Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.20 no.64 Murcia oct. 2021 Epub 25-Oct-2021
https://dx.doi.org/10.6018/eglobal.471511
Originals
Association between sociodemographic characteristics, depressive symptoms, stress and anxiety in times of COVID-19
1 Universidad Autónoma de Coahuila. Facultad de Enfermería “Dr. Santiago Valdés Galindo” Saltillo Coahuila, México. dafne.gomez@uadec.edu.mx
Introduction:
The COVID-19 pandemic has affected the mental health of the population. Depressive symptoms, stress, and anxiety are negative responses that can occur in risky situations in which uncertainty, the unknown or crisis situations are faced, such as the current health crisis.
Objective:
To identify the association between sociodemographic factors and depressive symptoms, level of stress and anxiety in times of COVID-19 in inhabitants of the city of Saltillo Coahuila, Mexico.
Methods:
Cross-sectional predictive correlational study. The population was inhabitants of the city of Saltillo Coahuila, Mexico. The sample consisted of 501 participants, who were collected through an online survey that was made available from October 5 to 24, 2020.
Results:
Age (OR = .93; 95% CI: .900 - .979) and being without a partner (OR = 2.64; 95% CI: 1.347 - 5.201) increase the probability of suffering severe depressive symptoms. Younger people were .95 more likely to have elevated stress. Being a woman (OR = 2.37; 95% CI: 1,144 - 4,915) and not having a job (OR = 2.62; 95% CI: 1,308 - 5,254) was associated with a higher probability of suffering from severe anxiety.
Conclusion:
Associations were found in sociodemographic factors such as sex, age and economic income with depressive symptoms, level of stress and anxiety in times of COVID-19. These results project preliminary data on some aspects related to mental health in the Mexican context during the current health crisis.
Key words: Coronavirus Infections; Depression; Psychological Stress; Anxiety; Mental Health
INTRODUCTION
A new coronavirus disease dubbed COVID-19 by the World Health Organization has become a health emergency 1. This virus was identified in December 2019 in Wuhan, Hubei province, China. COVID-19 strains have been linked to Severe Acute Respiratory Syndrome coronavirus (SARS-CoV) and Middle East Respiratory Syndrome coronavirus (MERS-CoV) 2, characteristics for which it has been considered highly dangerous for human beings.
Worldwide, more than 99.3 million infections have been reported and more than 2.1 million deaths have been caused by COVID-19 3. In Mexico, more than 1.9 million confirmed cases have been identified; 425,044 suspected cases and 168,858 deaths. Of the confirmed cases, 49.50% are women and 50.50% are men, 13.70% are hospitalized and 86.30% are outpatients. The main associated comorbidities are hypertension (13.70%), obesity (12.30%), diabetes (10.40%) and smoking (6.60%) 4.
Due to the high incidence of cases, their rapid spread and severity, COVID-19 was termed a pandemic on March 11, 2020 5. Since this communiqué, governments around the world, including Mexico, have implemented various strategies to contain COVID-19, such as quarantine, isolation or social distancing, among others. These measures affect individual or collective behavior patterns, in addition to having biopsychosocial repercussions and affecting the mental health of the population 6,7,8.
The distance between people and the absence of interpersonal communication, the lack of vaccines and effective treatments, the lack of knowledge about the duration of isolation and the high economic, social and health impact generate uncertainty in the population, and increase the risk of suffering from depressive disorders, stress and anxiety 9,10,11. Likewise, an increase in negative emotions (anxiety, depression and indignation) and a decrease in positive emotions (happiness and satisfaction) have been detected 12. In a pandemic, people can be expected to experience fear, stress, anxiety, distress, irritability and anger, as well as memories of traumatic experiences, difficulty concentrating and sleep problems 13.
The COVID-19 pandemic has affected the mental health of many people around the world and has demonstrated, to a certain extent, how fragile people can be in the face of events that put their health and lives at risk. The COVID-19 pandemic has been a reflection of how a physical disease transcends the biological area to affect the mental area, adding mental manifestations to the common symptoms 14.
