Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.17 no.52 Murcia oct. 2018 Epub 01-Oct-2018
https://dx.doi.org/10.6018/eglobal.17.4.311591
Originals
Factors that favor re-entry in intensive patients with acute coronary syndrome
1 Diplomado en Enfermería. Máster Investigación. Hospital Universitario Ntra Sra. de Candelaria. Santa Cruz de Tenerife.España. clementediaz1@hotmail.com
2 Gerencia de Urgencias y Emergencias Sanitarias del 061. Servicio Murciano de Salud. Murcia. España.
3 Universidad de La Laguna. Santa Cruz de Tenerife. España.
Introduction
About 7% of patients admitted in Intensive Care Units (ICUs) due to acute coronary syndrome (ACS) in Spain, are readmitted again later.
Objectives
Identify the possible causes and predisposing factors for returning to ICU because of ACS.
Methodology
Retrospective, descriptive, comparative and longitudinal study of patients admitted for ACS in the ICU between January 2008 and December 2013.Demographic variables, number of admissions, admission risk factors (dyslipidemia, hypertension and diabetes) and non heart-healthy life habits (sedentary / obesity, smoking, alcoholism) of patients who come back were collected and were compared with control group (not readmitted patients). Pearson’s Chi 2 test and statistical significance were performed.
Results
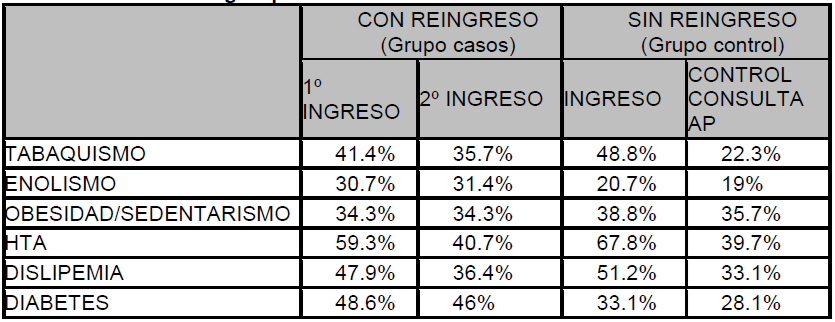
2.506 patients were admitted by ACS. Readmissions were 140 (5,58%) after 12,93±16,41 months from their first admission. The ICU’s reentering patients stayed4.97± 3.3 days (4.03±1.8 control group) in their first admission. A table is attached with risk factors’ incidence and non heart-healthy life habits of both groups. Smoking and alcoholism habits are related with readmissions (χ²=5.67; p<0.01)
Conclusions
The patients who are readmitted stay more days in ICU in their first admission, have less control about risk factors and less quitting index of nocive habits than control group. It seems to exist an adherence therapeutic problem in the sample studied.
Keywords: Re-Entry; Acute Coronary Syndrome; Life Habits; Risk Factors
INTRODUCTION
Ischemic heart disease and strokes are the first cause of death in the world 1 . In Spain, circulatory system diseases are responsible for 30.5% of all deaths, being the most relevant aetiology the ischemic heart disease, which comprehends 8.98% of the total number of deaths with a higher distribution in men 2). Heart attacks represent an expenditure of 250 million euros to our National Healthcare System every year, where 50.000 coronary attacks are registered annually with a 7% of mortality and a re-admission rate of 7% in less than 30 days 3)(4 .
It is been confirmed that patients with several risk factors or previous ischemic heart disease medical history, have a higher risk of suffering a new coronary attack 5 and several studies show that 6-8% of heart attack survivors suffer a new stroke during the following year, having a higher mortality rate than the general population 6 . Hence, an effective secondary prevention program is relevant in this phase.
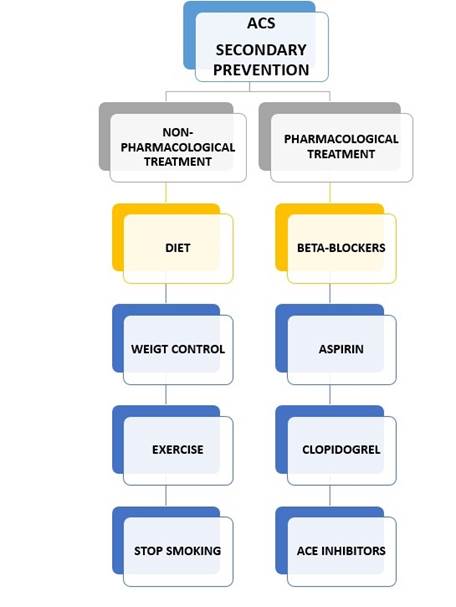
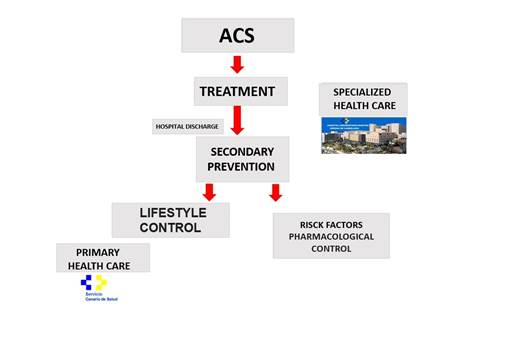
The main goals of this prevention level are to reduce mortality, prevent new cardiovascular events and control the associated risk factors. This secondary prevention includes, on one hand, pharmacological treatment to control risk factors (SAH, dyslipidemias, diabetes) 7 and, on the other hand, education in heart-healthy life habits and encouraging a change of harmful habits (smoking, obesity and sedentariness).
