INTRODUCTION
The temporomandibular joint (TMJ) is a dynamic structure capable of adapting to mechanical stress to preserve the stomatognathic system's morphological, functional, and occlusal homeostasis1,2,3. It represents a fundamental component in orthognathic surgery because, when performing the movements of the bone segments, it must adapt to achieve satisfactory immediate and long-term results1,2,3,4,5. However, pathological condylar resorption occurs when faced with excessive mechanical stress or when the host's adaptive capacities are diminished or exceeded6,7,8.
Condylar resorption after orthognathic surgery (CROS) is a rare clinical entity that affects the TMJ. It is defined as a progressive alteration of the shape and volume of the mandibular condyles after bilateral sagittal ramus osteotomy, bimaxillary surgery or even Le Fort osteotomy, resulting in a decrease in posterior facial height, progressive mandibular retrusion and anterior open bite, consequently generating an overload of the TMJ3,7,8.
The literature has reported different risk factors for CROS, classified into surgical and non-surgical. In this way, identifying the patient's risk has become essential to determine the treatment plan and avoid a second surgical treatment2,9,10,11.
A clear relationship between the TMJ's morphology, position, and CROS has yet to be established. The determination of CROS risk in the presurgical stage remains unclear due to the diversity of factors involved and the real influence that each of them could imply. The present study seeks to determine variations in the TMJ morphology, between the pre- and postoperative periods, in patients undergoing orthognathic surgery, exposing the condyle's cortical thicknesses and the measurements of its joint spaces for the different operative times.
MATERIAL AND METHODS
A descriptive study was carried out on patients who underwent orthodontic-surgical treatment. The sample was obtained from patients who attended the author's private practice in Santiago, Chile. It included patients between 16 and 60 years old who underwent orthodontic-surgical treatment due to dentoskeletal anomalies and with a minimum follow-up of three months after orthognathic surgery. Patients with previous maxillofacial trauma, history of maxillofacial surgeries, invasive joint disorders, joint ankylosis, articular condyle hyperplasia, hemifacial microsomia and patients who required joint surgery concomitant to orthognathic surgery were excluded. To recruit patients, they were contacted via telephone and email, sending the participants or guardians the proper informed consent and permission for underaged participants. This project was approved by the Scientific Ethics Commitee of the Universidad de los Andes.
Cone-beam computed tomographies (CBCTs) were evaluated in previously recruited patients. These images were obtained in two stages: One month before the orthognathic surgery (T0) and three months after the surgery (T1) to assess adaptive changes in the mandibular condyles. All patients underwent neuromuscular pacification before T0. The images were obtained with ProMax 3D Mid Pro Face equipment (Planmeca®, Finland), with a 70 x 70 cm field of view, a voltage of 90 kV, a current of 12 mA, and a scan time of 24 seconds. All patients sat upright in maximum intercuspation (MIC) for the procedure, with their Frankfort plane horizontal to the floor. The information obtained was reconstructed and analysed in the three-dimensional software HorosTM V 3.3.0.
The same surgical team performed the orthognathic surgery and the bilateral vector manipulation of the proximal segment to locate the mandibular condyle in a centric position in the glenoid fossa. Rigid internal fixation (RIF) was used to fix the bone segments using mini plates and Martin KLS screws, 1.5 and 2.0 systems.
Variables studied were the condylar joint space and its cortical thickness. They were analysed bilaterally at T0 and T1. A method described by Ikeda and Kawamura4 was used to evaluate the join's space, through which linear measurements were made on sagittal cuts of the patient TMJ's CBCTs. A horizontal line was drawn as a reference plane at the uppermost point of the glenoid fossa. Two lines, tangent to the condyle's most anterior and posterior aspects, were drawn from the same point. The distances, in millimetres, from the anterior and posterior points to the mandibular fossa corresponded to the anterior (AJS) and posterior (PJS) joint spaces, respectively. The distance from the highest point of the condylar head to the highest point of the mandibular fossa on the horizontal line corresponds to the superior joint space (SJS) (Figure 1). The cortical thickness was determined by measuring the width, in millimetres, of the TMJ's cortical bone in all three planes of space. Equidistant points were measured for each plane. In the sagittal plane (Figure 2A), five points were determined: anterior (A), anterosuperior (AS), superior (S), superoposterior (SP) and posterior (P). For the coronal plane (Figure 2B), five points: lateral (L), superolateral (SL), superior (S), superomedial (SM) and medial (M). Finally, for the axial plane (Figure 2C), eight points were determined: lateral (L), anterolateral (AL), anterior (A), anteromedial (AM), medial (M), posteromedial (PM), posterior (P), lateroposterior (LP). All sites that presented total resorption of their cortical thickness (0 mm) were grouped based on their initial thickness (on T0). The groups were divided into four: "[0-0.4 mm)", "[0.4-0.8 mm)", "[0.8-1.2 mm)" and "≥ 1.2 mm".

