Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Anales del Sistema Sanitario de Navarra
versión impresa ISSN 1137-6627
Anales Sis San Navarra vol.36 no.1 Pamplona ene./abr. 2013
https://dx.doi.org/10.4321/S1137-66272013000100020
Gastric lipoma and pyloric obstruction in a 51-year-old woman
Lipoma gástrico y obstrucción pilórica en una mujer de 51 años
W.S. Furtado1, D.A.C.P.G. Mello1, V.M. Santos2, T.L. Bringel1, W.P. Oliveira Junior1, H.J.L. Moura1
1. General Surgery Division of Armed Forces Hospital, Brasília-DF, Brazil
2. Catholic University Medical Course and Internal Medicina Department of Armed Forces Hospital, Brasília-DF, Brazil
Dirección para correspondencia
ABSTRACT
Gastric lipoma is considered a rare condition that may constitute a challenging diagnosis. A 51-year-old woman presented dysphagia and abdominal pain, and an upper digestive endoscopic study disclosed a gastric tumor located in the submucosa of the pyloric antrum. Conclusive diagnosis was established after repeated endoscopic biopsies, and the patient was subjected to an atypical gastrectomy, which evolved into a pyloric stenosis. This complication was appropriately corrected and the patient remains symptomless, under outpatient surveillance.
Key words: Atypical gastrectomy. Benign tumor. Gastric lipoma. Pyloric obstruction.
RESUMEN
Lipoma gástrico es un hallazgo muy raro que suele constituir un desafío diagnóstico. Una mujer con 51 años presentó disfagia y dolor abdominal; en una endoscopia digestiva superior se encontró un tumor gástrico submucoso localizado en el antro pilórico. Se hicieron biopsias endoscópicas para establecer el diagnóstico. Esta paciente se sometió a una gastrectomía atípica, que ocasionó estenosis del píloro. Esta complicación fue adecuadamente tratada, y la paciente se mantiene sin síntomas con control ambulatorio.
Palabras clave: Gastrectomía atípica. Lipoma gástrico. Obstrucción pilórica. Tumor gástrico benigno.
Introduction
Gastrointestinal lipomas more frequently occur in the colon (60-75%) and the small intestine (up to 31,2%)1-7. Only 5% of them are found in the stomach, which accounts for less than 1% of the gastric tumors, and 2% to 3% of benign tumors of this organ2,4-10. They can be under recognized or misdiagnosed by more common masses5 like gastrointestinal stromal tumor, leiomyoma, fibroma, neurilemmoma, adenomyoma, Brunner's gland adenoma, and heterotopic pancreas2. The first description of gastric lipoma is attributed to Cruveilhier (1842)8. There are only about 220 cases of gastric lipomas described in the literature2,5,8, around 10% are intramural or subserosal, while the vast majority have origin in the submucosa5,7-10. The etiology of lipoma remains unknown2,6,8, and it may constitute an acquired condition or an embryological misplacement6. The tumor is constituted by well differentiated adipocytes with a fibrous capsule, and if sectioned it grossly appears as an yellowish tissue2,3,5,7,10. Although more commonly located in the gastric antrum (75%)2, these tumors may be found at any site of the stomach4-10. Gastric lipoma is a rare benign condition, which may mimic malignancy of the stomach.