Therefore, nursing has an important role as a promoter and manager of the care of people to preserve their lives, this work is not limited to attending to biological conditions but also to meet psychosocial needs. Similarly, nursing is responsible for providing efficient, effective and quality care according to contemporary dynamics, through the care of interpersonal relationships, where different roles are played such as teaching and counseling 15,16.
It is important for the nursing professional to contribute to the improvement of mental health in the population, initially by producing research to explore and learn about the main psychological illnesses present in the population at the time of COVID-19 and the factors associated with these conditions. Subsequently, develop training and support programs on care focused on the implementation of educational support through cognitive-behavioral strategies in order to prevent, control or reduce psychological conditions during this health emergency. Therefore, the objective of this study was to identify the association between sociodemographic factors and depressive symptoms, level of stress and anxiety in times of COVID-19 in inhabitants of the city of Saltillo Coahuila, Mexico.
METHODS
A cross-sectional predictive correlational study design was used 17. The population was inhabitants of the city of Saltillo, Coahuila, Mexico. The sample consisted of 501 participants. For data collection, a virtual online sampling was used in conventional social networks. The survey was made available from October 5 to 24, 2020. Being at least 18 years of age or older was the only inclusion criterion adopted.
A personal data form (CDP) was completed that included questions such as age, sex, marital status, income, occupation, chronic illnesses present, whether the patient lost his job or had his salary reduced because of the pandemic, and whether he followed quarantine health recommendations such as asylum or social distancing. Radolff's Center for Epidemiological Studies Depression Scale (CES-D20) was used to measure depressive symptoms 18. It consists of 20 items, the parameters of the scale are: 0 = no days; 1 = 1 to 3 days; 2 = 4 to 6 days and 3 = every day, the range fluctuates between 0 to 60. The cut-off points are: 0 to 15 with no depressive symptoms, 16 to 20 mild depressive symptoms, 21 to 25 moderate depressive symptoms and scores greater than or equal to 26 severe depressive symptoms. Each item reflects the frequency that was experienced in the last week.
It consists of 20 items, the parameters of the scale are: 0 = no days; 1 = 1 to 3 days; 2 = 4 to 6 days and 3 = every day, the range fluctuates between 0 to 60. The cut-off points are: 0 to 15 with no depressive symptoms, 16 to 20 mild depressive symptoms, 21 to 25 moderate depressive symptoms and scores greater than or equal to 26 severe depressive symptoms. Each item reflects the frequency that was experienced in the last week.
The Perceived Stress Scale (PSS-14) of Cohen, Kamarck and Mermelstein 19) was used to assess the level of stress, designed to measure the degree to which life situations are perceived as stressful. Adapted in Mexico in its Spanish version by González and Landero 20. The PSS-14 has an adequate internal consistency of 0.80. It is a self-report instrument that assesses the level of perceived stress during the last month, consists of 14 items, uses a five-point likert-type response format (0 = never, 1 = almost never, 2 = occasionally, 3 = often, and 4 = very often).
The scale ranges from 0 to 56, with higher scores indicating greater perceived stress. In this research, it was classified into high and low stress levels, and the median of the total score of the scale was taken as a reference. The PSS-14 scale has proven to be reliable and valid for assessing stress symptoms in various populations.
The Generalized Anxiety Disorder Scale (GAD-7) by Spitzer et al., was used to detect anxiety levels 21, initially designed for the detection and measurement of the severity of generalized anxiety disorder, however, it has good operational characteristics for social anxiety disorder. The GAD-7 consists of 7 questions scored between 0 and 3, with minimum and maximum possible scores of 0 and 21. The cut-off points are: 0 - 4 = No anxiety symptoms are appreciated; 5 - 9 = Mild anxiety symptoms are appreciated; 10 - 14 = Moderate anxiety symptoms are appreciated and 15 - 21 = Severe anxiety symptoms are appreciated. The GAD-7 has reported a Cronbach's alpha coefficient of 0.93. With the 10-point cutoff, the sensitivity values were 86.8% and specificity 93.4%.