Figure 1. On the sagittal plane: AJS (anterior joint space), SJS (superior joint space), PJS (posterior joint space).

Figure 2. A: on the sagittal plane: A (anterior), AS (anterosuperior), S (superior), SP (superoposterior), P (posterior). B: on the coronal plane: M (medial), SM (superomedial), S (superior), SL (superolateral), L (lateral). C: on the axial plane: A (anterior), AL (anterolateral), L (lateral), LP (lateroposterior), P (posterior), LM (lateromedial), M (medial), AM (anteromedial).
For the statistical analysis, STATA software (V16.1) was used. Descriptive statistics were obtained with their averages, standard deviations, and ranges. Variables were analysed, defining two periods: preoperative (T0) for measurements taken from the CTs one month before orthognathic surgery and mediate postoperative (T1) for measurements taken three months after surgery. Shapiro-Wilk test was used to determine the normality of the data and paired t-test was used to determine statistical differences between the different periods. P-value < 0.05 (95 % CI) indicated significant differences.
RESULTS
The sample comprised 29 patients diagnosed with a dento-skeletal anomaly who underwent orthodontic-surgical treatment between October 2015 and December 2019. The average presurgical orthodontic treatment was 26 months, while postsurgical treatment was six months. Of the total of patients, 19 (65.5 %) were women, and 10 (34.5 %) were men; the mean age was 25 ± 7.4 years (range 16-60 years). The patients were categorised according to their skeletal class in class II (15 patients, 52 %) and class III (14, 48 %). The variables studied were evaluated in both TMJs (right and left) of the 29 patients.
A total of 58 TMJs were analysed, accounting for 1044 studied sites. Of the total sites surveyed, 1017 (97.4 %) showed remodelling of their cortical bone, while 587 (56.2 %) showed a decrease, and 52 (4.9 %) sites suffered total resorption of the cortical thickness between both operative times.
Of the 52 sites that underwent total resorption of their cortical thickness, 21 presented an initial thickness at T0 between 0-0.4 mm, 20 between 0.4-0.8 mm, ten between 0.8-1.2 mm, and one had more than 1.2 mm of cortical thickness in T0. Table I shows the detailed frequency distribution for each of the groups.
No statistically significant changes (p > 0.05) were found for both cortical thicknesses or joint spaces when comparing male and female subjects.
Table I. Sites with total resorption grouped according to their initial (T0) cortical width.

fia:simple frequency.
Fib:cumulative frequency.
hic:relative frequency.
Hid:relative cumulative frequency.
In the coronal plane, a mean decrease in cortical thickness was observed between T0 and T1 in the L, SL, S, and SM sites. Being statistically significant (p < 0.05) for the sites SL (p = 0.016), S (p = 0.002) and SM (p = 0.038). At site M, on average, maintenance of cortical thickness was not statistically significant (p > 0.05) between both operative times. The site with the most significant decrease in cortical thickness between both operative times was the S, with an average of 0.151 mm.
In the sagittal plane, sites AS, S, SP and P presented decreases in their cortical thickness, statistically significant (p < 0.05) for sites S (p = 0.049), SP (p < 0.05) and P (p = 0.001). In contrast, maintenance of cortical thickness was observed in site A without statistical significance (p > 0.05).
Finally, AL and A sites showed a gain in their cortical thickness in the axial plane. On the other hand, the sites L, AM, M, PM, P and LP showed a loss in their cortical thickness between both operative times. However, none of the results was statistically significant (p > 0.05). The data on the variations in cortical thickness for all planes of the space are summarised in Table II.
Table II. Cortical width variations.