The clinical trial MIRVAS38 has demonstrated in Spain that a comprehensive and intensive treatment of risk factors in cardiovascular disease patients reduces by half the morbidity and mortality 8 . In the Unites States, a meta-analysis has estimated that if the percentage of patients who in 2002 received the recommended treatment in secondary prevention had been of 60%, the subsequent mortality would have reduced to 50% 9 .
According to the Spanish Society of Cardiology, cardiovascular patient training programs are essential for an optimal prognosis because this is a disease which requires the participation of the patient to achieve changes in his life habits and his collaboration in the persistence of the treatment 10 . In this context, Nursery is a key aspect at this level of intervention, as educative agents and advisers to change harmful habits, for acquisition of new heart-healthy habits and to control risk factors as a means to improve the quality of life and avoid new coronary events.
Smoking is strongly associated to heart attacks 11 . Studies have shown that tobacco smoking cessation reduces the mortality by one third compared to those who continue smoking; therefore, it constitutes an effective measure of secondary prevention 12 . Also, it has been demonstrated that diet and reduction of obesity is effective in the control of SAH, diabetes and, hence, in the post-infarction secondary prevention 13 .
Practicing physical activity regularly brings with it a 26% reduction of the risk of mortality in heart disease patients 14 due to induced favourable changes in the platelet function and the fibrinolytic system which, in turn, implies an increase in the activity of the plasminogen caused by a decrease in the levels of its inhibitor 15 .
People are well aware of the benefits of following the described guidelines, but this is not the reality at the coronary unit where this research is being conducted. We have detected that many patients who are re-admitted due to heart attacks have held on to the same harmful habits as they had beforehand and did not want to or did not know how to correctly control coronary risk factors (since their condition upon re-admission was the same as in their first admission). As evident as it is the failure in the secondary prevention, the motivation to conduct this research leads us to establish the following goals:
GOALS
General
Identify possible causes and underlying factors to suffering a new ACS and be re-admitted to ICU.
Specifics
Quantify the proportion of patients who are re-admitted in the unit, number of re-entries, time lapse between them and days of stay.
Verify the degree of fulfilment of the pharmacological treatment.
Describe the degree of abandonment of harmful habits after ACS.
Compare risk factors and life habits in patients who are re-admitted and those who are not.
List cardiovascular risk factors associated to a higher rate of morbidity, mortality and re-admission.
METHOD
This is a retrospective, descriptive and analytic study about control-cases of patients admitted in a polyvalent ICU due to ACS between the 1st of January, 2008 and the 31st of December, 2013. The data is extracted examining the electronic Clinic and Primary Health Care History at the hospital, according to demographic variables (sex, age), number of re-admissions, time lapse between admissions, days of stay, cardiovascular risk factors and life habits previous to the heart attack and during the re-admission. The inclusion criteria in the case group means it is comprised of patients who suffered an ACS and were re-admitted in our unit for this same reason, at least once, during the period of study. The control group is comprised of patients who were admitted in the unit in 2010 but were not subsequently re-admitted during the rest of the study. This particular year is selected because of its convenience, due to the importance of the economic crisis (which might condition the patient’s attitude in relation to the secondary prevention) and because given that the study will be carried out until December, 2013, there is enough time for re-admission, and this would, in turn, be a cause of exclusion of the control group. Statistic analysis will be performed with the statistics application SPSS v.17. The test used for nominal independent variables is Chi 2 test and the level of significance considered is p<0.05. Likewise, re-admission likelihood based on risk factors is verified using the Odd Ratio.
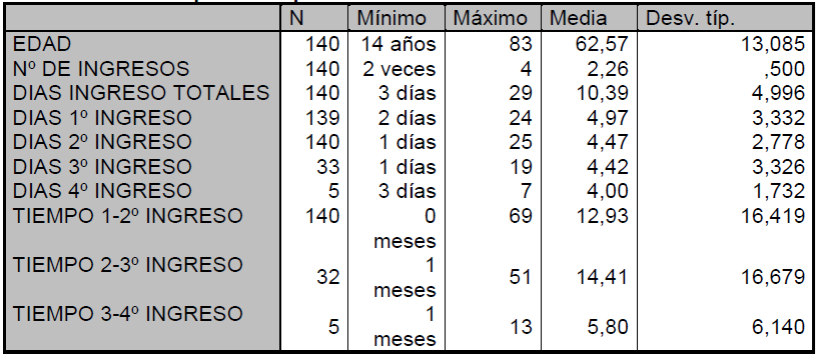
RESULTS
During the period of the study (01.01.2008-31.12.2013) 2.506 patients were admitted to our unit presenting ACS and 140 of them were re-admitted afterwards (5.58%), and the latter constitute the sample of the case group. Most subjects are male (73.6%) with an average of 62.5±13 years old. The mortality rate is 11.4%. 27.14% of re-admissions occurred during the first month after being discharged. 22.85% of the total amount are admitted a third time and 3.57% a fourth time (during the time of the study). The total days of stay in the unit were 10.39±4.9 days per patient distributed in 4.97 days/1st admission, 4.47/2nd admission, 4.42/3rd admission and 4 days the 4th admission. 92.1% of the patients claim compliance with the treatment prescribed by their specialist after their first admission.
