procesos Asistenciales sin Ingreso. Estructura de Gestión Integrada. Ourense, Spain
This study was supported by a grant from "Instituto de Salud Carlos III" (PI11/00094). Instituto de Salud Carlos III had no role in the study design, in the collection, analysis, and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Meeting presentations: XVI Congreso Asturgalaico de Patología Digestiva. Oviedo, November 23-24, 2012 and XVI Reunión de la Asociación Española de Gastroenterología. Madrid, March 20-22, 2013.
ABSTRACT
Background: the Galician Health Service established indications and priority levels (I = fast track, II = preferential, III = normal) for colonoscopy, according to the risk of colorectal cancer and significant colonic lesions detection with access from primary health care. Our aim is to show the results of the implementation.
Methods: we included colonoscopies requested in symptomatic patients from June to October 2012 in a prospective observational cross sectional study. We collected health care level (primary, secondary), priority, appropriateness to the established criteria, wait times (from colonoscopy application and initial consultation) and diagnostic yield for colorectal cancer and/or significant colonic lesion. We compared health care levels in priorities I and II.
Results: 425 colonoscopies were included (I = 221, II = 141, III = 63). The appropriateness rate to the protocol was 67.5 %. Priority levels were significantly associated to wait times (days) from application (I = 8.7 ± 8.9, II = 50 ± 20.3, III = 80.2 ± 32.2; p < 0.001) and initial consultation (I = 32.2 ± 38, II = 74.5 ± 44.2, III = 128.5 ± 47.4; p < 0.001), and with colorectal cancer (I = 20.1 %, II = 19.1 %, III = 4.8 %, p < 0.001) and significant colonic lesion (I = 35.3 %, II = 34 %, III = 19 %, p = 0.002) detection rates. In priority I and II, 21.8 % of colonoscopies were requested from primary health care. Referral form primary health care reduced wait times from initial consultation to colonoscopy (primary = 29.3 ± 26, secondary = 55.2 ± 48.6, p < 0.001). Instead, colorectal cancer (OR 2.41, 95 % CI 1.31-4.42) and significant colonic lesion (OR 1.88, 95 % CI 1.13-3.15) detection rate was increased.
Conclusions: Galician Health Service priority levels are significantly associated with colorectal cancer and significant colonic lesion detection. Referrals to colonoscopy from primary health care reduce waiting times and increase diagnostic yield.
Key words: Colonoscopy. Colorectal cancer. Primary health care. Referrals. Diagnostic yield.
RESUMEN
Introducción: el Servizo Galego de Saúde estableció indicaciones y niveles de prioridad de la colonoscopia (I-vía rápida, II-preferente, III-normal) acorde al riesgo de detectar cáncer colorrectal y lesiones colónicas significativas con acceso desde atención primaria. Nuestro objetivo es analizar los resultados de la implantación.
Métodos: estudio prospectivo transversal y observacional. Se incluyeron las colonoscopias solicitadas entre julio y octubre de 2012 en pacientes sintomáticos. Se recogió el nivel asistencial solicitante (especializada o primaria), nivel de prioridad, adecuación a los criterios establecidos, tiempos de demora (solicitud y consulta inicial) y rendimiento diagnóstico para cáncer colorrectal y/o lesión colónica significativa. Se compararon los niveles asistenciales en las prioridades I y II.
Resultados: se incluyeron 425 colonoscopias (I = 221, II = 141, III = 63) con una adecuación al protocolo del 67.5 %. Los niveles de prioridad se relacionaron significativamente con los tiempos de demora (días) desde la solicitud (I = 8,7 ± 8,9, II = 50 ± 20,3, III = 80,2 ± 32,2; p < 0,001) y la consulta inicial (I = 32,2 ± 38, II = 74,5 ± 44,2, III = 128,5 ± 47,4; p > 0,001); y con la tasa detección de cáncer colorrectal (I = 20,1 %, II = 19,1 %, III = 4,8 %; p < 0,001) y lesión colónica significativa (I = 35,3 %, II = 34 %, III = 19 %; p = 0,002). En las colonoscopias solicitadas con prioridad I y II desde primaria (21,8 %), la demora desde la consulta inicial fue inferior (primaria = 29,3 ± 26, especializada = 55,2 ± 48,6; p < 0,001) y se detectó más cáncer colorrectal (OR 2,41, IC 95 % 1,31-4,42) y lesión colónica significativa (OR 1,88, IC 95 % 1,13-3,15).
Conclusiones: los niveles de prioridad se asocian significativamente con la detección de cáncer colorrectal y lesión colónica significativa. El acceso a la colonoscopia desde primaria reduce los tiempos de demora e incrementa el rendimiento diagnóstico.
