Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.18 no.56 Murcia oct. 2019 Epub 23-Dic-2019
https://dx.doi.org/10.6018/eglobal.18.4.352261
Originals
Patient safety culture: evaluation of nurses in primary health care
1Nurse. Master's student at the Postgraduate Program in Nursing at UFPR (Federal University of Paramá). On scholarship provided by the Coordination of Higher Education Personnel Development from 2017 to 2019. Curitiba City, Paraná State (PR), Brazil.
2Nurse. Master's student of the Postgraduate Program in Nursing at UFPR (Federal University of Paramá). Curitiba-PR, Brasil.
3Nurse. Nursing Teacher at the UFPR (Federal University of Paramá). Curitiba City, Paraná State (PR), Brazil.
4Nurse. Master in Nursing by UFPR (Federal University of Paramá). Curitiba City, Paraná State (PR), Brazil.
Introduction
Studies on patient safety in Primary Health Care (PHC) are up to date; however, there are no details on professionals' actual performance in relation to this matter. Thus, it is important to evaluate the safety culture characterization among nursing professionals in this scenario, since it will promote better care for users.
Objective
To evaluate the patient safety culture from the perspective of nurses in Primary Health Care.
Method
Descriptive study of quantitative approach carried out in fourteen health Units in Curitiba City, Paraná State (PR), Brazil from July to December 2017. There were forty-three nurses participating in this study. Medical Office Survey on Patient Safety Culture (MOSPSC) was the tool used, comprising fifty-one questions that evaluate twelve dimensions of patient safety. This tool, Portuguese version, showed a Cronbach alpha coefficient of 0.95, which expresses high reliability. All data were analyzed by Descriptive Statistics using Likert scale.
Results
Inconsistencies were found related to the information exchange with other institutions, work process, fear of guilt, punishment for errors, and management. In the overall evaluation, 50% of the Family Health Strategy (FHS) professionals rated patient safety “very good”, and 73.9% of Basic Health Units (BHU) professionals rated patient safety “good”.
Conclusion
Results show a safety culture with potentialities and weaknesses that need to be developed, considering the nurse the cornerstone to the success of quality and safety enhancement of patient in Primary Health Care.
Keywords: Patient safety; Primary health care; Nursing
INTRODUCTION
Discussions on patient safety have been of fundamental importance to improve the quality in health organizations on the world scene.1 The World Health Organization (WHO)2 defined patient safety as the risk reduction of unnecessary damage related to health care to an accepTable minimum considered a health care quality dimension. However in this logic, it is known that zero error is unlikely in health care.3,4
Currently, patient safety research is focused on the hospital context, and studies show scarcity of scientific literature on Primary Health Care (PHC).5 PHC is considered the main entry point to the Sistema Único de Saúde (Unified Health System) (SUS, Brazilian acronym), the health care level most used by the population, and the communication center among Health Care Networks (HCN) in Brazil.6,7 In Curitiba City, there are two models of Health Units in PHC, Family Health Strategy Units (FHS) and Basic Health Units (BHU).6
Adverse events are also common in PHC, but the principle of not causing harm must be strictly linked to the PHC role; for that, it is needed to extend the discussion about safe care, looking for implementing it in health organizations as a cultural process, promoting the participation by professionals and stimulating debate and discussion on the theme, helping to implement strategies aimed at improving the safety and health care culture.5,8 In this sense, the nurse plays a key role in the development of actions that promote patient safety in the PHC, as an interlocutor between the health system and the user, leading to generate changes in the workplace and strength the patient safety culture.9,10
For the achievement of safe care, the safety culture is understood as a multifactorial structure that promotes the system actions to prevent and reduce harm so that health professionals and organizations can share practices, values, attitudes, and behavior for harm reduction and promote safe health care.8
In this way, it is important to evaluate the safety culture characterization among the PHC professionals, making it possible to analyze the organizational conditions that cause possible adverse events to service users, as well as, to diagnose the safety culture level, internal and external benchmarking, use effective strategies aimed at patient safety and interventions in safety culture evolution in the medium and long term.11
Taking into account the need to discuss the recommendations for the improvement of patient safety culture in PHC presented by the nurses, and the lack of Brazilian national literature on the theme, this study aims to evaluate the patient safety culture under nurses’ perspective in PHC.