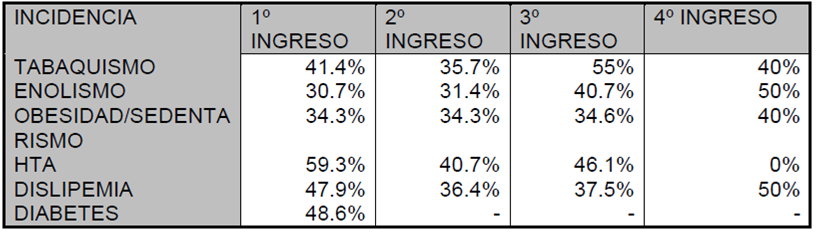
In the case group, 68.7% present some harmful habit (smoking, obesity, sedentary lifestyle, alcoholism) in their first admission, from whom 63.5% (p<0.01) still present them upon re-admission. 82.1% present some cardiovascular risk factor (HTA, diabetes, dyslipidemia) in their first admission but this value reduces to 63.5% in the second one. Only 5% of the sample does not present any risk factor or harmful habits. The influence of cardiovascular risk factors and lifestyle are represented in the following table:
The averages values corresponding to the third and fourth re-admissions are weighted on the number of patients that are re-admitted, therefore, the first and second re-admissions are the ones that should be considered representative because all of the patients from the sample (140 patients) were re-admitted at least once.
The only factor which is correlated with mortality is dyslipidemia. (χ² =4.01, p<0.05 y ODD Ratio= 2.03; IC: 0.88-4.83). HTA shows a bias but it is not significant in this series.
Smoking is correlated with alcoholism habits (active-moderate) (χ² =14.35, p<0.001 y ODD Ratio= 4.16; IC: 1.9-8.9), HTA (p<0.01) and dyslipidemia (p<0.05). In this study, smoking and alcoholism are directly related to re-admissions (χ² =5.67; p<0.01). There’s no relation between re-admission and obesity or sedentary lifestyle.
Age is correlated with HTA and diabetes (p<0.01) and inversely related to tobacco and alcohol (p<0.01).
Regarding the gender, men are more related to tobacco (41.5% vs 22.6%; χ²= 3.29; p=0.06) and alcohol (41.5% vs 16.1%; χ²= 6.09; p<0.05). Women have an obesity/sedentary lifestyle tendency but it is not significant.
Risk factors and harmful habits are not correlated with the time lapse between admissions.
In 17.14% of the cases we find inconsistencies between the harmful habits that they present at the moment of admission in our unit and the Clinic History of Primary Health Care.
In the control group, we take into account all the patients who were admitted in 2010 that were not previously admitted because of coronary events nor were they admitted afterwards earlier than December, 2013. This means that 242 patients were admitted, 73.2 of them were men with an average age of 60.2 ±11 and they were admitted in ICU during 4.03 days of average.
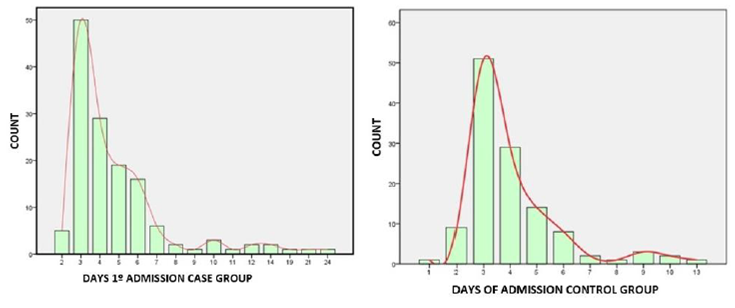
Figures 3, 4 Comparison of the days of the first admission between groups of cases and control group
DISCUSSION
Experience teaches that when a patient with a stroke is admitted in the unit and he feels his life is in danger, usually, he expresses the need to abandon the harmful habits, to reduce his stress level, to eat healthier, to do exercise or control his risk factors. However, in the case group, upon a subsequent re-admission (12.9 months afterwards on average), data shows that few actual changes in their life habits took place.