aSites:Anterior (A), Anterosuperior (AS), Superior (S), Posterosuperior (PS), Posterior (P), Lateral (L), Anterolateral (AL), Anteromedial (AM), Medial (M), Posteromedial (PM), Posterolateral (PL), Superolateral (SL), Superomedial (SM)
bMean difference:Variation in cortical width between pre- and postsurgical stages (T0 and T1).
*P-value < 0,05.
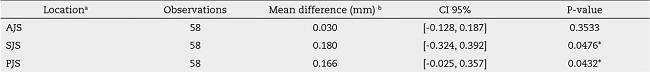
Table III shows the summary of the data corresponding to the changes in the joint space. All the spaces (AJS, SJS and PJS) showed an average decrease in their thickness in the sagittal direction, being more significant for SJS (0.178 ± 0.08 mm) and PJS (0.166 ± 0.07 mm) and to a lesser extent for AJS (0.03 ± 0.06 mm). Of the data shown, only the first two showed to be statistically significant (p < 0.05).
DISCUSSION
The TMJ is a dynamic structure capable of adapting to internal and external stimuli due to its anatomical and histological characteristics5,12. In the present study, bone remodelling of the condylar cortex was observed in all patients. These changes were consistent with the literature, in which remodelling due to mechanical stress is reported in orthodontic-surgical management to treat dentofacial anomalies13.
Changes in the position of the condyles have been mainly related to the fixation system used during surgical treatment and the surgeon's ability to control the proximal segment when performing the bilateral sagittal ramus osteotomy, primarily to avoid excessive stress generated by compression and torsion of the proximal segment, prolonged malposition of the mandibular condyle in its respective fossa and increased perimandibular muscle tension11,14. However, if the articular surface is remodelled or undergoes resorption seems to be related to the adaptation capacities of the TMJ of each individual, making the presurgical imaging evaluation of the TMJ essential when planning surgery, especially in patients who show some of the risk factors for condylar resorption, such as hyperdivergent craniofacial biotype, female gender, temporomandibular disorders, among others1,2,3,4,8,9,10,,11,12,15). Gateno et al.7 showed a significant decrease in the joint space in patients with anterior disc displacement. The magnitude of the condylar movement was considerably greater towards the posterior space than the superior space. To these findings, the pre-surgical evaluation of the articular disc using magnetic resonance imaging (MRI) is suggested in patients with signs of disc displacement who show a decrease in their superior and posterior joint space.
Notably, sites with the most significant loss of cortical thickness were correlated with those presenting a substantial decrease in the width of their joint space, suggesting a possible relationship between these variables. In turn, a predisposition was observed for sites with lower initial cortical thickness to undergo total resorption, which speaks of a potential decrease in the protective role of the TMJ's cortical surface in patients with smaller cortical widths. Before condylar resorption occurs and the joint space increases, an intermediate reduction seemed to take place. Associated with this remodelling stage, and in case of surpassing the mandibular condyle's capacity to adapt, its surface could go on to a subsequent resorption stage with a consequent increase in joint space11,13,15 Despite the unexpected results, we realised the tremendous adaptive capacity of the temporomandibular joint since small morphological changes would not lead to irreversible functional or aesthetic alterations. It would be essential to analyse the cortical thickness and the variation of the joint space with a longer follow-up time of at least a T2 of six months and a T3 of one year.
Even though significant results were seen, none of these had a clinical impact, for none of the patients developed any changes in their occlusion or the dynamic of their TMJs.
This research, however, is subject to several limitations. We only accounted for a limited number of study subjects, giving us a limited number of TMJs to study. The number of studied TMJs could have affected the significance of our results, considering how changes are most commonly seen in the TMJs of female patients10,7, which in our case didn't show any significant results when comparing both genders.
Given the descriptive nature of the present study and the results obtained, it is suggested to continue with lines of research that evaluate the relationship that the variations of the studied parameters could be generating on the genesis of the resorption of the articular surface, also considering qualitative aspects such as the presence of osteophytes and subchondral cysts, and whether these could eventually be considered as predictive factors of its development-considering the low cost and the relatively easy access to CBCTs14, the presurgical evaluation of the temporomandibular joint plays a fundamental role in avoiding possible condylar resorption in patients who will undergo orthognathic surgery.