METHODOLOGY
It is a descriptive research of quantitative approach, carried out in fourteen Health Units belonging to a Sanitary District of Curitiba City, Paraná State (PR), Brazil, composed of seven Basic Health Units (BHU) and seven Family Health Strategy (FHS). A sanitary district was chosen for carryind out this study among ten sanitary subdivisions in the municipality, managed separately subject to variations in the organizational culture. This study is part of the research project titled “Avaliação e Planejamento da Segurança do Paciente e da Qualidade em Saúde: em busca de ações estratégicas para a melhoria do cuidado” ("Evaluation and Planning of Patient Safety and Health Quality: in search of strategic actions for care improvement").
The ethical aspects described in the Resolution No. 466/2012 of the National Health Council (CNS, Brazilian acronym) and in the Circular Letter No. 51-SEI/2017 were support for this study. This study was approved by the Research Ethics Committee of Health and Science Department at the Federal University of Paraná and the Municipal Health Department of Curitiba, under the terms of Opinion No. 2,043,970 and Certificado de Apresentação para Apreciação Ética (CAAE) (Presentation Certificate for Ethical Appreciation) No. 66939717.3.0000.0102
The PHC professional population in this Sanitary District was composed of fifty-two nurses. Professionals who worked longer than six months at this study site were included and those who were away from their activities, for vacation or health/maternity leave, in the time of data collection were not included. The sample loss consisted of two FHS professionals who refused to participate in this study, a nurse from BHU who did not deliver the instrument completed at the time of data collection, and six nurses who were on vacation or maternity leave. This study final sample was composed of forty-three participants, of which twenty nurses belonging to FHS units and twenty-three from the BHUs, from July to December 2017.
Regarding the Units characteristics, the FHS objective is to reorganize the PHC in the country under the Sistema Único de Saúde (SUS, Brazilian acronym) (Health Unic System) regulatory standards. The teams are responsible for monitoring a certain number of families, boosting actions to promote, prevent, recover, and rehabilitate health, diseases, and other injuries. The nursing professional working hours is forty hours a week in FHS. Basic Health Units (BHU) is the type of unit that must meet the principles and guidelines proposed for basic care. The municipal administration can form the teams according to the municipality characteristics and needs. Its goal is to ensure access, connection among people, professionals, community, coordination, and care longitudinality. The nursing working hours is thirty hours a week in BHU.6
The data collection approach started via telephone call to the immediate manager of each Unit and the research and its objectives were explained. Subsequently, a day was scheduled for the researcher to go to the study site and meet the participants in their work environment, make a formal invitation and present the research objectives along with the Free and Informed Consent Term (FICT). The evaluation tool and the FICT were delivered to the professionals who agreed to participate. Participants had the option to answer the evaluation tool in working hours or deliver it on another date.
The Medical Office Survey on Patient Safety Culture (MOSPSC) was the tool used.12 This tool is composed of fifty-one questions that assess twelve patient safety dimensions and, in the Brazilian context, it was translated, adapted, and validated.8 The tool Portuguese version showed a Cronbach alpha coefficient of 0.95, which expresses high reliability.8
Data from the MOSPSC completion were entered in Excel® spreadsheet, double typed, and analyzed using Descriptive Statistics. The gradual progression of data comprehension was carried out using the Likert scale according to the denominations of sections and the respective Units model (FHS/BHU). Items of C, D, E, and F sections had score inversion to follow the sequential logic of positive, neutral, and negative points of the other items in the tool. The inverted questions were: (c3), (c6), (c8), (c10), (c12), (c14), (d4), (d7), (d10), (e1), (e2), (e4), (f3), (f4), and (f6). They were labeled "inv".