5.58% of the patients are re-admitted and this figure is lower than the national rate (7%). The difference might be related to the foreign floating population assisted in our hospital 16). This does not mean that fewer patients are re-admitted; it means that many of those patients will be re-admitted in their respective countries of origin in the future.
Other studies show the same demographic data related with ACS: most patients are male and have the same average age 17). It should also be noted that mortality is not relevant in our study in the sense that if the patient dies, he will not be re-admitted. The expressed percentage represents patients who died in our unit although, unfortunately, we are aware that many of them died outside and are, therefore, not registered as new re-admissions, and this could bias the results, but not significantly. According to the study DIOCLES which addresses the prognosis and treatment of acute coronary syndrome in Spain 18 , the ACS intra-hospital mortality rate is around 7.8%.
Something that should be noted is the high rate of re-admissions in the first month after discharge from the hospital (27.14% of the patients who were re-admitted, corresponding to 1.51% from the ACS overall). The possible clinical factors that are behind these early re-admissions should be evaluated. In accordance with other studies, in the long term, re-admission rate is significantly lower in the group where risk factors are more controlled 19 .
We can observe that control of harmful habits in the case group did not achieve an adequate progress. It strikes one that 40% of the patients admitted a fourth time still smoke. It should be pointed out that the representative values come from the first and second re-admission meaning we will focus on them to draw the conclusions. Data from the third and fourth admission is weighted with respect to the sample that is re-admitted, hence, they are not representative.
It is significant that there are so many inconsistencies between Specialized and Primary Health Care Clinic History. Though some studies state that, in effect, there are differences, they are usually related to medication 20 . However, in our study, 17.14% of the patients who stated to have harmful habits upon admission, probably motivated by fear and the serious situation, did not tell the same story to their nurses from Primary Health Care in the days previous to the coronary event. This information agrees with other studies about the lack of sincerity of some patients with their nurses 21 . It would be interesting to look into the reason behind, because it may mean that the patient does not give to his disease the importance it deserves.
Some authors mention that patients lie to the doctor all the time, unconsciously, motivated by the power relationship between doctor and patient. They feel that hiding the truth away from medical staff gives them back power and control over the situation 22 . Other studies show that age and sociocultural and economic level are related with a bad understanding of the disease 23)(24)(25 and as a consequence, they do not consider their illness as serious as it really is. But there are other studies that demonstrate that the information perceived by the medical staff is not correct or sufficient 26)(27 .
If you look at the case group and compare it with the control group, no differences are found related to age, gender or medical record. Moreover, patients from the control group present higher levels of tobacco consumption, HTA and dyslipidemia. There is a difference which can’t be considered significant regarding the days of stay in the first admission (4.93 ± 3.3 vs. 4.01± 1.8 days). The difference is, however, obvious in the risk factor management because patients from the control group (who were not re-admitted), abandoned in greater proportion tobacco consumption and reduced their cholesterol and hypertension levels more than the case group. We should emphasise that the incidence of diabetes is higher in the case group. It has been widely studied that high blood sugar levels play in favour of morbidity and mortality 28)(29)(30)(31)(32 and, in this study, it could represent a factor that makes re-admission more likely. High blood sugar levels should be studied at the moment of admission and be compared with the group control, in which there are diabetics too, but none of them had to be re-admitted.
Data indicates that a significant proportion of coronary patients do not reach the accurate therapeutic goals aimed at prevention of a new coronary event. It all seems tied around a lack of therapeutic compliance 33 . The World Health Organization 34 defined the therapeutic compliance as “the degree in which a person’s behaviour (taking the medicine, changing his/her lifestyle) is aligned with the recommendations of a healthcare provider. Based on this concept, we look for an active patient who can learn to live with his chronic illness, who is appropriately informed and who takes part in making decisions regarding his own health and disease along with the medical staff that assist him 35 . Poor compliance with the treatment and wrong heart-related health habits cause a deterioration of the disease and results in high expenses 33)(36 .
The control group presents a better compliance than the case group and this could be the reason why some people are re-admitted while others are not. There is a great variability in the prevalence of risk factors in the case group. The economic crisis might be an influencing factor, leading to patients that do not spend money to control the silent pathologies such as hypercholesterolemia and instead spending money in the ones which require painkillers considering them more important 25 . Even so, it is important to note that patients have a better control on the risk factors than on their lifestyle, even when risk factors depend, above all, on the treatment (apart from diet and physical exercise) and a change of habits depends on them and means an additional expense.
It should be contemplated the need to raise secondary prevention standards to reduce the recurring risk. In the second admission in the case group, dyslipidemia was reduced only an 11.5%, HTA 18.6% and 46% of the diabetics patients maintained measures over 140 mg/dl. This information contrasts with the one in our study, where 92.1% of the patients state that they comply with the prescribed treatment after their first admission in the coronary unit. Sugar blood levels have not been taken into account in the results because hyperglycaemia is favoured when a diabetic enters with an ACS due to his own disease, the stress and the anxiety of the situation. This information is extracted from the Primary Assistance Records in which random controls are carried out.
