Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de la Sociedad Española del Dolor
versión impresa ISSN 1134-8046
Rev. Soc. Esp. Dolor vol.27 no.2 Madrid mar./abr. 2020 Epub 25-Mayo-2020
https://dx.doi.org/10.20986/resed.2020.3729/2019
ORIGINALS
Ethical problems in the management of pain. Qualitative study through open reflection interview
1Unidad de Cuidados Paliativos, Servicio de Medicina Interna, Hospital Universitario Virgen Macarena. Sevilla, España.
2Unidad de Farmacología Clínica, Unidad del Dolor, Hospital General Universitario de Alicante. Alicante, España.
3Servicio de Oncología y Cuidados Paliativos, Fundación Rioja Salud. España.
4Unidad de Dolor, Servicio de Anestesiología, Hospital Povisa. Vigo, España.
5Unidad de Dolor y Cuidados Paliativos, Hospital Universitario 12 de Octubre. Madrid, España.
6Unidad de Dolor, Servicio de Anestesiología, Hospital Bellvitge. L'Hospitalet de Llobregat, Barcelona, España.
Introduction:
The medical practice in the area of pain associates ethical problems in the care of patients with a disease that causes a functional deterioration, with an uncertain prognosis for their labor reintegration, and a great consumption of family and social resources. After the creation of a working group on bioethics within the Spanish Pain Society (SPS), an attempt is made to analyze these problems.
Objective:
To know which are the ethical problems that identify professionals (clinical practice, environment and institutions) which concerns SPS members; encouranging an ethical reflection.
Methodology:
Qualitative study, based on a semi-structured, open interview, send to members of the SPS (n = 1035), through electronic access, on 4 bioethical aspects: the problems detected in clinical practice, the problems of the work environment, the problems in the work organizations, and possible suggestions. These are grouped as they refer to the indications (beneficence and non-maleficence), justice (understood as equity), autonomy (information and preferences).
Results:
A total of 6 % professionals participated in the interview (n = 62/1035). A panel was prepared with the 10 main issues identified. They emphasize the uncertainty in the taking of decisions in the therapeutic, the limitation of the therapeutic effort, the conditioning of the sanitary system, the relations with the pharmaceutical industry and the search of the excellence.
Conclusions:
This qualitative study allows identifying ethical problems that interest professionals dedicated to pain. It is convenient to confirm and size them through quantitative studies.
Keywords: Professional ethics; pain management; qualitative research; basic principles of bioethics
INTRODUCTION
Pain is a global health problem, underestimated for decades, and in Spain it affects 20 % of the adult population chronically. Despite the fact that about half of the patients receive some analgesic treatment, 64 % cannot control it 1. In them, quality of life has become an indicator of the evolution of their health condition, as an expression of their vital functioning in relation to their goals, expectations, values and interests.
Pain medical practice raises ethical problems in the care for patients with a disease that causes impairment of functionality, with an uncertain prognosis for their reintegration into productive life, and with a large consumption of family and social resources. It is important that the patient can participate in decision-making in a rational way, and not under the influence of ignorance, irrational ideas, or fear 2,3.
The decision of an adult and competent patient to refuse to be treated must be respected, in consistency with their values (principle of autonomy). This may be in conflict with values and duties of the professional, such as the duty to safeguard life and seek the good of the patient (principle of beneficence), not committing the crime of omission (duty to assist), the obligation of do no harm (principle of non-maleficence) 4, or the duty to guarantee equitable accessibility (principle of justice) . These and other problems interest and concern professionals.
The Spanish Pain Society ((Sociedad Española del Dolor, SED) has multidisciplinary active members (n = 1035), among which there is a majority group of anesthesiologists working in pain units (n = 365), in addition to pharmacologists, rehabilitationists, psychologists, internists, family doctors, physiotherapists, nurses, neurosurgeons and other professional profiles. This society has created an Interest Group and a Bioethics Working Group (GT BioSED). Its main objectives are to sensitize the scientific society and the whole society about the ethical aspects related to pain, promote training in bioethics and promote the development of scientific studies on bioethics and pain.