RESULTS
Forty-three nurses participated in the study, 74.4% (n=32) occupied a care position and 25.6% (n=11) occupied a management position (called a “local health authority”), aged from 30 to more than 50 years old.
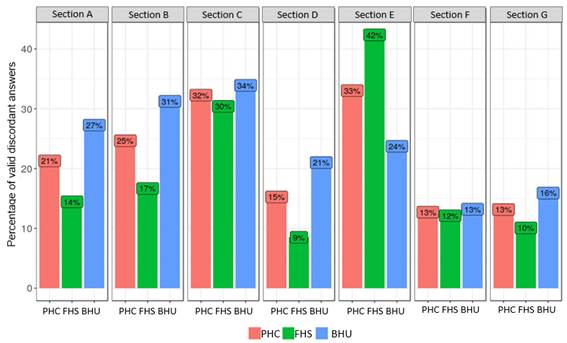
Due to the tool extension, it was decided to present the results, the description of the most important data that showed low scores of each section in each Unit and the percentage of valid discordant answers of each section (Figure 1). It can be noticed that in the FHS there was predominance of disagreement in section E; in BHU, there was predominance of disagreement in section C. This fact shows high concern for PHC patient safety.
Section A provides description of events that may interfere in the user safety and the care quality. Concerning question (a1) about FHS care ("A patient could not get appointment within 48 hours for a serious/chronic health issue"), the following answers were obtained: (a) "at least once a week" [20% (n=4)]; (b) "at least once a month" [10% (n=2)]; and (c) "daily" [5% (n=1)]. In BHU, 21.5% of participants (n=5) reported the possible event of "at least once a week".
Section B referred to issues related to the information exchange with other health institutions. The questions (b3) ("pharmacies") and (b4) ("hospitals") showed events of daily issues regarding the information exchange with other institutions in the FHS. In BHU, there were many choices in the item, "It does not apply or I do not know"; however, issues related to image centers/laboratories got a lot of attention, in which 26.1% (n=6) chose "Several issues in the last 12 months” and 13% (n=3) chose "Daily issues" related to the hospitals. Specifying the “Issues at least once a month" in the Social Action Foundation (SAF), one participant (4.4%) pointed the "Others" item.
Section C relates to the work process. Regarding the question (c3.inv) ("In this service we often feel rushed when attending the patient") in the FHS, 50% (n=10) of professionals reported yes, they feel rushed. In BHU, 43.5% (n=10) of the professionals also reported that they feel rushed in this issue. However, 39.1% (n=9) were in a neutral position, pointing "I do not agree or disagree".
Section D refers to communication and medical monitoring. In the FHS, for the question (d7.inv) ("The staff of this service believe that their mistakes can be used against themselves"), 45% (n=9) of professionals answered yes. In BHU, this item showed the worst evaluation with 52.2% (n=12) of the participants answering also that the errors can be used against themselves.
Section E relates to the managers/administrators/leaders and the respondents were only the non-manager nurses. In the FHS, the high rate of professional dissatisfaction in this section was analyzed, since the most answers were "totally disagree" and "disagree". In (e.4 inv) item ("They often make decisions based on what is best for the service rather than what is best for the patients"), 43.7% (n=7) of the participants reported negative connotations, because they agree that most decisions are based on improving the service in detriment of the user. For this same issue in BHU, 26.7% (n=4) agreed with this statement, but 33.3% (n=5) kept "neutral".
Section F refers to the workplace of the health professional. Regarding the question (f.6 inv) ("In this service, the number of activities performed is more important than the care quality provided") in the FHS, there was the worse evaluation, since 30% (n=6) of the nurses agreed with the statement. In the (f4.inv) item (“Is only by chance that we do not make more mistakes that affect our patients”) in BHU, 17.4% (n=4) of the participants believe that it is true. In the question (f6.inv), only 39.4% (n=7) of participants agree with the question.