The digital survey was created by the researchers on the QuestionPro platform. The questions in the scales were adapted to refer to the time spent in quarantine or social isolation due to COVID-19. Subsequently, the survey link was shared through conventional virtual social networks (Facebook, Messenger, Linkedln and WhatsApp) through various groups in some of them. Upon accessing the survey, the informed consent form with a detailed description of the study was presented in the first instance, as well as the researchers' e-mail addresses to answer any doubts that might arise. Those who agreed to participate gave their electronic informed consent and continued with the survey questions. Upon sending their responses, they were thanked for their time and thus concluded their participation. The order of appearance of the instruments on the platform was as follows: 1) CDP, 2) CES-D20, 3) PSS-14 and 4) GAD-7. The approximate filling out time was 10 - 15 minutes and to guarantee anonymity no personal data were collected that could allow the identification of the participants.
Descriptive analyses (measures of central tendency, frequencies and percentages) were used to characterize the study sample. Cronbach's alphas were obtained to obtain the reliability of the instruments. In order to determine the association between sociodemographic variables and the levels of depressive symptoms, stress and anxiety, binary and multinomial logistic regression analysis was performed using Pearson's Chi test and Nagelkerke's R2, which explain the significance of the variables and the percentage of variance explained.
The present study followed the guidelines of the Regulations of the General Law on Health Research 22, Title Two of the ethical aspects of research on human subjects, in order to ensure respect for the dignity of the subjects, the protection of their rights and the use of informed consent. In addition, the ethical recommendations contained in the Declaration of Helsinki were followed 23.
RESULTS
The mean age was 32.69 (SD = 10.32), 68.50% were female and 31.50% male. The 46.90% were single, 39.10% were married and 8.40% were in a common-law relationship. It was found that 25.10% suffered from overweight/obesity, 6.00% from hypertension (HTA) and 5.00% from diabetes (DM). In terms of individual monthly income, 28.90% receive an income of less than 5 thousand Mexican pesos (MN), 33.70% receive between 5,001 and 10 thousand MN and only 12.40% mentioned receiving an income of more than 20 thousand MN.
In terms of monthly family income, 26.70% reported an income of 5,001 to 10 thousand MN, followed by 25.70% who reported an income of more than 20 thousand MN. Regarding the medical coverage of the participants, 66.50% reported being a member of the Mexican Social Security Institute (IMSS), 13.20% of the Institute of Security and Social Services for State Workers (ISSSTE), 8.60% had private medical insurance, and 7.60% reported having no health care services at all.
Regarding occupation, 65.40% are workers in a company or institution, 15.20% are students, and 10.40% are engaged in household activities. 22.60% stated that they or a family member lost their job because of the COVID-19 pandemic. 53.70% said that they stayed at home and did not go to work because of instructions from their workplace, 36.50% have performed work activities from home. Finally, 35.70% said that their salary had decreased due to the situation generated by the COVID-19 containment measures.
Regarding the pathologies suffered by the people living with the participants and which are considered risk factors for COVID-19, 26.90% suffer from DM, 30.10% AHT, 34.70% SP-OB, 7% respiratory problems and 25.70% live with people over 60 years of age.
Regarding depressive symptoms (M = 13.05; SD = 9.75), 64.70% reported no depressive symptoms, 12.80% had mild depressive symptoms, and 11.40% and 11.20% moderate to severe. Regarding the level of stress (M = 21.81; SD = 8.94), 51.90% reported high levels. Regarding the level of anxiety (M = 7.12; SD = 5.08), 42.90% had mild anxiety, 32.10% had no anxiety, 13.60% reported moderate anxiety and 11.40% severe anxiety. Reliability analyses (Cronbach's alpha [α]) of the scales used showed accepTable values in the study sample (CES-D20 α = 0.92; PSS-14 α = 0.86 and GAD-7 α = 0.92). Table 1 presents the relationship between depressive symptoms, level of stress and anxiety and sociodemographic factors.
