BACKGROUND
In patients with familial adenomatous polyposis (FAP), prophylatic subtotal colectomy with ileorectal anastomosis (IRA) does not prevent lesions appearing in the rectal remnant 1. When this occurs, endoscopic resection becomes difficult and highly ineffective 2. Therefore, patients are usually treated by additional proctectomy with a permanent ileostomy. Otherwise, endoscopic submucosal dissection (ESD) might be a rescue option. However, these cases remain a challenge even for ESD, due to several drawbacks such as dramatic fibrotic tissue and a hypervascularized area with a difficult access due to the anastomosis (dog ear sign) 3.
CASE REPORT
We present the case of a 42-year-old female with FAP, who was diagnosed two years previously with a 3 cm granular homogeneus lateral spreading tumor (G-LST) that was located in the rectal remnant and extended to the IRA (Fig. 1). The lesion was treated ineffectively in two previous attempts via endoscopic mucosal resection and argon plasma coagulation. The patient was offered the endoscopic option prior to surgery and signed the informed consent prior to the procedure.
The tunnel below the lesion was performed using an Erbejet-2-HybridKnife (Erbe Elektromedizin GmbH, Tübingen, Germany). Therefore, the anastomotic area was reached using this technique, shown as a suture staple line. Subsequently, the staples were removed using a grasper in order to maintain an appropriate dissection plane. Once, the tunnel below the whole lesion was made, the dissection was completed in the retroflex position to achieve the en-bloq resection (Fig. 2). The pathological assessment identified a tubulovillous adenoma with high-grade dysplasia. Unfortunately, one lateral margin was affected by adenomatous tissue with low-grade dysplasia. Therefore, a close endoscopy follow-up 2 months after the resection was performed, which showed a scar with non-residual adenomatous tissue (Fig. 3).
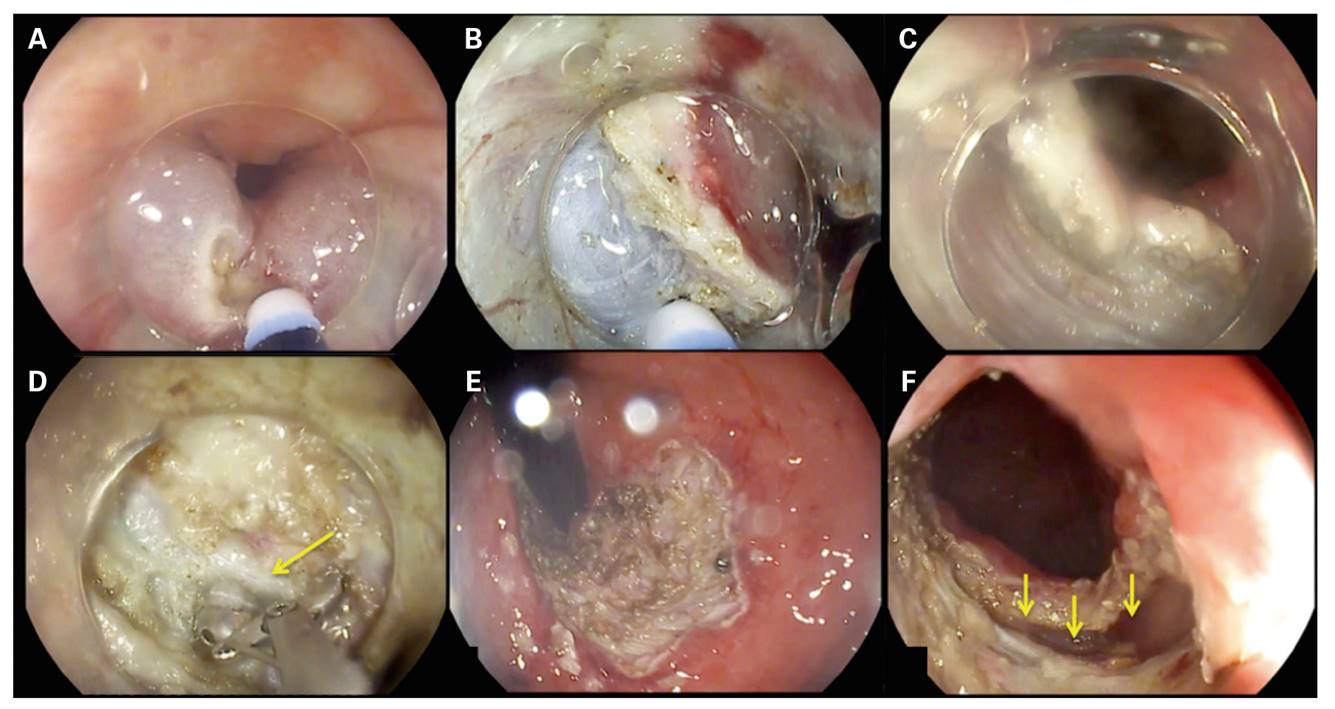
Fig. 2 ESD procedure. A. Initial steps of PCM close to the dentate line. B. Inside the tunnel. C. Tunnel below the whole lesion. D. Removing the staples (yellow arrow) of the Ileorectal anastomosis. E&F. Scar appearance with the ileorectal anastomosis dissected (yellow arrows).
DISCUSSION
ESD as a rescue treatment of dramatic fibrotic adenomas seems to be a suitable approach, especially in areas close to the dentate line. Besides, the anatomy of this area allows us to safely descend the dissection plane, below the submucosal layer. According to our previous reported experience 4, we performed the pocket creation method (PCM) to easily overcome the two expected drawbacks: extreme fibrosis and difficult maneuverability 5.
In order to achieve the en-bloc resection, the ileorrectal anastomosis had to be dissected, which caused a transmural defect (Fig. 2 F) that was closed by second intention healing. These encouraging results overlap with the previous reported experience 3. Therefore, the endoscopic treatment of challenging adenomas (fibrotic, recurrent or large size) located in the rectal remnant, even those affecting the surgical anastomosis, should be attempted. This is due to the fact that the lower rectum is a safe area and also the severe consequences of surgery, especially with regard to quality of life. On the other hand, it is important to underline that the rectal remnant has a poor maneuverability owing to the extreme stiffness caused by the surgery (dog ear sign), which could affect the technical feasibility of the ESD.
In conclusion ESD, especially performed by PCM, allows a complete en-bloc resection, even in difficult scenarios such as extreme fibrotic areas including colorectal anastomosis.
