Following the scientific method, the first task of the group is to analyze the ethical questions and problems that the members perceive and are interested in. To investigate issues related to ethical attitudes, values and duties, the qualitative research approach is highly appropriate 5. In this way, the reflective interview allows to show emotions and thoughts related to situations that we live. It allows us to go deeper into the judgments we make about these situations and discard some prejudices. It facilitates a deeper knowledge of reality 6 and provides a deeper meaning 7,8 to the experience, which can later be transformed during practice 9,10. When the reflection is expressed in writing, it provides information about the workplaces from which it is written, and the character and values of the participants 11. Ethical reflection should help to respond to the needs for transformation of work and professional processes.
Objectives: The main objective of this study is to understand the ethical problems related to pain management (in clinical practice, its settings, and the institutions where the professional members of the SED work and that interest or concern them). As a secondary objective, the present study aims to foster reflection on ethical problems in these professionals interested in pain management.
METHODOLOGY
A qualitative approach has been used, through a semi-structured interview, with open questions that invite reflective writing. All SED members (n = 1035) were invited to participate, through a link that leads them to the survey-interview. The invitation was accompanied by a short cover letter, and it was sent on September 9, 2016, by email from the SED technical secretariat. A deadline of 2 weeks was offered to answer it, and a reminder was sent 48 h before the deadline.
The interview consists of 4 open-ended questions, and there were no instructions that limited or closed the way to answer them. Open-ended questions make it possible to detect areas of interest for members in a broad way, although it requires subsequent synthesis work to establish priorities. For this synthesis, we now group the answers to the questions in 4 blocks, according to whether they refer to the indications (beneficence and non-maleficence), justice (equity), autonomy (information) or others.
The semi-structured interview
The interview asks professionals about ethical problems in pain management, in 3 spheres: (i) problems they find in their clinical practice, (ii) problems they observe in their settings and (iii) problems they identify in organizations where they work. Furthermore (iv), possible suggestions are requested from the GT BioSED. There are 4 different ways of inviting reflection and expression of the ethical problems that interest them. In fact, the survey was a questionnaire with 4 open questions to allow paragraphs and free text that we would later analyze. The 4 questions were: 1 In your daily practice, which ethical problems or questions make you doubt?; 2 In your professional and work environment, which issues do you think deserve ethical reflection?; 3 In the organization in which you work, which ethical issues should be considered most?; 4 Do you have any suggestion for the BioSED GT?
The following steps were followed to prepare the questionnaire: 1. Design of a questionnaire. Unlike other surveys aiming to list the explored problems, we propose an open questionnaire that invites reflection. 2. Test. The interview questionnaire was sent to 10 professionals not included in the study, to identify if it is understood and if the results respond to the objective for which it was prepared. 3. Selection of the participants. Sampling is not necessary; the purpose is not to achieve statistical representativeness. Participants must contribute with information; they should be accessible and motivated. 4. Sending of the interview questionnaire through a mailing to all SED members, with an information sheet requesting their participation.
Exploratory analysis of responses
Two researchers read the reflections submitted by the participants separately, without a predetermined way to classify them. They wrote headlines to summarize the key contents of the reflections, and made a list of categories. They synthesized the long texts highlighting the mentioned ethical problem, checking the number of times it was repeated. They broke down the paragraphs that refer to various ethical problems, and recorded separately if there is repetition of ethical problems to facilitate the observation of the futility of the detected issues.
Then, these syntheses were grouped with higher order headings, under which those that allude to similar problems are joined. It was decided to group them into 4 headings related to the categories of Jonsen's ethical deliberation methodology and ethical principles. Jonsen's method invites to analyze the ethical-clinical problems analyzing the situation from 4 aspects: the indications section is related with the principles of non-maleficence and beneficence; the preferences section is related to the principle of autonomy, for which it requires analyzing information and capacity; the quality of life section is related to the principle of beneficence; and the contextual features section deals mainly with equal justice.