Table 1. Chi-square analysis: depressive symptoms, stress and anxiety and sociodemographic factors.
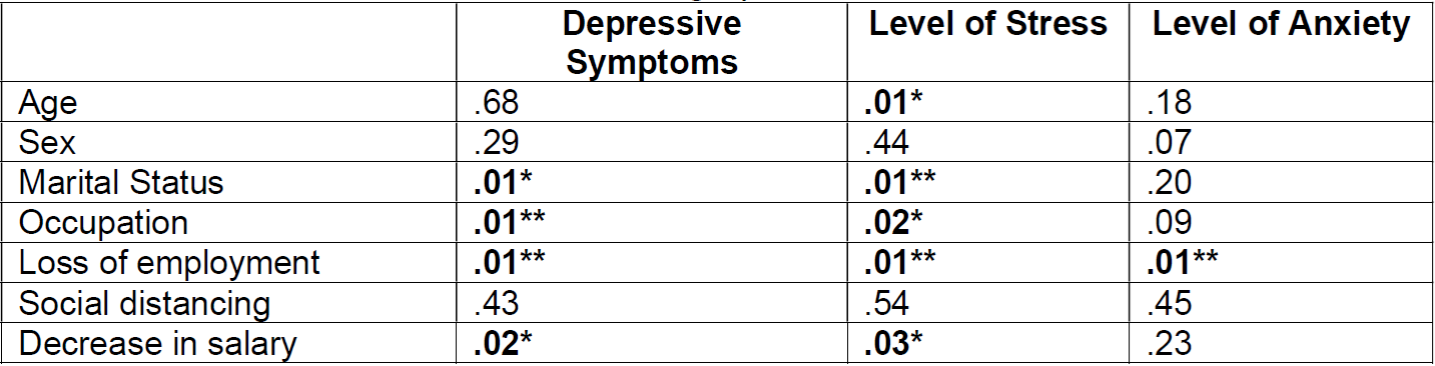
Note: p = < .05*, p = < .01**
To identify sociodemographic factors associated with depressive symptoms derived from the COVID-19 pandemic, a multinomial logistic regression analysis was performed. The model was significant (χ2 = 58.877, gl = 15, p = ˂ .001). Pearson's chi-square test (χ2= 718.606, gl = 702, p = ˂.324) and chi-square deviation (χ2 = 551.947, gl = 702, p = 1.000) indicated a good model fit. Nagelkerke's R2 was .127, which predicts 12.70% of the variance. The model showed that younger participants were .93 (95% CI: .900 - .979) more likely to suffer moderate depressive symptoms. Those without a partner (OR = 2.64; 95% CI: 1.347 - 5.201), unemployed (OR = 2.43; 95% CI: 1.330 - 4.453) and who lost their job or a family member because of the COVID-19 pandemic (OR = .35; 95% CI: .191 - .664) were more likely to suffer severe depressive symptoms.
To observe the association between sociodemographic variables and stress level, a binary logistic regression analysis was developed. The analysis indicates that the null model has a 52% probability, the model was significantly (χ2 = 60.570, gl = 6, p = ˂ .001). The Hosmer and Lemeshow test (χ2 = 3.477, gl = 8, p = ˂ .901) indicates a good model fit. The Nagelkerke R2 was .148, which predicts 14.80% of the variance. With the ranking, it is observed that the model predicts 62.60% compared to the null model. It was found that younger participants were .95 more likely to have elevated stress levels. And those who did not lose their jobs because of the pandemic were .37 less likely to have elevated stress levels.