Palabras clave: Colonoscopia. Cáncer colorrectal. Atención primaria. Derivaciones. Rendimiento diagnóstico.
Introduction
Colonoscopy demand is gradually increasing in our population (1). In recent years, it has outnumbered radiologic studies (especially barium studies) in the evaluation of patients with gastrointestinal symptoms (2). There are numerous reasons for this increase: high prevalence of gastrointestinal symptoms (3,4), increased incidence of colorectal cancer (CRC) and a higher risk perception in the population (5). Finally, the almost universal use of sedation has improved acceptance of colonoscopy (6,7). However, endoscopic resources to meet this growing demand are limited, resulting in an increase in waiting lists. Although the majority of colonoscopies performed due to digestive symptoms are normal or do not yield changes in the therapeutic approach (8), waiting lists can cause a delay in the start of treatment of organic pathology. In the case of CRC this delay may worsen the prognosis (9).
In recent years several initiatives have been developed to determine the appropriate delay times (10), rationalize the indications for colonoscopy and reduce waiting times for patients with a high suspicion of CRC. Thus, expert recommendations have emerged: European Panel on the Appropriateness of Gastrointestinal Endoscopy (EPAGE), American Society of Gastrointestinal Endoscopy and clinical criteria predictors of CRC detection: the rule of the two weeks of the National Institute for Health and Care Excellence (NICE) for high suspected cancer or the Weighted Numerical Score (11-14). Furthermore, initiatives have been evaluated to reduce delays in the whole diagnosis process from the initial consultation of the patient in the healthcare system: Open-access endoscopy units, coordination between primary healthcare (PHC) and secondary healthcare (SHC), and evaluation of missed opportunities in the diagnostic process (8,15-18).
In this sense, the Servicio Galego de Saúde (Galician Healthcare Service) developed precise indications for colonoscopy in patients with digestive symptoms, as well as priority levels and appropriate optimal time delay according to the risk of CRC or significant colonic lesion (SCL) detection with access both for PHC and SHC. Such indications and priority levels have been initially implemented in the healthcare area of Ourense for their evaluation. The objectives of this study are, on the one hand, to describe the design of the indications, priority levels and subsequent implementation and, on the other hand, to present the results of the appropriateness to the approved indications, time delay, and diagnostic yield of the examinations ordered in the first four months in symptomatic patients. Finally, we consider whether there are differences between colonoscopies referred from PHC and SHC in terms of appropriateness, time delay and diagnostic yield.
Aims and methods
Study design
This is a prospective cross-sectional observational study conducted in the health area of Ourense, in the Complexo Hospitalario Universitario de Ourense (CHOU) as the referral hospital. In this study we included all outpatients referred to colonoscopy due to digestive symptoms between July 1 and October 31, 2012. We excluded those referrals to colonoscopy due to surveillance (familial or personal CRC high risk), endoscopic treatment and those colonoscopies that were not finally performed. As we started with no prior assumptions, a sample size was not determined. Moreover, we decided to analyze arbitrarily the first four months of implementation to assess if there was any early dysfunction.
Design of the indications and priority levels
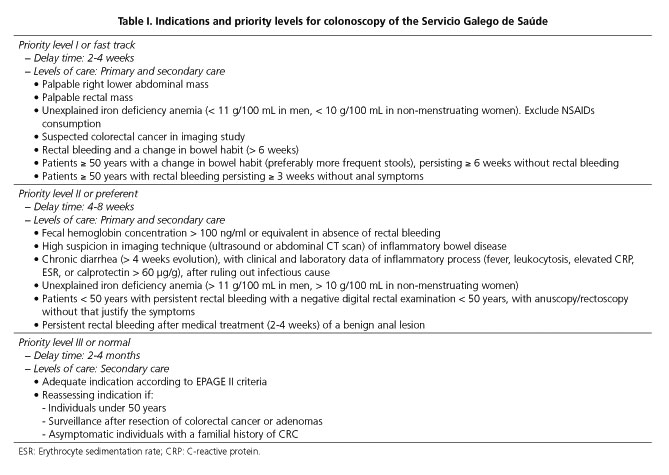
In 2011 the working group "Program for early detection of CRC in Galicia" of the Conselleria de Sanidade was commissioned to design the priority levels and indications for colonoscopy in the Servicio Galego de Saúde, in order to optimize its use. Such working group determined priority levels and indications for colonoscopy based on the risk of detecting CRC and/or SCL, suitable waiting times to performance, which healthcare levels should have access to each priority level, as well as situations in which its performance would not be indicated. Thus, a priority level I (fast track) was established for cases with a high "a priori" probability of detecting CCR (10-20 %) with a delay time of 2-4 weeks and access from PHC and SHC. A priority level II (preferential) was defined for cases with an intermediate probability of detecting CRC (5-10 %) and high probability of detecting SCL (advanced adenomas, inflammatory bowel disease...), with a delay time between 4-8 weeks and access from PHC and SHC. A priority level III (normal) was determined for cases with a low probability of detecting CRC (1-5 %), and intermediate for detecting SCL, with a delay of 2-4 months and access only from SHC. Finally, a fourth priority level (not indicated) was established with a probability of detecting CCR <1 % and a low probability of detecting SCL.