A deep analysis of the collected data reveals that impact in the secondary prevention and health education concerning the case group has been low. These results bring along some questions. Are the current prevention strategies failing? Why? Health education is a tool to work on risk factors and it can improve the rates of mortality, re-stroke, etc. As a consequence, early introduction within a pre-scheduled educative strategy could avoid the development of new events. This would be the ideal case, but nowadays, due to the economic context and the demand of assistance to the health system, the information received by the patient in Primary Health Care depends on the nurse’s time during the consultation, which apparently is not enough.
Another question that arises is whether patients are aware of their disease and whether they are aware about the importance of prevention and control and change of habits. As it was previously mentioned, based on the results of other studies we could state that higher levels of ignorance are associated with old people and low socio-economic level patients 23)(24)(25 . If this information is confirmed, adjusting the educative programs according to the characteristics of every patient might have positive outcome. In this aspect, research should be part of the Hospital quality programs in order to analyse and correct potential weaknesses, may they exist, in the information and communication between doctor and nurse-patient.
Nonetheless, the main idea that arises from this context is that our message, as educators, is not getting to every patient. Perhaps, re-admissions in a hospital should be considered as a quality indicator in secondary prevention.
The case group results suggest that patients with harmful habits are, at the same time, the ones who show a worse control of risk factors and they are directly related to the number of re-admissions and days of stay in hospital. Patients with this profile should be the main focus for prevention and health education. It seems that when these patients leave the hospital and return to society, they continue holding on to their harmful habits. Moreover, many studies state that patients abandon the prescribed treatment after a few months 33 .
These facts reveal that, in addition to secondary prevention, it is necessary to consider whether patients who do not control risk factors should join specific programs of cardiac rehab 37 . The World Health Organization defines Cardiac Rehabilitation programs as the set of measures aimed at the recovery and re-adaptation of the sick person who suffers or has suffered some heart disease episode in order to reach optimal levels in physic, psychological, social and labour aspects 23 . Therefore, the aim of these programs is to educate and help patients get their normal lives back, once they have acknowledged the disease, as soon as possible, or to adapt to the limitations associated with the disease. With respect to life habits, these programs are focused in tobacco use, diet and physic exercise, not just informing but also providing the necessary economic and human resources.
In Europe, cardiac rehabilitation programs are used in about 60% of the cases, in USA in 30% of the cases whereas in Spain it does not reach 5% 39 . We should consider this information together with recent research in our country that show that 65% of cardiac patients do not have enough information about their disease and prevention; 29% consider their illness less serious than it really is and 22% cannot tell if their illness is relevant in their prognosis 39 . Besides, many patients abandon the treatment a few months after discharge, and this is directly related to the number of prescribed tablets 40 .
Rehabilitation programs are relevant for the reoffending coronary patient. As health care agents, nursery can’t be considered integral assistance if it does not make the patient understand and be aware of the seriousness of the disease. It has to engage the patient in self-care, raise awareness about the seriousness of the disease and about the impact that this decision will have in the future regarding life-style changes.
Since education and health promotion provided to patients in Primary Assistance is not working as expected, one strategy that we could follow is to start the prevention during the recovery phase after an acute cardiovascular event, when patient and relatives are sensitive and motivated. This moment could be considered as the most suitable time for teaching. In Health Sciences, the perfect time is defined as the perfect context that engages the patient to improve his health 41 . Choosing the most suitable time is fundamental and it has been studied in different contexts 42)(43)(44 . Sometimes, a positive event is used to modify habits. In such case, we want to take advantage of the susceptibility that causes experiencing adverse effects caused by harmful habits to do the prevention and promotion of healthy ones towards a change in behaviour. There is evidence that being admitted in hospital gives the opportunity to adopt initiatives which trigger the change 45 . Based on public health care evidences it is recommended to do a short motivational intervention 46 . It is a short interview which tries to achieve a change regarding some behaviour in order to promote healthy habits. The short motivational intervention has demonstrated to be effective in several fields 47)(48)(49)(50)(51 and combined with the appropriate time for teaching, it should be even more effective. The seriousness and speed of ACS, favours patients who are more sensitive to quit non-healthy habits and it puts them in an ideal situation to start adopting steps for changing. The patient’s profile detected in this study, could be the suitable candidates to receive the motivational intervention upon re-admission, together with continuous care among units (ICU, ward) and continuous health education in the different levels of assistance which will have them as patients (Specialised and Primary Assistance).
The nurse’s action strategies must be aimed at:
- Adopting and maintaining healthy habits.
- Advising and helping to quit harmful habits.
- Stabilizing, slowing down and reverting the increase of the disease and the atherosclerotic processes.
- Reducing cardiovascular risk factors and morbidity and mortality, looking for a correct therapeutic compliance.
- Decreasing permanent handicap effects, and promoting an active lifestyle.
- Limiting the psychologic and physiological effects of the disease.
- Controling the symptomatology.
- Improving the life quality and the psychosocial and labour status.
- Improving the physic, psychic and social condition.