Finally, section G was divided into two categories, G.1, overall quality evaluation, and G.2, general patient safety evaluation. The FHS presented three questions that showed negative answers. One of them was (g1c) ("Especifically: It minimizes waiting times and delays, potentially harmful") with 20% (n=4) considering this statement "reasonable". In G.2 category, 50% (n=10) of the nurses marked "Very good" the patient's safety in primary care, and only 10% (n=2) considered "reasonable".
In UBS, two categories attracted attention due to the high rate of negativism. For the (g1c) question ("Especifically: It minimizes waiting times and delays, potentially harmful"), 30.4% (n=7) of participants answered "reasonable", and to (g1d) question ("Efficient: Ensures good effective-cost care (avoiding wastage, overuse and misuse of services)”), 21.7% (n=5) of the participants also considered it "reasonable". In the (G.2) category, 73,9% (n=17) of the professionals evaluated the patient safety in the PHC "Good" and 26,1% (n=6), evaluated "Very good". It was also found that no professional considered this category with negative aspects.
DISCUSSION
The results obtained with the application of the questionnaire allowed the evaluation of the safety culture by the nurses from the Sanitary District, as well as, identification of strengths and weaknesses points.
It is understood that PHC is the entry point to the health system and the difficulty of access shows that the user looking for the services not necessarily has this access guaranteed. The obstacles for scheduling appointments, medical care, and the delay in some health check puts into question the PHC role of ordinance that end up serving as alibi for the attempts to displace it as a entry point to SUS.13
The inconsistences in the information exchange were evident and daily in the PHC context. Efficient communication avoids errors; however, the existence of barriers that make it difficult results in important meanings for both professionals and users. Studies have shown that ineffective communication among health professionals has been one of the contributing factors for adverse events, accounting for more than 70% of the root causes of errors in health care.14,15
This can be noticed not only in the workplace, but also at other health institutions, especially in PHC, since it needs to share information with hospitals, laboratories, healthy special centers, and other departaments and institutions. This item is considered of prime importance for PHC care, since communication with other health services is deficient.16 In this way, it is recommended to improve and articulate the communication among the main areas involved for developing and promoting positive actions for patient safety (communication skills training programs, practical simulations, and standardized ways to present information to users), minimizing risks and ensuring safe and quality care.15,17
Regarding the work process, Brazilian health institutions have been facing a lack of health planning and, as showed in this study, professionals feel rushed to provide care to the user often due to the high service demand, which, added to workload, can compromise user safety in PHC. However, the Ministry of Health, the National Sanitary Surveillance Agency, and other ministerial bodies in Brazil have implemented policies to improve care resulting in a consequent increase in patient safety in Brazilian institutions.
A Brazilian study shows that factors such as service management, human resources deficit, work overload, interpersonal relationship, communication breakdown, and low continuity of care provided to users have compromised the health care in institutions.18
Although expressing their opinions, the professionals of the FHS and BHU believe that their errors can be used against themselves, showing weakness in this dimension and confirming another study carried out in the PHC context.19 Tying mistake to guilty is still a common practice in a punitive work environment, as well as concluding that mistakes are caused by the health care professionals due to their carelessness or inattention. When professionals do not express their opinions or do not report an alleged error, the issues will remain or even worsen, so the safety culture must be aligned with the discussions and priorities of the institutions, excluding the punitive culture.20,15
It is also critical to encourage teams that mistakes and guilty events can be chances to turn them into opportunities to discuss, improve care, critically reflect about, and prevent recurring events with the same cause.19
In the management-related dimension, the FHS participants showed dissatisfaction with their managers, administrators, and leaders, countering the BHU professionals who remained neutral. Widely, managers' commitment to patient safety is an essential element for the strengthening of a safety culture, since management is an important tool of institutional policy, incorporating an articulator and interactive character.21 Managers or administrators are recognized as a subculture of the safety culture with responsibility of the commitment for the service to the user, as well as, designing the pertinent elements for the construction of patient safety, including existing gaps, which involve reduction in the patient care quality.22
The nurses agreed that their work process is effective for error prevention, which can be aligned to establishment of a good relationship among the professional team. The identification of risks in user safety is considered a strategy for the development of safety culture23 in PHC. However, with respect to negative connotation answers, nurses reported that the amount of activities performed is more important than the quality. It is known that this aspect results negatively for patient safety, especially in the FHS context, since this program is focused on family care.