Priority level I used fast track criteria previously defined by the Servicio Galego de Saúde working group to improve the accessibility of the patients with suspected CRC. These criteria were based on a modification of the two weeks NICE's rule (13). Criteria defined for priority level II were based on a consensus group based on the evidence (19-21). All other indications for colonoscopy were included in priority level III. Finally, it was considered that the colonoscopy was not indicated if it was categorized as inappropriate according to EPAGE-II criteria (11). Individuals under 50 years and colonoscopies requested due to high personal or familial risk of CRC were established as risk factors for inappropriate indication (22). Table I shows defined indications in each of the priority levels.
Implementation in the Healthcare Area of Ourense
We performed two actions to implement the indications and priority levels in the Healthcare Area of Ourense. First, colonoscopy application forms for PHC and SHC were designed with fillable boxes with the items proposed in each priority level. These were presented to those responsible for the different levels of care (primary care physicians and representatives of the SHC involved). On the other hand, training programs were conducted in SHC services as well as PHC centers from the area. Specifically, in the case of PHC, a physician from our department conducted a training program in the form of clinical sessions directed to primary care reference physicians in each health center, who subsequently conducted the training of PHC physicians of each health center. In those health centers where clarification was required, specific training was given. Finally, we established an internal procedure for colonoscopy request with quality indicators for further evaluation.
Data collection
Before the colonoscopy procedure, all patients were assessed in a nursing consultation. The nurse used a predesigned questionnaire to register which healthcare level demanded the colonoscopy, the level of care making the request (PHS, SHC), the department responsible of the request and the priority level indicated. This nurse determined the appropriateness of the request to the established criteria and the real level of priority through the questionnaire "Colonoscopy Research Into Symptom Prediction" (23). The questionnaire was translated into Spanish after receiving permission from the authors. Two physicians (PV and JC) performed the translation independently and then a consensus version was obtained. The questionnaire was sent to ten workers in the health area, and twenty colonoscopy patients to determine if it was easily understandable. Based on their comments, the final version was developed. The nurse also collected the date of application of colonoscopy and the date of initial consultation in the healthcare system. From these data, two delays were calculated: since the application of colonoscopy and since initial patient consultation.
The colonoscopies were performed in the usual care practice in our endoscopy unit by experienced endoscopists (> 200 endoscopies per year). In all cases we collected the findings from anorectal examination, the depth of insertion, and the bowel cleansing according to Aronchick scale (excellent when displayed > 95 % of the mucosa; good when liquid remains in 5-25 % of colon with > 90 % of the mucosa displayed; fair-adequate when liquid or semisolid that can be aspirated/washed remains with > 90 % of mucosa displayed; inadequate when there were no semisolid remains that can be aspirated/washed with < 90 % of the mucosa displayed; and poor when there remains solid that impedes vision) (24). We considered that endoscopic examination was complete if the cecal intubation was achieved or if a complete neoplastic stenosis was found. Cleansing was defined as adequate if it was excellent or good. Endoscopists described all colorectal lesions and biopsied as appropriate. Adenomas 10 mm or larger, with villous histology or high-grade dysplasia were classified as advanced adenomas. Significant colonic lesion (SCL) was defined as the finding of CRC, advanced adenoma, adenomatous polyposis or hyperplastic (more than 10 polyps), polyp > 10 mm, colitis of any origin (inflammatory bowel disease, ischemic, actinic, microscopic or infectious), complicated diverticular disease (diverticulitis, perforation or lower gastrointestinal bleeding due to diverticulosis), angiodysplasia in the context of lower gastrointestinal bleeding and colorectal ulcers. Other lesions were considered not significant.
Data analysis
Data were entered in a database. Initially, a descriptive analysis of the sample obtained was performed. Qualitative variables were expressed in absolute numbers and percentages, and quantitative variables as mean and standard deviation. We determined whether there were differences in the appropriateness and diagnostic yield between the different priority levels (application and real) with Chi Square test. The Student's t-test was used to analyze the differences in delay times (since application and initial consultation) between the different priority levels. We also analyzed whether colonoscopies indicated with priority levels I and II showed differences in the appropriateness, delay times and diagnostic yield depending on the level of care. The association between the diagnostic yield and the level of care was expressed as odds ratio (OR) and confidence intervals (CI) at 95 %. In all cases, differences were considered statistically significant if p < 0.05. All statistical calculations were performed using SPSS software, version 15.0 (SPSS Inc, Chicago IL).