The synthesis and grouping task was performed independently by 2 reviewers, and it was agreed with the help of a third reviewer. In total, the 10 most frequent ethical problems were selected, with a minimum of 2 for each group (indications, justice, autonomy, other aspects). This was the criterion for assigning the importance of the detected issues, apart from the number of times mentioned. A group meeting was held to share the results. Because they were free-text questions, in some cases, the same answer could include 2 different aspects according to the ethical principle. In these cases, it was decided that they would be assigned to the section most consistent with the rest of the answer.
RESULTS
A total of 6 % of professionals who received the interview participated (n = 62). No age, gender or profession was recorded. They present, under the aforementioned headings, the syntheses of the reflections on the ethical issues present in the reflections of the participants, which they perceive both in their daily practice and in their work environment, in the organizations in which they work, or in the suggestions to the research group. The concordance between researchers after the classification and consensus process was complete.
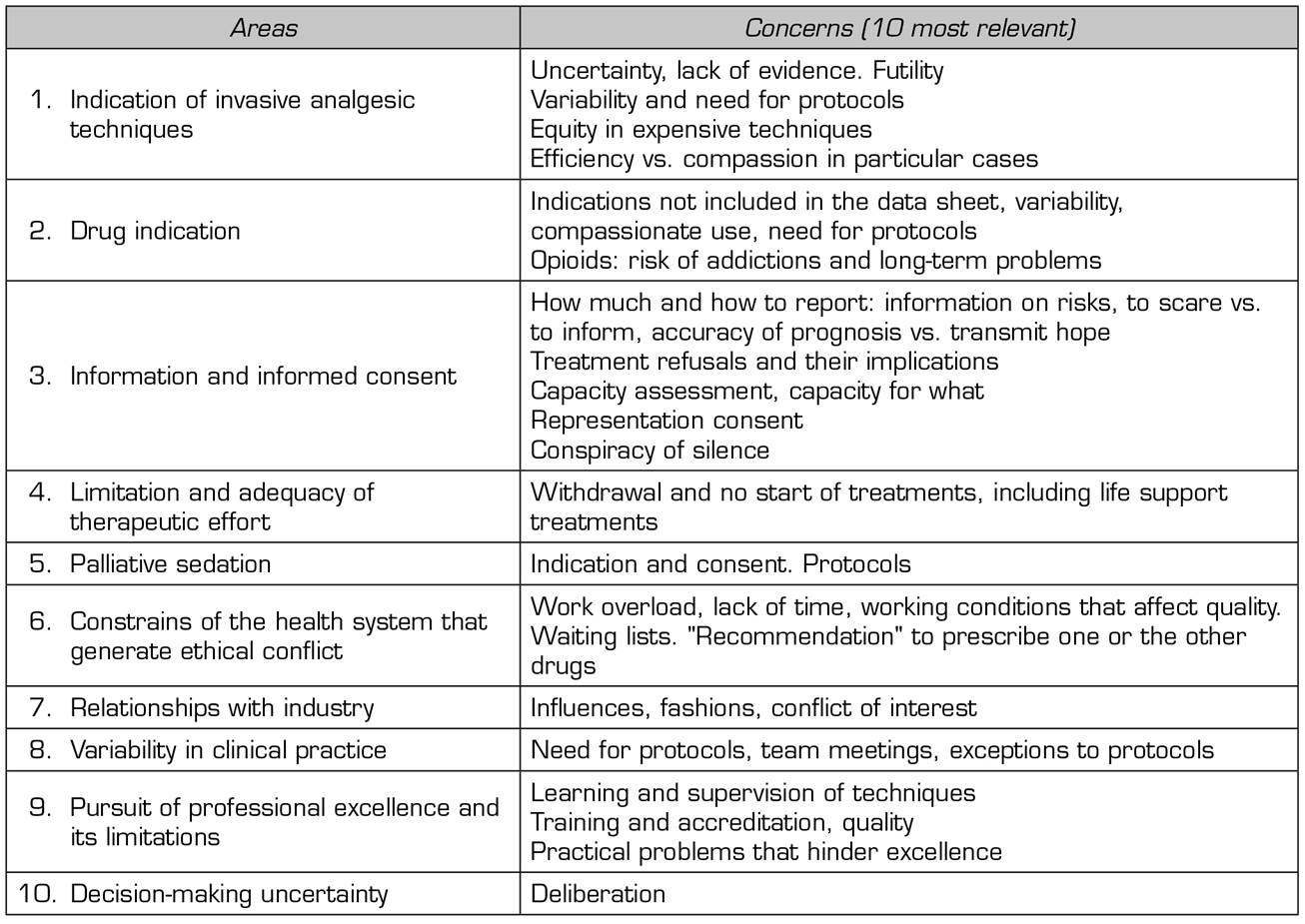
Table 1 summarizes the reflections that concern all bioethical principles. The synthesis of the 10 most relevant ethical questions (concordance, reliability, interpreting results among researchers) most mentioned in the reflections of the participants is presented in Table 2.