CONCLUSIONS
This study suggests that the main reason why patients are re-admitted to ICU is the lack of therapeutic compliance in secondary prevention and it is clear the need to detect a patient’s profile that is likely to suffer new coronary events. In a perfect work frame the patient should be provided with a series of assistance and teaching programs from the very first moment in which the disease is detected. Especially, in patients with harmful habits given that they are associated with uncontrolled cardiovascular factors and it is directly related to the number of re-admissions, days of stay in the hospital and medical expenses. According to this study, the candidate to be re-admitted in ICU due to ACS and which should be subject to cardiac rehab and educative intervention is a man between 55-65, every day smoker and drinker with HTA and dyslipidemia who is admitted in ICU for more than four days. The rest of the patients who do not fit in this profile, could follow the typical flow of secondary prevention.
REFERENCIAS
1. Organización Mundial de la Salud [Internet]. Copenhague (Den): Cause-specific mortality and morbidity: Age standardized mortality rate by cause by country. 2008-[citado 2013 Mar 17]. Disponible en: http://apps.who.int/gho/data/node.main.18. [ Links ]
2. Díaz-Guzmán J, Egido-Herrero JA, Fuentes B, Fernández-Pérez C, Gabriel-Sánchez R, Barberà G et al. Incidence of strokes in Spain: the Iberictus study. Data from the pilot study. Rev Neurol. 2009;48:61-5 [ Links ]
3. Villar Álvarez F, Banegas Banegas JR, de Mata Donado Campos J, Rodríguez Artalejo F. Las enfermedades cardiovasculares y sus factores de riesgo en España: hechos y cifras. Madrid: Sociedad Española de Arteriosclerosis; 2007. [ Links ]
4. Proyecto RECALCAR. La atención al paciente con cardiopatía en el Sistema Nacional de Salud. Recursos, actividad y calidad asistencial, Sociedad Española de Cardiología, Noviembre 2012. [ Links ]
5. Andrés E, Cordero A, Purificación M, Alegría E, León M, Luengo E, et al. Mortalidad a largo plazo y reingreso hospitalario tras infarto agudo de miocardio: un estudio de seguimiento de ocho años. Rev. Esp. Cardiología. 2012; 65 (5): 414-420. [ Links ]
6. García Garrido L. Epidemiología de la enfermedad coronaria. En: Portuondo Masera MªT, Martínez Castellanos T, Delgado Pacheco J, García Hernández P, Gil Alonso D, Mora Pardo JA, et al. Manual de enfermería. Prevención y rehabilitación cardíaca. Madrid: Asociación de Enfermería en Cardiología; 2009. p.39-42. [ Links ]
7. Boden WE, O'Rourke RA, Teo KK, Hatigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl Med. 2007; 356:1503-16. [ Links ]
8. Nekane Murga, A. Seguimiento del paciente en la fase crónica de la enfermedad coronaria. Rev Esp Cardiología. 2013; 13(Supl.B):35-41 - Vol. 13. [ Links ]
9. Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, BerryJD, Borden WB, et al. Heart disease and stroke statistics-2012 Update: A Report From the American Heart Association. Circulation. 2012; 125: e2 - e220. Publicación electrónica: 2011 Dic 15. http://circ.ahajournals.org/content/125/1/e2. [ Links ]
10. Maroto JM, ed. Rehabilitación cardíaca. Madrid: Sociedad Española de Cardiología, 2009. [ Links ]
11. Aberg A, Bergstrand R, Johansson S, Ulvenstam G, Vedin A, Wedel H, et al. Cessation of smoking after myocardial infarction. Effects on mortality after 10 years. Br Heart J. 1983;49:416-22. [ Links ]
12. Charles J Bentz. An intensive smoking cessation intervention reduced hospital admissions and mortality in high risk smokers with CVD. Evid. Based Med. 2007; 12; 113. [ Links ]
13. Brunner EJ, Rees K, Ward K, Burke M, Thorogood M. Dietary advice for reducing cardiovascular risk. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No.: CD002128. DOI: 10.1002/14651858.CD002128.pub3. [ Links ]
14. Hooper L, Thompson RL, Harrison RA, Summerbell CD, Ness AR, Moore HJ, et al. Risks and benefits of omega 3 fats for mortality, cardiovascular disease, and cancer: systematic review. BMJ. 2006; 332:752-60. [ Links ]
15. Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004; 116:682-92. [ Links ]
16. Salvador J, Santana L, Godenau D. Turismo, migraciones y mercado de trabajo en canarias. Rev Atlántida. 2015 [ Links ]
17. Royo-Bordonada MÁ, Lobos JM, Brotons C, Villar F, de Pablo C, Armario P, et al. El estado de la prevención cardiovascular en España. Med Clin (Barc) [Internet]. 2014 Jan 7 [ Links ]