Other aspects
Galician Clinical Research Ethics Committee approved this study (Code 2011/038) under resolution dated on March 2, 2011. We accessed patients' clinical histories for study purposes in accordance with the research protocols laid down by our hospital clinical documentation department. Finally, we used STROBE checklist for cross sectional studies to write this original paper (25).
Results
Descriptive analysis
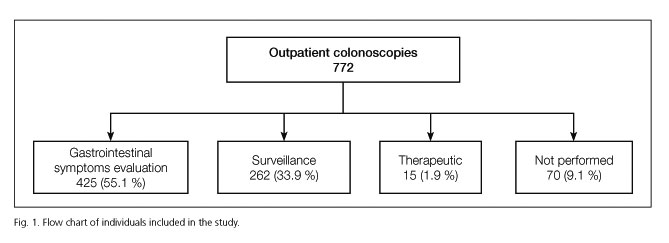
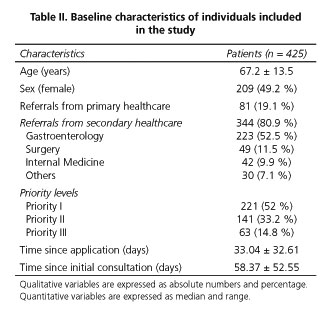
Between 1st July and 31st October 2012, 772 outpatient colonoscopies were applied, of which 347 were excluded from the analysis because they met an exclusion criteria. Finally, 425 colonoscopies ordered due to digestive symptoms that were performed until 11 December (Fig. 1) were included in this analysis. Of these, 221 were ordered as priority I (52 %), 141 as priority II (33.2 %) and 63 colonoscopies as priority III (14.8 %). PHC referred 19.1 % of colonoscopies and SHC referred 80.9 % (52.5 % from gastroenterology, 11.5 % from general surgery, 9.8 % from internal medicine and 7.1 % from other SHC services). Forty-nine point two per cent of the patients were female and 74.4 % were over 60 years (< 50 years: 11.3 %, 50-59 years: 14.6 %, 60-69 years: 23.8 %, 70-79 years: 31.1 % and ≥ 80 year: 19.2 %). Table II summarizes the baseline sample characteristics.
Appropriateness of the orders
The overall appropriateness of the colonoscopies included in the analysis to the criteria and priority levels previously determined was 67.5 %. Sixty-nine point two per cent of the colonoscopies referred in priority level I were adequate (7.3 % were priority II and 23.5 % were priority III); 53.2 % in the priority level II were adequate (19.8 % were priority I and 27 % were priority III) and 90.5 % in the priority III were adequate (4.7 % were priority I and 4.8 % were priority III) to the established criteria. Finally, after reassessing the appropriateness of the 425 colonoscopies included in the analysis, the real priority, was I: 43.3 % (184), II: 22.1 % (94) and III: 34.6 % (147).
Delay times
The overall time delay from the request was 33 ± 32.6 days; and the time delay from initial consultation was 58.4 ± 52.5 days. The time delay from the request was 8.7 ± 8.9 days for priority I, 50 ± 20.3 days for priority II and 80.2 ± 32.2 days for priority III (p < 0.001). The time delay from the initial patient consultation was 32.2 ± 38 days for priority I, 74.5 ± 44.2 days for priority II and 128.5 ± 47.4 days for priority III (p < 0.001).
Diagnostic yield
In the analysis of endoscopic findings (Table III), the digital rectal examination was normal in 53.3 %, a benign anal pathology was detected in 44.9 % and a rectal mass was palpated in 1.4 % of colonoscopies. The cleansing was considered adequate in 86.3 % (excellent: 28.2 %, 58.1 % good) and inadequate in the rest (10.4 % fair, 2.6 % poor, inadequate 0.7 %). Cecal intubation was not achieved in 11.8 % of examinations (rectum 0.2 %, sigmoid 1.2 %, descendent 4.9 %, transverse 2.4 %, ascendant 3.1 %). Nevertheless, the examination was considered complete (cecal intubation or neoplastic stenosis) in 92.5 % of explorations.
As described in table III, CRC was detected in 62 patients (14.6 %) and an SCL in 125 patients (29.4 %). We found a statistically significant association between priority level and CRC detection (I 18.1 %, II 12.8 %, III 6.3 %, p = 0.01). However this association was not statistically significant with respect to SCL detection (I 30.8 %, II 33.3 %, III 15.9 %, p = 0.09). When we evaluated the diagnostic yield based on the real priority, the Servizo Galego de Saude priority levels were significantly associated with the risk of CRC (I 20.1 %, II 19.1 %, III 4.8 %, p < 0.001) and SCL detection (I 35.3 %, II 34 %, III 19 %, p = 0.002).