Table 1. Main ethical problems (controversial issue to be solved or explained) mentioned by the participants

Principles of beneficence / non-maleficence (indications, quality of life)
The synthesis of ethical reflections on indications based on the principles of beneficence and non-maleficence is shown below.
In the daily practice: Regarding invasive techniques, 9 comments raised questions about the variability in the indications, the uncertainty about their effectiveness, and the conflict between trying to alleviate pain in a patient at all costs versus having to be efficient. The need for protocols was raised. The question of when to stop treatments and what alternatives to propose to avoid abandoning the patient was a concern.
Regarding drugs, 10 comments raised problems with opioid use: prescription and management, identification of malpractices, use of rapid-release opioids with the possibility of addiction and abuse (which is of more concern in young patients with pain cancer), and the indications of drugs not included in the data sheet and for compassionate use.
Regarding the care of patients with advanced or terminal diseases, 9 comments were obtained on limitation or adequacy of therapeutic effort, palliative sedation, attention to the vegetative state, difficulties for analgesia in dementia, influence of family members, and how far to go in applying techniques.
In the workplace: Five comments mentioned the "primum non nocere". They raised the problems of applying invasive techniques that may be futile, in a context of insufficient evidence, and the need to establish unified protocols that avoid inequality and favor patient safety. Polypharmacy was also a concern. Errors due to confusion between pain and suffering, the problem of rentier patients, the need to review and adjust the dose to the needs, and conflicts with the potential inappropriate use of opioids were mentioned. Problems regarding end of life, limitation of therapeutic effort, and palliative sedation were mentioned in 7 comments.
Regarding organizations: Six comments reflected on the promotion of professional excellence, good treatment, empathy, emotional support in public health. The limitation and adequacy of therapeutic effort, the possibility of therapeutic obstinacy and palliative sedation were of concern.
As a suggestion for the bioethics group, awareness of organizations and conduction of training activities on treatments not included in the data sheet and of compassionate use, comprehensive assessment and palliative care were suggested.
Principle of justice (contextual features)
In daily practice itself: Six comments mentioned waiting lists and healthcare pressure, which prevent good clinical practice. They were concerned with prioritizing appointments, cancer patients, those who live far away, and after-hours patient care. Five comments mentioned the possible influence of the industry on the use of new drugs and the possible conflicts of interest. The conflict on the indication of a drug or practice other than those recommended by the health system was also a concern.
In the workplace: Nine comments mentioned the need to raise awareness among professionals and the health system regarding the drama of chronic pain, its consequences and the need for a comprehensive approach. Six comments addressed the problem of waiting lists and healthcare pressure, with insufficient time for comprehensive care. Four comments elaborated thoughts on ethical aspects of working conditions and the risk of burnout. Five comments on the need for training and knowledge management raised, among others, the need for expert help and supervision to perform the techniques. Four comments showed concern about the influence of the pharmaceutical industry and conflicts of interest.
Regarding organizations: Six comments addressed the need for coordination, at the regional level (pain plans), in hospitals (pain committees), between the different services and with primary care, and within each service or unit (sessions, protocols). Eight comments mentioned waiting lists and how to prioritize care and follow up in response to this delay. Five commented on the problem of treatment costs, the conflict they pose in private medicine and public health. Three addressed the respect, dignity and non-discrimination of patients due to distance, age or mental health, and 2 comments mentioned insufficient psychological support.