At the end of this analysis, the tool used provides the overall evaluation of these health services. Regarding the general evaluation and the quality, the nurses of the FHS and BHU consider their workplaces "very good" or "good". This professional perception is important for direct risk evaluation because it contributes to care apropriate management, focusing on the error prevention and on the safety culture implementation in PHC.21
These research contributions may serve as a foundation for managers to analyze the relevance of understanding the patient safety culture in PHC. One study showed that many adverse events found in the hospital come from PHC and, often, go unnoticed by health professionals. It is understood that this theme is more focused on the hospital environment, considering that care is more complex.7
Studying patient safety culture in PHC is fundamental for advancing knowledge about the risks, magnitude, and nature of adverse events caused by unsafe practices. Considering these aspects, specific protocols can be developed for safe care in PHC.
CONCLUSION
The evaluation of safety culture in PHC is multifactorial and goes beyond elements related to the structure, process, and results of health work. In the scenario studied, the punitive culture focuses on the errors, by the fear that professionals must report them.
It is emphasized the need to strengthen patient safety discussions in PHC to promote the professionals' awareness about their ethical commitment and effective communication, aiming to strengthening non-punitive culture. The negative evaluation assigned by FHS professionals to managers is a challenge to PHC.
The participation of only nurses and not multiprofessional team is a limitation for this study, which did not allow evaluating globally the safety culture. However, the importance of nursing engagement for safe and quality practices is known, and the nurse is the basis of this process and fundamental for the skills improvement knowledge, and strategy developments that promote patient safety.
It is understood that the safety culture in PHC is a complex phenomenon, which needs to be identified to provide better actions and to create tools to assist and promote safe care. The user of these services must also be introduced in this battle, since they are also responsible for their safety, helping to identify and prevent adverse events and promoting safety.
REFERENCIAS
1. Poghosyan L, Nannini A, Clarke S. Organizational climate in primary care settings: Implications for nurse practitioner practice. J Am Assoc Nurse Pract [Internet]. 2013 [acceso en 2018 oct. 17]; 25(3):134-140. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/24218200 [ Links ]
2. World Health Organization (WHO) [Internet]. Geneva: World Health Organization; 2009 [acceso en 2018 oct 22]. Human Factors in Patient Safety Review of Topics and Tools. Disponible en: https://www.who.int/patientsafety/research/methods_measures/human_factors/human_factors_review.pdf [ Links ]
3. WORLD HEALTH ORGANIZATION (WHO) [Internet]. Geneva: World Health Organization; 2017 [acceso en 2018 sept 29]. Patient Safety. Disponible en: http://www.who.int/patientsafety/safer_primary_care/en/ [ Links ]