Comparison of priority level I and II colonoscopies between PHC and SHC
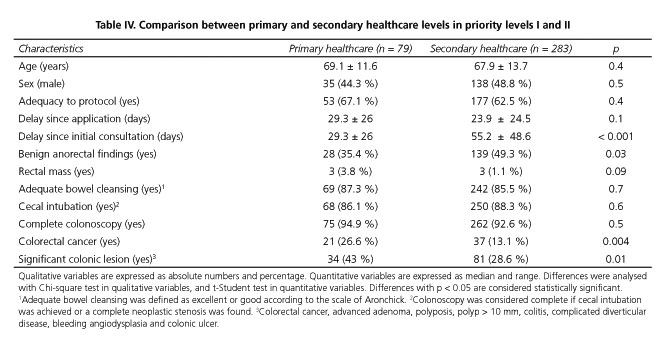
Out of the 362 colonoscopies referred with priority I and II, 21.8 % were referred from, PHC and 78.2 % from SHC, as shown in table IV. We found no differences in age, sex or appropriateness to the indications according to the level of care. Moreover, although there was no statistically significant difference in the time delay from the order, the time delay from the initial consultation to the health system was significantly lower when it was PHC that ordered the colonoscopy (PHC 29.3 ± 26 days, 55.2 ± 48.6 days SHC, p < 0.001), as can be seen in table IV. Finally, no differences were found between the degree of cleansing or depth of colonoscopy insertion according to level of care. Additionally, no differences were detected with respect to the detection of rectal mass on digital rectal examination between PHC and SHC (OR 3.67, 95 % CI 0.7-18.5). In contrast, in patients whose colonoscopy was ordered by PHC, significantly less benign anal disease (OR 0.56, 95 % CI 0.34 to 0.95), more CRC (OR 2.41, 95 % CI 1.31-4.42) and SCL (OR 1.88, 95 % CI 1.13-3.15) were detected.
Discussion
Although the Servicio Galego de Saúde priority levels are significantly associated with the risk of detecting a CRC and / or SCL, its diagnostic yield is reduced by an insufficient appropriateness to the proposed criteria. Moreover, access to colonoscopy for symptomatic patients from PHC after specific training and implementation of colonoscopy applications forms based on items, reduces the time delay from the initial consultation with a higher diagnostic yield than colonoscopies ordered from SHC.
Despite the training provided in the implementation period and the use of structured application forms based on items, the adequacy to approved indications was suboptimal for priority levels I and II in our analysis. However, this problem is common to other programs of prioritization for colonoscopy access. Thus, the adequacy to the two weeks NICE's rule or EPAGE II criteria is between 40-75 % (26,27). It is noteworthy, moreover, that we did not find differences in the adequacy to the protocol between levels of care. Our implementation process was based on two widely evaluated strategies: Active local training and the use of structured questionnaires or applications. In a study evaluating the impact of an educational program on the ASGE criteria, the percentage of appropriate indications increased from 77 to 97 % after completion of the course (28). Moreover, a Cochrane review concludes that, active local training involving SHC specialists and structured referral applications are the only interventions that have an impact on outpatient referral rates (29). The symptom-based criteria have limitations due to the subjective assessment intended to reduce delays, which may decrease its specificity. To improve this limited adequacy, there are several options such as: The use of structured questionnaires of symptoms (14,23,30) or the use of structured applications forms with fill able boxes as were used in our study questionnaires.
Diagnostic oncological process is usually not started at hospitals but it is in PHC where the initial suspicion is established (31). Therefore, it seems reasonable to train primary care physician skills in detecting it, and to provide them with a quick access to diagnostic techniques for reasonable suspicions. Our study confirms that strategies based on training primary care physicians to evaluate patients with digestive symptoms, and allowing them access to endoscopy units, reduces waiting times and increases the diagnostic yield (8). Moreover, it is noteworthy that in those patients undergoing colonoscopies referred directly from PHC, significantly less benign anal pathology was detected. This finding is concordant with several clinical practice guidelines, which recommend a wait and see strategy after application of treatment in rectal bleeding in the absence of alarm symptoms (21,32). This attitude, which is easily achievable in PHC, is difficult to apply in the context of SHC.
Another important aspect of our study is the diagnostic yield of the priority level II (preferential). Our study shows a detection rate of 19.1 % for CRC and 34 % for SCL.