There is also concern about the need for training in techniques and the possibility of performing them with expert help, and vacation replacements.
As suggestions to the group, 4 comments proposed an ethical thought on the saturation of the health system. Three proposed to request more material and human resources. Six mentioned the need to act according to protocols and guidelines, to evaluate their efficiency and quality, and to consider exceptions. Four suggested evaluating the level of evidence of frequent practices in pain and palliative care units. Three suggested to develop a code of good practice in relation to the industry. They also suggested teaching self-control strategies to separate the pressure and external influences from patient's interest, mentioning the problem of the rejection of treatments due to beliefs, and they insist on the need for specialization.
Principle of autonomy (preferences)
In daily practice itself: Four comments mentioned the information given to the patient about analgesic techniques and drugs, their expectations on efficacy, risks and side effects, and the degree of information given to cancer patients. Six comments concerned the assessment of competence and consent by representation (in minors, disability, in family disagreements, etc.).
In the workplace: In 8 comments, the problem of hiding information from the patient and the patient's right to make informed decisions were of concern.
Regarding organizations: Four comments addressed the need to inform patients and 2 commented on confidentiality and privacy.
As suggestions to the group, 3 comments suggested to elaborate thoughts on the information to the patient in the informed consent.
DISCUSSION
The qualitative method used is a variant of an in-depth interview, using a reflective open survey, and its main drawbacks are that the analysis of the results is laborious for the researchers and that it does not facilitate mass participation. Still, it offers clear advantages for investigating not just perceived facts. It facilitates the expression of the professionals' reflections on their experience, and the expression of emotions and thoughts related to the situations experienced, helping to identify the conflicting values and the duties identified by the professionals, which are the fundamental content that studied by bioethics according to Professor Gracia 12,13. This method facilitates the expression of the professio)nals' reflections on their experience, and the expression of emotions and thoughts related to the situations experienced, helping to deepen the ethical problems that these situations pose.
Despite the low number of responses, around 6 % of members, participation was sufficient to find saturation on issues and problems identified, repeated in numerous answers sent by experts and motivated professionals, which is shown by their answers to the questionnaire and in the content of their answers. Statistical representativeness is not intended.
This qualitative approach should be completed with a new study with a quantitative approach, through a closed survey of the contents detected in this first one, since the open-reflection interview explores understanding the beliefs and values of the interviewee, and a focus group methodology would provide more information, by grading the importance of the responses by virtue of their frequency, evidence and consistency. This would offer more rigor in the interpretation of the results.
In the ethical questions explored, problems such as uncertainty in therapeutic decision-making, the limitation of therapeutic effort, the conditions of the health system that include, the search for excellence, or relationships with the pharmaceutical industry are appreciated. These emerging problems are similar to those found by other authors 14,15. In the future, they will be categorized by type of pain (for example, acute, postoperative, chronic, oncologic or not), because perhaps the management of ethical issues may differ for each type, especially in potentially more preventable cases, such as acute postoperative pain.
Regarding the principle of autonomy, many comments refer to problems related to information and capacity and informed consent. The autonomy of the patient is not respected if it is considered a priori that he does not possess it or is diminished because of his illness, his opinions and wishes are not taken into account, and the details of his condition are hidden from him, forgetting that his preferences and values are paramount.
Regarding the indications (principles of beneficence and non-maleficence), the variability in the indications of invasive techniques raises a conflict of justice (inequity), which is mentioned in various ways. Uncertainty about the effectiveness of a technique is increased by insufficient evidence, and it is reflected in the problems of the environment rather than in clinical practice itself, motivating reflection on the need for protocols to avoid doing harm ("primum non nocere"). There is also a conflict between beneficence and justice, due to the obligation to be efficient in the interest of sustainability. The ambition for professional excellence and the search for patient safety lead to the need for expert help and supervision to perform the techniques. Concern about when to stop ineffective treatments is accompanied by comments about the duty not to abandon the patient when the therapeutic arsenal is depleted.