4. Cruz EDA, Rocha DJM, Mauricio AB, Ulbrich FS, Batista J, Maziero ECS. Safety culture among health professionals in a teaching hospital. Cogitare Enferm [Internet]. 2018 [acceso en 2018 sept 29]; 23(1):e50717. Disponible en: http://docs.bvsalud.org/biblioref/2018/02/879967/50717-222541-1-pb.pdf [ Links ]
5. Mesquita KO, Silva LCC, Lira RCM, Freitas CASL, Lira GV. Segurança do paciente na atenção primária à saúde: revisão integrativa. Cogitare Enferm [Internet]. 2016 [acceso en 2018 oct 12]; 21(2):1-8. Disponible en: https://revistas.ufpr.br/cogitare/article/view/45665 [ Links ]
6. Brasil. Ministério da Saúde. Portaria GM n. 2.436, de 21 de setembro de 2017. Aprova a Política Nacional de Atenção Básica, estabelecendo a revisão de diretrizes para a organização da Atenção Básica, no âmbito do Sistema Único de Saúde (SUS) [Internet]. Brasília (DF); 2017. [acceso en 2018 oct 12]. Disponible en: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2017/prt2436_22_09_2017.html [ Links ]
7. Marchon SG, Mendes Junior WV, Pavão ALB. Características dos eventos adversos na atenção primária à saúde no Brasil. Cad Saúde Pública [Internet]. 2015 [acceso en 2018 oct 14]; 31(11):2313-2330. Disponible en: http://www.scielo.br/pdf/csp/v31n11/0102-311X-csp-31-11-2313.pdf [ Links ]
8. Timm M, Rodrigues MSC. Adaptação transcultural de instrumento de cultura de segurança na Atenção Primária. Acta Paul Enferm [Internet]. 2016 [acceso en 2018 oct 22]; 29(1):26-37. Disponible en: http://www.scielo.br/pdf/ape/v29n1/1982-0194-ape-29-01-0026.pdf [ Links ]
9. Macedo TR, Rocha PK, Tomazoni A, Souza S, Anders JC, Davis K. Cultura de segurança do paciente na perspectiva da equipe de enfermagem de emergências pediátricas. Rev Esc Enferm USP [Internet]. 2016 [acceso en 2018 oct 20]; 50(5):757-763. Disponible en: http://www.scielo.br/pdf/reeusp/v50n5/pt_0080-6234-reeusp-50-05-0757.pdf [ Links ]
10. Martiello RDC, Lima EFA, Coelho MCR, Oliveira ERA, Leite FMC, Primo CC. A cultura de segurança do paciente na perspectiva do enfermeiro. Cogitare Enferm [Internet]. 2016 [acceso en 2018 agosto 22]; 21 (esp):1-9. Disponible en: https://revistas.ufpr.br/cogitare/article/view/45408 [ Links ]
11. Andrade LEL, Lopes JM, Souza Filho MCM, Vieira Júnior RF, Farias LPC, Santos CCMS et al. Cultura de segurança do paciente em três hospitais brasileiros com diferentes tipos de gestão. Ciência & Saúde Coletiva [Internet]. 2018 [acceso en 2018 agosto 21]; 23(1):161-172. Disponible en: https://www.scielosp.org/article/ssm/content/raw/?resource_ssm_path=/media/assets/csc/v23n1/1413-8123-csc-23-01-0161.pdf [ Links ]
12. Agency for Healthcare Research and Quality (AHRQ) [Internet]. Rockville, MD: AHRQ; c2007 [acceso en 2018 agosto 22]. Surveys on Patient Safety Culture. Disponible en: https://www.ahrq.gov/sops/quality-patient-safety/patientsafetyculture/hospital/index.html [ Links ]
13. Campos RTO, Ferrer AL, Gama CAP, Campos GWS, Trapé TL, Dantas DV. Avaliação da qualidade do acesso na atenção primária de uma grande cidade brasielira na perspectiva dos usuários. Saúde Debate [Internet]. 2014 [acceso en 2018 agosto 22]; 38 (esp): 252-264. Disponible en: http://www.scielo.br/pdf/sdeb/v38nspe/0103-1104-sdeb-38-spe-0252.pdf [ Links ]