These detection rates are higher than expected when the prioritization criteria were established by the Servicio Galego de Saúde. Although we were unable to specifically analyze each of the items in the priority levels, we believe this is related to the inclusion of fecal occult blood determination by quantitative immunological methods (FIT). Thus, prioritization systems based on symptoms as the two-week NICE's rule have an insufficient diagnostic accuracy for the detection of CRC, both in terms of sensitivity and specificity (19,34).This has led, on the one hand, to an increase in referrals to SHC (35,36) and, moreover, to an increase in delay times in those patients with CRC who do not meet the criteria for quick referral (37,38). However, recent data from a meta-analysis and diagnostic tests studies indicate that FIT is a test with good sensitivity and specificity for the detection of CRC in symptomatic patients (19,39,40). A recently published study has shown that FIT has greater diagnostic accuracy in terms of sensitivity and specificity for CRC detection than NICE prioritization criteria (34). All these data and the results of our study suggest that the FIT test might be a good prioritization criterion itself. However, further studies are necessary to include objective tools, probably based on biomarkers, to improve diagnostic accuracy for CRC detection in patients with gastrointestinal symptoms.
In our analysis, waiting times were adjusted to the requirements set by the Servicio Galego de Saúde. It is known that excessive delay for diagnostic tests causes deterioration in the quality of life perceived by the patient, as well as delays in the initiation of specific treatment (41). However, there is controversy about the effect of the NICE prioritization criteria in CRC prognosis, because it has not been demonstrated that patients urgently referred are either diagnosed in an early stage or have a prolonged survival (37,38,42). The main limitation of our study that may hinder the generalizability of our findings is the high incidence of CRC detected in symptomatic patients. Against 14.1 % in our sample, other studies that have attempted to assess the effectiveness of other strategies for prioritizing colonoscopy detected a significantly lower incidence of CRC, between 1.9-5.2 % (14,30,36,43,44). This can hinder the reproducibility of our results to other populations with lower CRC incidence.
In conclusion, units that offer open-access endoscopy to PHC are able to reduce the delay time without affecting the appropriateness, as well as increasing the diagnostic yield. Training programs designed to improve the appropriateness to the new criteria are needed for both PHC and SHC. Finally, the incorporation of FIT to the prioritization criteria can improve the diagnostic yield of colonoscopy.
Acknowledgments
To the members of the working groups "Programa de detección precoz de CCR en Galicia" (Vicent Hernández Ramírez, Blanca Cimadevila Álvarez, José Ignacio Rodríguez Prada, Ángel Lancho Seco, María Antonia Trueba Moreno, Juan Carlos Álvarez Fernández, Raquel Almazán Ortega, Raquel Zubizarreta Alberdi and Julio García Comesaña), and "Mejora de la accesibilidad de los pacientes con cáncer colorrectal" (Ángel Facio Villanueva, Blanca Cimadevila Álvarez, Luisa Vázquez López, Mercedes Salgado Fernández, Carmen Zueco Zueco, Antonio Gómez Caamaño, Ángel Lancho Seco, Fernando Lamelo Alfonsín, Luciano Sanromán Álvarez, Manuel Gómez Gutiérrez, Juan Carlos Álvarez Fernández); and to the people who facilitated the implementation of the indications and priority levels in Ourense (Ciro Andres Cabezas Cecchi, Antía González Vázquez and the referents in primary care for digestive diseases).
References
1. Argüello L, Pertejo V, Ponce M, Peiró S, Garrigues V, Ponce J. The appropriateness of colonoscopies at a teaching hospital: Magnitude, associated factors, and comparison of EPAGE and EPAGE-II criteria. Gastrointest Endosc 2012;75:138-45. [ Links ]
2. Karasick S, Ehrlich SM, Levin DC, Harford RJ, Rosetti EF, Ricci JA, et al. Trends in use of barium enema examination, colonoscopy, and sigmoidoscopy: Is use commensurate with risk of disease? Radiology 1995;195:777-84. [ Links ]
3. Jones R. Primary care research and clinical practice: Gastroenterology. Postgrad Med 2008; 84:454-8. [ Links ]