Regarding drug indications, the concern about opioids was highlighted (opioid use in general), the possibility of addiction and aberrant use, and prescriptions not indicated in the data sheet, especially in new ultrafast-acting opioids, which have a larger addictive potential and its indication in the technical sheet is only for patients with opioid-controlled base pain. This concern about opioids has been reported in some studies 16, but others seem to deny this topic. In clinical practice, it is recommended to assess the predictive factors of addictive behavior such as the positive Cage test 17.
Controlled studies on potential indications other than those included in the data sheet will be needed, as well as promoting training activities that favor dialogue and consensus, and eliminate prejudice. It is not possible to be beneficent if pain cannot be alleviated due to lack of rigorous and up-to-date theoretical-practical training, and maleficence occurs when someone, instead of refraining from doing harmful actions, refrains from alleviating pain by not providing the most suitable treatment. Pain relief is implicitly linked to the quality of patient care, and the professional has an ethical duty to try to do so, with the available resources and adequate knowledge, and for this, good communication with the patient is needed 18.
Regarding indications for advanced and terminal diseases, the main ethical questions arise regarding palliative sedation and the limitation or adaptation of therapeutic effort (in a broad sense, which includes not only life support measures, but also other treatments). There is a relationship between the two, since the limitation of invasive techniques can lead to considering pain as a refractory symptom, which is a criterion for palliative sedation. These will be questions on which to deepen training activities, and several comments raise the need to sensitize organizations and services about them, as well as the need for empathy and respect.
Regarding the principle of justice (equity), waiting lists and healthcare pressure are the most frequently mentioned problems, both with regard to the clinical practice of the participants, as well as in their environment and in organizations. There is concern about setting priorities in appointments, especially in cancer patients, and there are complaints about the saturation that comes from citing extra patients, after hours, during guards, etc. with the consequent risk of burnout. The pressure of care is related to insufficient time to perform a comprehensive assessment and provide psychological support. The conflict regarding the indication of drugs or techniques other than those recommended by the health system, generally with criteria of efficiency and sustainability, which may require justified exceptions, is also of concern.
Numerous comments on the need for training that favors the accessibility of the patients to the best treatments refer to justice. Programs for the study of pain during the training of health professionals are insufficient. It is not fear to consider that there is nothing left to do in patients with difficult pain and the necessary resources to alleviate their suffering are not available, in the same way that it would be performed with other types of diseases. Several thoughts deal with the influence of the pharmaceutical industry, which may condition the indication of new and more expensive treatments, and conflicts of interest. The costs of treatments pose ethical conflicts in private medicine and also in public health (sustainability / beneficence).
Thoughts pointing to the need for coordination at the regional and local levels also allude to equity, which is also raised in other studies on pain18 and in other fields of medicine between different services and primary and specialized care. The main suggestion in this regard was the thought on the saturation of the health system, with the need to adapt and make profitable material and human resources, act according to protocols and guidelines based on evidence, and evaluate its efficiency and quality.
Regarding research, there was concern about how to propose cancer patients to be included in trials, and the guarantee that control groups receive at least standardized treatment. They propose creating information sheets on frequently asked ethical questions when designing studies, developing a minimum plan of ethical requirements for a study, a new technique, or a change in clinical practice. They propose to complete this study with a quantitative descriptive study using a survey with closed questions, and to elaborate a bioethics guide of the SED.
CONCLUSIONS
Professionals dedicated to pain management in Spain are concerned about ethical problems related to uncertainty in the indications, especially regarding invasive and expensive techniques, and the risk/benefit of the use of certain drugs, especially opioids and for indications not included in the data sheet.
They are interested in problems related to information and the capacity for informed consent.
Regarding advanced and terminal diseases, they are challenged by the conspiracy of silence and decisions to limit therapeutic effort, refusal of treatments and palliative sedation.
They express their concern for equity and to avoid variability and discrimination, the pursuit of professional excellence, and constraints due to restrictions imposed by healthcare organizations, waiting lists, and the influence of the industry.
This first approach was qualitative, and it should be completed with a descriptive study using a questionnaire. It will be useful to take these results into account for drafting the questionnaire. The training and awareness activities on bioethics for SED members should consider these results in the design of their teaching objectives, content and methodologies.