18. Redondo-Diéguez A, Gonzalez-Ferreiro R, Abu-Assi E, Raposeiras-Roubin S, Saidhodjayeva O, López-López A, et al. Pronóstico a largo plazo de pacientes con infarto agudo de miocardio sin elevación del segmento ST y arterias coronarias sin estenosis significativa. Rev Española Cardiol [Internet]. 2015 Sep 1 [ Links ]
19. García-Molina Sáez C, Urbieta Sanz E, Madrigal de Torres M, Piñera Salmerón P, Pérez Cárceles MD. Fiabilidad de los registros electrónicos de prescripción de medicamentos de Atención Primaria. Atención Primaria [Internet]. 2016 Mar 1 [ Links ]
20. De J, Salord H. Comunicación real y aparente en la entrevista clínica?: Modelo del doble espejo. 2016;123-36. [ Links ]
21. González-Zobl G, Grau M, Muñoz MA, Martí R, Sanz H, Sala J, et al. Posición socioeconómica e infarto agudo de miocardio. Estudio caso-control de base poblacional. Rev Española Cardiol [Internet]. 2010 Sep 1 [ Links ]
22. Andrés M, García-Castrillo L, Rubini S, Juárez R, Skaf E, Fernández M, et al. Evaluación del efecto de la información en la satisfacción de los pacientes atendidos en los servicios de urgencias hospitalarios. Rev Calid Asist [Internet]. 2007 Jul 1 [ Links ]
23. Sanjuán R, Núñez J, Blasco ML, Miñana G, Martínez-Maicas H, Carbonell N, et al. Implicaciones pronósticas de la hiperglucemia de estrés en el infarto agudo de miocardio con elevación del ST. Estudio observacional prospectivo. Rev Española Cardiol [Internet]. 2011 Mar 1 [ Links ]
24. Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev [Internet]. 2014 Nov 20 [ Links ]
25. Fernández-de-Bobadilla J, López-de-Sá E. Carga económica y social de la enfermedad coronaria. Rev Española Cardiol Supl [Internet]. 2013 Jan 1 [ Links ]
26. Rehabilitation of patient with cardiovascular disease WHO. Technical Reports Ginebra: OMS, 1964; n. º 270. [ Links ]
27. Manuel Barreiroa,, Elena Velascoa, Alfredo Renillaa, Francisco Torresa, María Martín, De la Hera JM. Grado de conocimiento sobre su enfermedad cardiaca entre los pacientes hospitalizados..Rev Esp Cardiología. 2013; 66:229-30. - Vol. 66 Núm.3. [ Links ]
28. Meseguer C, Galan I, Herruzo R, Zorrilla B, Rodriguez-Artalejo F. Actividad física de tiempo libre en un país mediterráneo del sur de Europa: Adherencia a las recomendaciones y factores asociados. Rev Esp Cardiol. 2009; [ Links ]
29. Lawson PJ, Flocke SA. Teachable moments for health behavior change: a concept analysis. Patient Educ Couns [Internet]. 2009 Jul 1 [ Links ]
30. Lakerveld J, Bot SD, Chinapaw MJ, van Tulder MW, Kostense PJ, Dekker JM, et al. Motivational interviewing and problem solving treatment to reduce type 2 diabetes and cardiovascular disease risk in real life: a randomized controlled trial. Int J Behav Nutr Phys Act [Internet]. 2013 Apr 19 [ Links ]
31. Gil Extremera B, Maldonado Martín A, Soto Más JA, Gómez Jiménez FJ. Hiperglucemia postprandial como factor de riesgo cardiovascular. Rev Clínica Española [Internet]. 2002 Jan 1 [cited 2018 Mar 12];202(7):399-402. Available from: https://www.sciencedirect.com/science/article/pii/S0014256502710904 [ Links ]
32. López-Maldonado FJ, Reza-Albarrán AA, Suárez ÓJ, Villa AR, Ríos-Vaca A, Gómez-Pérez FJ, et al. Grado de control de factores de riesgo cardiovascular en una población de pacientes con diabetes mellitus tipo 1 y 2 de difícil manejo. Gac Méd Méx [Internet]. 2009 [cited 2018 Mar 12];145(1). Available from: https://www.anmm.org.mx/GMM/2009/n1/vol_145_n1.pdf [ Links ]
33. Munger MA, Van Tassell BW, LaFleur J. Medication nonadherence: an unrecognized cardiovascular risk factor. MedGenMed [Internet]. 2007 Sep 19 [cited 2018 Mar 11];9(3):58. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18092064 [ Links ]
34. OMS | El incumplimiento del tratamiento prescrito para las enfermedades crónicas es un problema mundial de gran envergadura. WHO [Internet]. 2013 [cited 2018 Mar 12]; Available from: http://www.who.int/mediacentre/news/releases/2003/pr54/es/ [ Links ]
35. Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev [Internet]. 2014 Nov 20 [cited 2018 Mar 11]; Available from: http://doi.wiley.com/10.1002/14651858.CD000011.pub4 [ Links ]