A multinomial logistic regression analysis was performed to identify the sociodemographic variables associated with the level of anxiety. The model was significant (χ2 = 64.442, gl = 27, p = ˂.001). Pearson's Chi test (χ2 = 1111.84, gl = 1095, p = ˂ .355) and the Chi-square deviation (χ2 = 921.180, gl = 1095, p = 1.000) indicated a good model fit. The Nagelkerke R2 was .132, which predicts 13.20% of the variance. It was detected that if the participant or a family member lost their job because of the pandemic they had .49 (95% IC: .283 - .865) the probability of presenting levels of mild anxiety was higher. Age was negatively associated with the level of anxiety, so that people with lower number of years were more likely to have mild anxiety .94 (95% IC: .916 - .983) higher probability of presenting moderate anxiety levels. Being female (OR = 2.48; 95% IC: 1.254 - 4.941) and not having a partner (OR = 1.95; 95% IC: 1.015 - 3.774) were associated with a higher probability of presenting moderate anxiety levels.
Likewise, being female (OR = 2.37; 95% CI: 1.144 - 4.915) and being unemployed (OR = 2.62; 95% CI: 1.308 - 5.254) were related to a higher probability of suffering severe anxiety. The loss of the participant's job or that of a family member due to the pandemic (OR = .31; 95% CI: .149 - .654) and reporting family income of less than 5 thousand MN (OR = .23; 95% CI: .068 - .812) or between 5001 and 10 thousand MN (OR = .29; 95% CI: .119 - .747) were associated with a higher probability of presenting severe anxiety levels.
DISCUSSION
The present research work identified associations between sociodemographic factors and depressive symptoms, stress level and anxiety in times of COVID-19 pandemic. The results show similar data to those reported by Lei et al., 24 who found high levels of depressive symptoms (50.70%), anxiety (44.70%) and stress (73.40%). Similar data to those of Elbay et al., 25 where 64.70% had depressive symptoms, 51.60% had anxiety symptoms and 41.20% had stress-related symptoms and to those of Wang et al., 26 who observed moderate to severe psychological stress in more than half of the respondents and about one third reported moderate to severe anxiety.
Significant relationships were also found between the variables of interest and some sociodemographic factors (age, marital status, occupation, job loss and salary decrease) by means of chi-square. These results differ from some research showing that apart from the factors mentioned above, suffering from chronic degenerative diseases were related to depressive symptoms, stress and anxiety 27,28, characteristic that was not found in this study, which can be attributed to the low percentage of chronic diseases in the study sample. However, Parrado-González and León-Jariego 29 mentioned that being a woman and having a lower level of income had a greater psychological impact and worse mental health.
One possible cause is the purchasing power in the country, being Mexico a developing country, the economic and sociocultural issues have a considerable impact, as do other Latin American countries. This can be corroborated with the results of Johnson et al., 30 where they point out that the impact on mental health of COVID-19 is unequal according to gender, educational level and perceived comfort at home, in addition to the social and economic consequences of the measure of isolation for daily, social and work life.
Furthermore, the Economic Commission for Latin America and the Caribbean 31 points out that because of COVID-19 the social situation is deteriorating, due to the increase in poverty and extreme poverty indices, the persistence of inequalities and widespread discontent. In other words, the health crisis will have negative repercussions on health and education, as well as on employment and poverty, factors that have been related to the risk of suffering depressive symptoms, stress and anxiety, which affect mental health.
Regarding the associations identified between sociodemographic variables and depressive symptoms in this research, the youngest participants and people without a partner were at the highest risk. Data similar to those reported by Lei et al., 24 indicate that the younger age group had higher and more significant depressive symptoms than the older group, and that not having a romantic relationship was related to suffering depressive symptoms.
Lozano-Vargas 32 found that older people presented high levels of psychological stress, which differs in this research, as it was found that younger participants were .95 more likely to present elevated stress levels. It has been reported that women are twice as likely to suffer from stress and anxiety 33. Female gender has been identified as a predictor of post-traumatic stress disorder symptoms after pandemics 21. This is consistent with the results of this research, where being a woman was associated with a higher probability of presenting moderate anxiety levels.
One possible explanation is that young people's sudden change in their academic, social and other activities due to isolation caused negative changes in their behavioral patterns, affecting their mental health. In women, the likelihood of presenting higher levels of anxiety may be attribuTable to the emotional burden of the protective role of caring for the family or the overload of domestic activities that comes with family members spending more time at home. Furthermore, it has been reported that the hormonal factor may have an influence, especially if they are exposed to a danger or risk such as COVID-19.