ACKNOWLEDGMENTS
To Prof. Diego Gracia Guillén, who has promoted the development of this working group. To all members of the SED bioethics interest group.
REFERENCES
1. Carmona L, Ballina J, Gabriel R, Laffon A; EPISER Study Group. The burden of musculoskeletal diseases in the general population of Spain: results from a national survey. Ann Rheum Dis. 2001;60(11):1040-5. DOI: 10.1136/ard.60.11.1040. [ Links ]
2. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287-333. DOI: 10.1016/j.ejpain.2005.06.009. [ Links ]
3. Katz N. The impact of pain management on quality of life. J Pain Symptom Manage. 2002;24 (1 Suppl):S38-47. DOI: 10.1016/S0885-3924(02)00411-6. [ Links ]
4. Remmers PA, Speer AJ. Clinical strategies in the medical care of Jehovah's witnesses. Am J Med 2006;119(12):1013-8. DOI: 10.1016/j.amjmed.2006.04.016. [ Links ]
5. Grupo de trabajo Sociedad Española del Dolor. Bioética [acceso: 28 Nov 2016]. Disponible en: http://www.sed.es [ Links ]
6. De Cossart L, Fish D, Hillman K. Clinical reflection: A vital process for supporting the development of wisdom in doctors. Curr Opin Crit Care 2012;18(6):712-7 DOI: 10.1097/MCC.0b013e328358e239. [ Links ]
7. Plack MM, Driscoll M, Blissett S, McKenna R, Plack TP. A method for assessing reflective journal writing. J Allied Health. 2005;34(4):199-208. [ Links ]
8. Mann KV. Reflection: understanding its influence in practice. Med Educ. 2008;42(5):449-51. DOI: 10.1111/j.1365-2923.2008.03081.x. [ Links ]
9. Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287(2):226-35. DOI: 10.1001/jama.287.2.226. [ Links ]
10. Gracey CF, Haidet P, Branch WT, Weissmann P, Kern DE, Mitchell G, et al. Precepting humanism: Strategies for fostering the human dimensions of care in ambulatory settings. Acad Med. 2005;80(1):21-8. DOI: 10.1097/00001888-200501000-00007. [ Links ]
11. Branch WT Jr, Kern D, Haidet P, Weissmann P, Gracey CF, Mitchell G, et al. Teaching the human dimensions of care in clinical settings. JAMA. 2001;286(9):1067-74. DOI: 10.1001/jama.286.9.1067. [ Links ]
12. Gracia-Guillén D. Teoría y práctica de la deliberación moral. En: Lydia Feito L, Gracia D, Sánchez M, editores. Bioética: el estado de la cuestión. Madrid: Ed Triacastela; 2011. p. 101-54. [ Links ]
13. Gracia D. Deliberation and consensus. En: Chadwick R, ten Have H, Meslin EM, editores. The SAGE handbook of health care ethics: Core and emerging issues. London: SAGE Publications Ltd; 2011. p.84-94. DOI: 10.4135/9781446200971.n9. [ Links ]
14. Anwari JS. Medical ethics and chronic pain management. Saudi Med J. 2008;29(6):921-2. [ Links ]
15. Rich BA, Dubois M. Pain, ethics, and public policy. Pain Med. 2011;12(9):1295-6. DOI: 10.1111/j.1526-4637.2011. 01219.x. [ Links ]
16. Pérez-Castañeda T. Aspectos bioéticos en el manejo del dolor por cáncer [acceso: 12 Mar 2017]. Disponible en: http://www.cbioetica.org/revista/102/102-0914.pdf [ Links ]
17. Kwon JH, Hui D, Bruera E. A pilot study to define chemical coping in cancer patients using the Delphi method. J Palliat Med. 2015;18(8):703-6. [ Links ]
18. Boceta J, de la Torre A, Samper D, Farto M, Sánchez-de la Rosa R. Consensus and controversies in the definition, assessment, treatment and monitoring of BTcP: results of a Delphi study. Clin Transl Oncol. 2016;18(11): 1088-97. [ Links ]
Received: February 23, 2019; Accepted: February 03, 2020











 texto en
texto en