36. Fernández-de-Bobadilla J, López-de-Sá E. Carga económica y social de la enfermedad coronaria. Rev Española Cardiol Supl [Internet]. 2013 Jan 1 [cited 2018 Mar 11];13:42-7. Available from: https://www.sciencedirect.com/science/article/pii/S1131358713700797 [ Links ]
37. Mora Pardo JA. Programas de prevención y rehabilitación cardiaca. En: Portuondo Masera MªT, Martínez Castellanos T, Delgado Pacheco J, García Hernández P, Gil Alonso D, Mora Pardo JA, et al. Manual de enfermería. Prevención y rehabilitación cardíaca. Madrid: Asociación de Enfermería en Cardiología; 2009. p. 123-188. [ Links ]
38. Rehabilitation of patient with cardiovascular disease WHO. Technical Reports Ginebra: OMS, 1964; n. º 270. [ Links ]
39. Manuel Barreiroa,, Elena Velascoa, Alfredo Renillaa, Francisco Torresa, María Martín, De la Hera JM. Grado de conocimiento sobre su enfermedad cardiaca entre los pacientes hospitalizados..Rev Esp Cardiología. 2013; 66:229-30. - Vol. 66 Núm.3. [ Links ]
40. Meseguer C, Galan I, Herruzo R, Zorrilla B, Rodriguez-Artalejo F. Actividad física de tiempo libre en un país mediterráneo del sur de Europa: Adherencia a las recomendaciones y factores asociados. Rev Esp Cardiol. 2009; [ Links ]
41. Lawson PJ, Flocke SA. Teachable moments for health behavior change: a concept analysis. Patient Educ Couns [Internet]. 2009 Jul 1 [cited 2018 Mar 13];76(1):25-30. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19110395 [ Links ]
42. Clark BJ, Moss M. Secondary prevention in the intensive care unit: does intensive care unit admission represent a »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ teachable moment? »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ . Crit Care Med [Internet]. 2011 Jun [cited 2018 Mar 13];39(6):1500-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21494113 [ Links ]
43. Phelan S. Pregnancy: a "teachable moment" for weight control and obesity prevention. Am J Obstet Gynecol [Internet]. 2010 Feb 1 [cited 2018 Mar 13];202(2):135.e1-135.e8. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0002937809006280 [ Links ]
44. DiFranza JR, Lew RA, Palfrey JS, Perrin JM, Rigotti NA. Morbidity and mortality in children associated with the use of tobacco products by other people. Pediatrics [Internet]. 1996 Apr 1 [cited 2018 Mar 13];97(4):560-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8632946 [ Links ]
45. Glasgow RE, Stevens VJ, Vogt TM, Mullooly JP, Lichtenstein E. Changes in Smoking Associated with Hospitalization: Quit Rates, Predictive Variables, and Intervention Implications. Am J Heal Promot [Internet]. 1991 Sep 25 [cited 2018 Mar 13];6(1):24-9. Available from: http://journals.sagepub.com/doi/10.4278/0890-1171-6.1.24 [ Links ]
46. Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT). Subst Abus [Internet]. 2007 Nov 21 [cited 2018 Mar 13];28(3):7-30. Available from: http://www.tandfonline.com/doi/abs/10.1300/J465v28n03_03 [ Links ]
47. Smedslund G, Berg RC, Hammerstrøm KT, Steiro A, Leiknes KA, Dahl HM, et al. Motivational interviewing for substance abuse. Cochrane Database Syst Rev [Internet]. 2011 May 11 [cited 2018 Mar 13]; Available from: http://doi.wiley.com/10.1002/14651858.CD008063.pub2 [ Links ]
48. Wong EM, Cheng MM. Effects of motivational interviewing to promote weight loss in obese children. J Clin Nurs [Internet]. 2013 Sep 1 [cited 2018 Mar 13];22(17-18):2519-30. Available from: http://doi.wiley.com/10.1111/jocn.12098 [ Links ]
49. Smedslund G, Berg RC, Hammerstrøm KT, Steiro A, Leiknes KA, Dahl HM, et al. Motivational interviewing for substance abuse. In: Smedslund G, editor. Cochrane Database of Systematic Reviews [Internet]. Chichester, UK: John Wiley & Sons, Ltd; 2009 [cited 2018 Mar 13]. Available from: http://doi.wiley.com/10.1002/14651858.CD008063 [ Links ]
50. Cochrane Database of Systematic Reviews [Internet]. Chichester, UK: John Wiley & Sons, Ltd; 1996 [cited 2018 Mar 13]. Available from: http://doi.wiley.com/10.1002/14651858 [ Links ]
51. Lakerveld J, Bot SD, Chinapaw MJ, van Tulder MW, Kostense PJ, Dekker JM, et al. Motivational interviewing and problem solving treatment to reduce type 2 diabetes and cardiovascular disease risk in real life: a randomized controlled trial. Int J Behav Nutr Phys Act [Internet]. 2013 Apr 19 [cited 2018 Mar 13];10(1):47. Available from: http://ijbnpa.biomedcentral.com/articles/10.1186/1479-5868-10-47 [ Links ]
Received: November 21, 2017; Accepted: March 18, 2018











 texto en
texto en