4. Quintas Lorenzo P, Dacal Rivas A, Francisco González M, Cubiella Fernández J, López Sánchez L, García García MJ, et al. Referrals to a gastroenterology outpatient clinic from primary care: Evaluation of two programs. Gac Sanit 2011;25:468-73. [ Links ]
5. Clèries R, Esteban L, Borràs J, Marcos-Gragera R, Freitas A, Carulla M, et al. Time trends of cancer incidence and mortality in Catalonia during 1993-2007. Clin Transl Oncol 2014;16:18-28. [ Links ]
6. Baudet J-S, Aguirre-Jaime A. The sedation increases the acceptance of repeat colonoscopies. Eur J Gastroenterol Hepatol 2012;24:775-80. [ Links ]
7. Hüppe D, Lemberg L, Felten G. Effectiveness and patient tolerance of screening colonoscopy - first results. Z Gastroenterol 2004;42:591-8. [ Links ]
8. Quintas Lorenzo P, Dacal Rivas A, Francisco González M, Cubiella Fernández J, García García MJ Fernández Seara J. Effect of the implementation of a program to improve referrals by primary care on appropriateness and wait times in endoscopic examinations. Gastroenterol Hepatol 2011;34:254-61. [ Links ]
9. Alonso-Abreu I, Alarcón-Fernández O, González-Méndez Y, Nicolas-Pérez D, Romero-García R, Gimeno-García Z, et al. Impacto de un programa de cita rápida de colonoscopia en el pronóstico de pacientes con cáncer colorrectal sintomático. Gastroenterol Hepatol 2011;34:186. [ Links ]
10. Paterson GW, Depew WT, Paré P. Petrunia D, Switzer C, Veldhuyzen Van Zanten SJ, et al. Canadian consensus on medically acceptable wait times for digestive health care Membership of the Consensus Group. Can J Gastroenterol 2006;20:411-23. [ Links ]
11. Juillerat P, Peytremann-Bridevaux I, Vader J-P, Arditi C, Schusselé Filliettaz S, Dubois RW, et al. Appropriateness of colonoscopy in Europe (EPAGE II). Presentation of methodology, general results, and analysis of complications. Endoscopy 2009;41:240-6. [ Links ]
12. ASGE Guidelines for Clinical Application. Establishment of gastrointestinal endoscopy areas. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc 1999;50:910-2. [ Links ]
13. NICE Clinical Guideline 27- Referral guidelines for suspected cancer. April 2011. Available at: www.nice.org.uk/CG027 (Internet). 2011. Available from: www.nice.org.uk. [ Links ]
14. Selvachandran SN, Hodder RJ, Ballal MS, Jones P, Cade D. Prediction of colorectal cancer by a patient consultation questionnaire and scoring system: A prospective study. Lancet 2002;360:278-83. [ Links ]
15. Singh H, Daci K, Petersen LA, Collins C, Petersen NJ, Shethia A, et al. Missed opportunities to initiate endoscopic evaluation for colorectal cancer diagnosis. Am J Gastroenterol 2009;104:2543-54. [ Links ]
16. Singh H, Petersen LA, Daci K, Collins C, Khan M, El-Serag HB. Reducing referral delays in colorectal cancer diagnosis: Is it about how you ask? Qual Saf Health Care 2010;19:e27. [ Links ]
17. Sebastián Domingo JJ, Sánchez Sánchez C, Galve Royo E, Mendi Metola C, Valdepérez Torrubia J. Management of open access gastrointestinal endoscopy and quality of care: Collaboration between an improvement team and primary care. Gastroenterol Hepatol 2012;35:65-9. [ Links ]
18. Singh H, Khan R, Giardina TD, Paul LW, Daci K, Gould M, et al. Postreferral colonoscopy delays in diagnosis of colorectal cancer: a mixed-methods analysis. Qual Saf Health Care 2012;21:252-61. [ Links ]
19. Jellema P, Van der Windt DA, Bruinvels DJ, Mallen CD, Van Weyenberg SJB, Mulder CJ, et al. Value of symptoms and additional diagnostic tests for colorectal cancer in primary care: Systematic review and meta-analysis. BMJ 2010;340:c1269-c1269. [ Links ]
20. Jellema P, Van Tulder MW, Van der Horst HE, Florie J, Mulder CJ, Van der Windt DA. Inflammatory bowel disease: a systematic review on the value of diagnostic testing in primary care. Colorectal Dis 2011;13:239-54. [ Links ]
21. Grupo de Trabajo de la Guía De Práctica Clínica sobre Rectorragia. Manejo del paciente con rectorragia. Guía de Práctica Clínica. Actualización 2007. Asociación Española de Gastroenterología, Sociedad Española de Medicina de Familia y Comunitaria y Centro Cochrane Iberoamericano; 2007. Programa de Elaboración de Guías. Disponible en: www.guiasgastro.net. [ Links ]
22. Gimeno García AZ, González Y, Quintero E, Nicolás-Pérez D, Adrián Z, Romero R, et al. Clinical validation of the European Panel on the Appropriateness of Gastrointestinal Endoscopy (EPAGE) II criteria in an open-access unit: A prospective study. Endoscopy 2012;44:32-7. [ Links ]