Case report
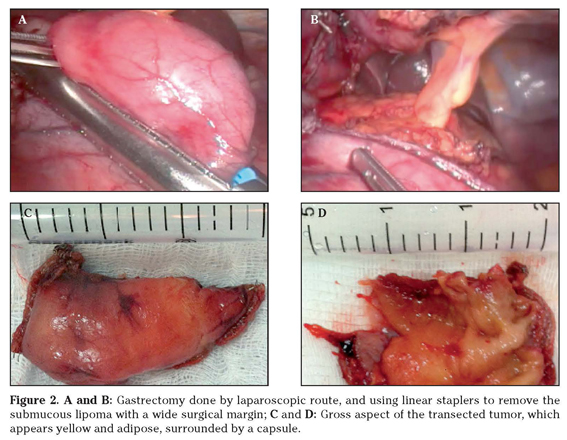
A 51-year-old Brazilian woman was admitted because of a severe epigastric pain associated with episodes of vomiting, dyspepsia, dysphagia and weight loss of 5 kg during 8 months. Her body mass index was 19.81Kg/m2, and the routine laboratory determinations were unremarkable. She underwent three endoscopy studies that disclosed an antral mass with around 3 cm (Fig. 1A-B). PET/CT images revealed a spherical hypoattenuating mass (31 mm x 20 mm) with fat density, without enhanced metabolism, at the antrum; and the ecoendoscopy study found a submucosal homogeneous hyperecogenic mass (27 mm x 20 mm) on the same site. The specimens obtained from two routine endoscopic biopsies revealed normal mucosa. Another biopsy was performed - guided by endoscopic ultrasound, and revealed mature fat tissue at the submucosa, and diagnosis of submucosal lipoma was characterized (Fig. 1C-D). She underwent an atypical gastrectomy by laparoscopic route, and employing linear staplers (Fig. 2A-B) to remove the gastric mass along with a wide free surgical margin. Grossly, the aspect of transected tumor was yellow and adipose (Fig. 2C-D), with a capsule. On the fifth postoperative day, the patient presented with vomiting and dysphagia, and the endoscopic evaluation revealed a pyloric substenosis, corrected by dilation. After an uneventful evolution, she was discharged to home; nevertheless, five days later, she claimed of anorexia and recurrent vomiting, and another endoscopy detected pyloric obstruction. Therefore, the patient was submitted to a pylorotomy, and was discharged to outpatient surveillance on the third postoperative day, asymptomatic and accepting solid foods.
Discussion
This 51-year-old female presented with clinical features typical of gastrointestinal obstruction and her age was in accordance with the mean age of patients at diagnosis of gastric lipomas5,8. However, no specific symptoms could hardly contribute to raise suspicion about gastric lipoma, and the final diagnosis was based on imaging investigation and further histopathology studies. The upper digestive endoscopy showed a submucosal mass measuring about 3 cm in diameter. The first two biopsy procedures did not furnished enough tissue to histopathology analysis, phenomenon that is frequently reported in literature3-5,8,9. The tissue samples from the third biopsy, which was guided by endoscopic ultrasound, revealed the origin of the tumor - a classical lipoma. Surgical approach was done, as most of the authors recommend for symptomatic patients3-5,7-9,11. The occurrence of pyloric stenosis was an expected complication of the atypical gastrectomy, because the tumor resection was performed at the antrum, and with a large free surgical margin. Gastric lipomas predominate in people over than 50 years of age2,5,8,11, and appear as solitary and asymptomatic masses5-10. However, patients with gastric lipomatosis have been reported as an exceeding rare condition12. The symptoms depend on localization and size of the tumor and of associated entities2,7-10. Those lipomas developed at the antrum and the body of the stomach may origin intussusceptions into the pylorus causing obstruction and pain; while voluminous tumors may be associated with venous stasis, resulting in ulceration and hemorrhage6-10. Lipomas larger than 2 cm usually cause symptoms (diarrhea, obstruction, intussusception, hemorrhage)2,4,5,7,10. The most common symptoms are dyspepsia, epigastric pain, upper gastrointestinal bleeding (usually by ulceration and necrosis), obstruction and intussusception3-11. Because of the absence of symptoms, in the vast majority of cases gastric lipoma constitutes an endoscopic finding3,5,6,8,10, and the tumor often appears as a smooth, yellowish submucosal mass with or without ulceration3-5,10. Classical imaging aspects like «tenting», «cushion sign» and «naked fat sign» are useful to diagnose submucosal lipomas.2-7,11 To perform a successful endoscopic biopsy of submucosal lipomas can be a challenging task2,4,5,9. In general, these biopsies only reveal a normal gastric mucosa2,3,6,8,9. The use of electrocautery to elicit a local mucosal ulceration, before the biopsy procedure, might be of some utility5. Computerized tomography (CT) is a highly specific tool that can contribute to diagnosis2,3-9,10. In CT images, the lipoma typically appears as a mass that is isodense (-70H to -120H) with fat3,4,6,7,9,10. Endoscopic ultrasound is useful to diagnosis of gastric lipoma, showing the hyperecoic density of the tumor in the submucosa2,3-10. Gastric lipomas do not have malignant potential2,4-6,9, however, synchronous gastric carcinomas have been very rarely described6,9. Treatment of gastric lipoma, is controversial4,9, but resection is the best choice for symptomatic tumors2-5,8,10. Laparoscopic route is used for tumors up to 6 cm in diameter2,7. Pedunculated lipomas smaller than 3 cm may be excised by upper digestive endoscopy route4,7,8,11, but mere observation is an alternative2,4,7,10,11. Hemorrhages can be treated by endoscopic clipping5.