14. Rede Brasileira de Enfermagem e Segurança do Paciente (REBRAENSP). Estratégias para a segurança do paciente: manual para profissionais da saúde [internet]. Porto Alegre (RS): EDIPUCRS; 2013. [acceso en 2018 agosto 22]. Disponible en: http://biblioteca.cofen.gov.br/wp-content/uploads/2017/10/Estrat%C3%A9gias-para-seguran%C3%A7a-do-paciente-manual-para-profissionais-da-sa%C3%BAde.pdf [ Links ]
15. Nogueira JWS, Rodrigues MCS. Comunicação efetiva no trabalho em equipe em saúde: desafio para a segurança do paciente. Cogitare Enferm [Internet]. 2015 [acceso en 2018 agosto 22]; 20(3):636-640. Disponible en: https://revistas.ufpr.br/cogitare/article/view/40016 [ Links ]
16. Massoco ECP, Melleiro, MM. Comunicação e segurança do paciente: percepções dos profissionais de enfermagem de um hospital de ensino. Rev Min Enferm [Internet]. 2015 [acceso en 2018 sept 18]; 19(2):192-195. Disponible en: http://www.reme.org.br/artigo/detalhes/1014 [ Links ]
17. Gonçalves MI, Rocha PK, Anders JC, Kusahara DM, Tomazoni A. Comunicação e segurança do paciente na passagem de plantão em unidades de cuidados intensivos neonatais. Texto Contexto Enferm [Internet]. 2016 [acceso en 2018 sept 18]; 25(1):e2310014. Disponible en: http://www.scielo.br/pdf/tce/v25n1/0104-0707-tce-25-01-2310014.pdf [ Links ]
18. Capucho HC, Cassiani SHB. Necessidade de implantar Programa de segurança do paciente no Brasil. Rev Saúde Pública [Internet]. 2013 [acceso en 2018 oct 23]; 47(4):791-798. Disponible en: http://www.scielo.br/pdf/rsp/v47n4/0034-8910-rsp-47-04-0791.pdf [ Links ]
19. Paese F, Dal Sasso GTM. Patient safety culture in primary health care. Text Context Enferm [Internet]. 2013 [cited 2018 oct 16]; 22(2):302-310. Disponible en http://www.scielo.br/pdf/tce/v22n2/en_v22n2a05.pdf [ Links ]
20. Calori MAO, Gutierrez SL, Guidi TAC. Segurança do paciente: Promovendo a cultura de segurança. Saúde em Foco. [Internet] 2015 [acceso en 2018 sept 18]; (7):226-235. Disponible en: http://unifia.edu.br/revista_eletronica/revistas/saude_foco/artigos/ano2015/seguranca_paciente.pdf [ Links ]
21. Lemos GC, Azevedo C, Bernardes MFVG, Ribeiro HCTC, Menezes AC, Mata LRF. A Cultura de Segurança do Paciente no Âmbito da Enfermagem: Reflexão Teórica. Revista de Enfermagem do Centro-Oeste Mineiro [Internet]. 2018 [acceso en 2018 sept 2]; 8: e2600. Disponible en: http://www.seer.ufsj.edu.br/index.php/recom/article/view/2600/1880 [ Links ]
22. Cauduro FLF, Sarquis LM, Sarquis LMM, Curz, EDA. Cultura de segurança entre profissionais de centro cirúrgico. Cogitare Enferm. [Internet]. 2015 [acceso en 2018 sept 18]; 20(1): 129-38. Disponible en: https://revistas.ufpr.br/cogitare/article/view/36645/24859 [ Links ]
23. Oliveira RM, Leitão IMTA, Silva LMS, Figueiredo SV, Sampaio RL, Gondim MM. Estratégias para promover segurança do paciente: da identificação dos riscos às práticas baseadas em evidência. Esc Anna Nery [Internet]. 2014 [acceso en 2018 sept 2]; 18(1):122-129. Disponible en: http://www.scielo.br/pdf/ean/v18n1/1414-8145-ean-18-01-0122.pdf [ Links ]
Received: December 03, 2018; Accepted: February 06, 2019











 texto en
texto en