23. Adelstein B-A, Irwig L, Macaskill P, Katelaris PH, Jones DB, Bokey L. A self administered reliable questionnaire to assess lower bowel symptoms. BMC Gastroenterol 2008;8:8. [ Links ]
24. Aronchick CA. Bowel preparation scale. Gastrointest Endosc 2004;60:1037-8. [ Links ]
25. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344-9. [ Links ]
26. Balaguer F, Llach J, Castells A, Bordas JM, Pellisé M, Rodríguez-Moranta F, et al. The European panel on the appropriateness of gastrointestinal endoscopy guidelines colonoscopy in an open-access endoscopy unit: A prospective study. Aliment Pharmacol Ther 2005;21:609-13. [ Links ]
27. Rai S, Kelly MJ. Prioritization of colorectal referrals: a review of the 2-week wait referral system. Colorectal Dis 2007;9:195-202. [ Links ]
28. Grassini M, Verna C, Battaglia E, Niola P, Navino M, Bassotti G. Education improves colonoscopy appropriateness. Gastrointest Endosc 2008;67:88-93. [ Links ]
29. Akbari A, Mayhew A, Al-Alawi MA, Grimshaw J, Winkens R, Glidewell E, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev 2008;(4):CD005471. [ Links ]
30. Adelstein B-A, Macaskill P, Turner RM, Katelaris PH, Irwig L, Chan SF. The value of age and medical history for predicting colorectal cancer and adenomas in people referred for colonoscopy. BMC Gastroenterol 2011;11:97. [ Links ]
31. Hamilton W. Five misconceptions in cancer diagnosis. Br J Gen Pract 2009;59:441-5. [ Links ]
32. Scottish Intercollegiate Guidelines Network (SIGN). Diagnosis and management of colorectal cancer. Edinburgh: SIGN; 2011. (SIGN publication no. 126). (December 2011). Available at: http://www.sign.ac.uk. [ Links ]
33. Adelstein B-A, Macaskill P, Chan SF, Katelaris PH, Irwig L. Most bowel cancer symptoms do not indicate colorectal cancer and polyps: A systematic review. BMC Gastroenterol 2011;11:65. [ Links ]
34. Cubiella J, Salve M, Díaz Ondina M, Vega P, Alves MT, Iglesias F, et al. Diagnostic accuracy of fecal immunochemical test for colorectal cancer in symptomatic patients: Comparison with NICE and SIGN referral criteria. Colorectal Dis (in press). [ Links ]
35. Rai S, Kelly MJ. Prioritization of colorectal referrals: a review of the 2-week wait referral system. Colorectal Dis 2007;9:195-202. [ Links ]
36. Thorne K, Hutchings HA, Elwyn G. The effects of the Two-Week Rule on NHS colorectal cancer diagnostic services: A systematic literature review. BMC Health Serv Res 2006;6:43. [ Links ]
37. Dua RS, Brown VSF, Loukogeorgakis SP, Kallis G, Meleagros L. The two-week rule in colorectal cancer. Can it deliver its promise? Int J Surg 2009;7:521-5. [ Links ]
38. Chohan DPK, Goodwin K, Wilkinson S, Miller R, Hall NR. How has the "two-week wait" rule affected the presentation of colorectal cancer? Colorectal Dis 2005;7:450-3. [ Links ]
39. McDonald PJ, Digby J, Innes C, Strachan JA, Carey FA, Steele RJC, et al. Low faecal haemoglobin concentration potentially rules out significant colorectal disease. Colorectal Dis 2013;15:e151-9. [ Links ]
40. Oono Y, Iriguchi Y, Doi Y, Tomino Y, Kishi D, Oda J, et al. A retrospective study of immunochemical fecal occult blood testing for colorectal cancer detection. Clin Chim Acta 2010;411:802-5. [ Links ]
41. Paterson WG, Barkun AN, Hopman WM, Leddin DJ, Paré P, Petrunia DM, et al. Wait times for gastroenterology consultation in Canada: The patients' perspective. Can J Gastroenterol 2010;24:28-32. [ Links ]
42. Zafar A, Mak T, Whinnie S, Chapman MAS. The 2-week wait referral system does not improve 5-year colorectal cancer survival. Colorectal Dis 2012;14:e177-80. [ Links ]
43. Hodder RJ, Ballal M, Selvachandran SN, Cade D. Pitfalls in the construction of cancer guidelines demonstrated by the analyses of colorectal referrals. Ann R Coll Surg Engl 2005;87:419-26. [ Links ]
44. Ballal MS, Selvachandran SN, Maw A. Use of a patient consultation questionnaire and weighted numerical scoring system for the prediction of colorectal cancer and other colorectal pathology in symptomatic patients: A prospective cohort validation study of a Welsh population. Colorectal Dis 2010;12:407-14. [ Links ]
![]() Correspondence:
Correspondence:
Pablo Vega Villaamil.
Department of Gastroenterology.
Complexo Hospitalario Universitario de Ourense.
C/ Ramón Puga, 52-54.
32005 Ourense, Spain
e-mail: pablo.vega.villaamil@sergas.es
Received: 03-07-2013
Accepted: 04-12-2013











 texto en
texto en