Choi et al., 34 found that participants with medium-high family income presented lower levels of anxiety than families with medium-low income. Data similar to those of this research, since losing their job and reporting a family income of less than 10 thousand MN was associated with a higher probability of presenting severe anxiety levels. The loss of employment brings with it the loss of income, a situation that can generate high levels of anxiety due to not being able to meet their needs, and can be complicated in the case of having economic dependents.
The results presented allowed to know possible diseases present in the population due to the COVID-19 quarantine, such as depressive symptoms, stress and anxiety, and some sociodemographic characteristics that were associated with these conditions. It is hoped that the findings of this study can be useful for nurses and serve as a basis for future research to expand existing knowledge and thus develop programs to promote mental health. Nurses must face the challenges generated by the current pandemic, innovate in their professional practice and position themselves in the scientific community and the general population to strengthen mental health care practices through e-Health, the use of ICTs and interdisciplinary work 14.
One of the main limitations of this research is that due to the cross-sectional nature of the research, it was not possible to observe changes in the variables of interest over time. In addition, at the moment it is not possible to apply any sampling method other than virtual online, due to pandemic containment measures. Therefore, there is a possibility of selection bias, as individuals without access to the Internet, a device, or virtual social networks could not be included in this study. However, the findings may be useful for the scientific and health community to establish action plans where contextual and personal factors should be considered and related to mental health.
CONCLUSION
An association was found with age, economic income and sex with the different psychological variables of interest (depressive symptoms, level of stress and anxiety) in times of COVID-19. Health professionals are urged to consider mental health as a priority to cope with this health crisis. According to projections, the pandemic may extend over several years and affect the mental health of people who are still in confinement and social isolation. These results project preliminary data in the Mexican context, and the development of interventions to reduce depressive symptoms, stress and anxiety is needed. Finally, more large-scale studies should be conducted in different contexts in Mexico, including rural areas, and incorporate other factors that may better explain the phenomenon under study.
REFERENCIAS
1. Organización Mundial de la Salud. Preguntas y respuestas sobre la enfermedad por coronavirus (COVID-19); World Helth Organization. [Internet]. 2020. [acceso: 15/11/2020]. Disponible en: https://www.who.int/es/emergencies/diseases/novel-coronavirus-2019/advice-for-public/q-a-coronaviruses [ Links ]
2. Zhou, P., Yang, X. L., Wang, X. G., Hu, B., Zhang, L., Zhang, W., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. [Internet]. 2020. [acceso: 15/11/2020]; 579 (7798): 270. Disponible en:https://doi.org/10.1038/s41586-020-2012-7 [ Links ]
3. Johns Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)". ArcGIS. [Internet]. 2021. [acceso: 26/04/2021]. Disponible en: https://coronavirus.jhu.edu/map.html [ Links ]
4. Secretaria de Salud. Covid-19 México: Información General. [Internet]. 2021. [acceso: 26/04/2021]. Disponible en: https://datos.covid-19.conacyt.mx [ Links ]
5. Organización Mundial de la Salud. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19-11. World Helth Organization. [Internet]. 2020. [acceso: 15/11/2020] Disponible en: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-may-2020 [ Links ]