References
1. Calvo AM, Montón S, Rubio T, Repiso M, Sarasibar H. Invaginación intestinal en el adulto secundaria a lipoma yeyunal. An Sist Sanit Navar 2005; 28: 115-118. [ Links ]
2. Neto FA, Ferreira MC, Bertoncello LC, Neto AA, De Aveiro WC, Bento CA, et al. Gastric lipoma presenting as a giant bulging mass in an oligosymptomatic patient: a case report. J Med Case Rep 2012;6:317. [ Links ]
3. Penston J, Penston V. Gastric lipoma: a rare cause of iron-deficiency anaemia. BMJ Case Rep 2009; 2009. pii: bcr09.2008.0954. Epub 2009 Mar 24. [ Links ]
4. Sadio A, Peixoto P, Castanheira A, Cancela E, Ministro P, Casimiro C, et al. Gastric lipoma - an unusual cause of upper gastrointestinal bleeding. Rev Esp Enferm Dig 2010: 102: 398-400. [ Links ]
5. Saltzman JR, Carr-Locke DL, Fink SA. Lipoma case report. Med Gen Med 2005; 7: 16. [ Links ]
6. Yamamoto T, Imakiire K, Hashiguchi S, Matsumoto J, Kadono J, Hamada N, et al. A rare case of gastric lipoma with early gastric cancer. Intern Med 2004;43: 1039-1041. [ Links ]
7. Zameer M, Kanojia RP, Rao KL, Menon P, Samujh R, Thapa BR. Gastric lipoma. J Indian Assoc Pediatr Surg 2010; 15: 64-66. [ Links ]
8. Kim DD, Tsai AI, Otani AR, Puglia CR, Malheiros CA. Lipoma gástrico: case report. Rev Col Bras Cir 2011; 38: 205-206. [ Links ]
9. Krasniqi AS, Hoxha FT, Bicaj BX, Hashani SI, Hasimja SM, Kelmendi SM, et al. Symptomatic subserosal gastric lipoma successfully treated with enucleation. World J Gastroenterol 2008; 14: 5930-5932. [ Links ]
10. Thompson WM, Kende AI, Levy AD. Imaging characteristics of g 10. DONE HJ. Lipoma of the stomach. Br Med J 1961; 1: 183. [ Links ]
11. Bijlani RS, Kulkarni VM, Shahani RB, Shah HK, Dalvi A, Samsi AB. Gastric lipoma presenting as obstruction and hematemesis. J Postgrad Med 1993; 39: 42-43. [ Links ]
![]() Dirección para correspondencia:
Dirección para correspondencia:
Vitorino Modesto dos Santos
Hospital das Forças Armadas
Estrada do contorno do bosque, s/n
Cruzeiro Novo, 70658-900
Brasilia-DF
E-mail: vitorinomodestos@gmail.com
Recepción: 30 de octubre de 2012
Aceptación definitiva: 21 de noviembre de 2012