6. American Psychological Association. Pandemics. [Internet]. 2020. [acceso: 25/10/2020]. Disponible en: https://www.apa.org/practice/programs/dmhi/research-information/pandemics [ Links ]
7. Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. [Internet]. 2020. [acceso: 26/10/2020]. 14; 395 (10227): 912. Disponible en: https://doi.org/10.1016/S0140-6736(20)30460-8 [ Links ]
8. Lippi, G., Henry, B., Bovo, C., Sanchis-Gomar, F. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19). Diagnosis. [Internet]. 2020. [acceso: 26/10/2020]. 26;7(2):85-90. Disponible en: https://www.degruyter.com/document/doi/10.1515/dx-2020-0041/html [ Links ]
9. Johnson, M. C., Saletti-Cuesta, L., Tumas, N. Emociones, preocupaciones y reflexiones frente a la pandemia del COVID-19 en Argentina. Cien Saude Colet. [Internet]. 2020. [acceso: 27/10/2020]. 25 (suppl 1): 2447. Disponible en: https://doi.org/10.1590/1413-81232020256.1.10472020 [ Links ]
10. Xiao C. A Novel Approach of Consultation on 2019 Novel Coronavirus (COVID-19)-Related Psychological and Mental Problems: Structured Letter Therapy. Psychiatry Investig. [Internet]. 2020. [acceso: 27/10/2020]. 17(2):175. Disponible en: https://doi.org/10.30773/pi.2020.0047 [ Links ]
11. Zandifar A, Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J Psychiatr. [Internet]. 2020. [acceso: 28/10/2020]. 51:101990. Disponible en: https://doi.org/10.1016/j.ajp.2020.101990 [ Links ]
12. Ho CS, Chee CY, Ho RC. Mental Health Strategies to Combat the Psychological Impact of COVID-19 Beyond Paranoia and Panic. Ann Acad Med Singap. [Internet]. 2020. [acceso: 27/10/2020]. 16;49(3):155. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32200399/ [ Links ]
13. Taylor, S. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. Cambridge Scholars Publishing. [Internet]. 2019. Disponible en: https://cambridgescholars.com/product/978-1-5275-3959-4 [ Links ]
14. Martinez-Esquivel D. Desafíos para la enfermería de salud mental después del COVID-19. Rev. cienc. cuidad. [Internet]. 2020 [acceso 08/02/2021]. 17(3):122-9. Disponible en: https://doi.org/10.22463/17949831.2413 [ Links ]
15. Chen SC, Lai YH, Tsay SL. Nursing perspectives on the impacts of COVID-19. J Nurs Res. [Internet]. 2020. [acceso: 27/04/2021]. 28(3). Disponible en: https://doi.org/10.1097/NRJ.0000000000000389 [ Links ]
16. Courtenay M, Burnett E, Castro-Sanchez E, Figueiredo RM, Toit B, Gallagher R, et al. Preparing nurses for COVID-19 response efforts through involvement in antimicrobial stewardship programmes. J Hosp Infect. [Internet]. 2020. [acceso: 27/04/2021]. 106(1):176-8. Disponible en: https://doi.org/10.1016/j.jhin.2020.06.011 [ Links ]
17. Osingada CP., Porta CM. Nursing and Sustainable Development Goals (SDGs) in a COVID-19 world: the state of the science and a call for nursing to lead. Public Health Nurs. [Internet]. 2020. [acceso: 28/04/2021]. 37(5):799-805. Disponible en: https://doi.org/10.1111/phn.12776 [ Links ]
18. Stirling B., Hatcher J., Harmston J. Communicating the Changing Role of a Nurse in an Epidemic: The Example of the MERS-CoV Outbreak in Saudi Arabia. J Healthc Commun. [Internet]. 2017. [acceso: 28/04/2021]. 02(03). Disponible en: http://doi.org/10.4172/2472-1654.100070 [ Links ]
19. Lluch Canut MT. Enfermería de salud mental: El arte y la ciencia del cuidar. Revista española de enfermería de salud mental. [Internet]. 2018. [acceso 09/02/2021]. 4: 2-3. Disponible en: http://doi.org/10.35761/reesme.2018.4.01 [ Links ]
20. Peplau H. Relaciones interpersonales en Enfermería. Un marco de referencia conceptual para la Enfermería psicodinámica. Barcelona: Salvat Editores S.A.; 1990. [ Links ]
21. Gray, J. R., Grove, S. K., Sutherland, S. Burns and Grove's. The Practice of Nursing Research: Appraisal, Synthesis, and Generation of Evidence. Elsevier Health Sciences. [Internet]. 2017. Disponible en: https://www.elsevier.com/books/burns-and-groves-the-practice-of-nursing-research/gray/978-0-323-37758-4 [ Links ]
22. Radloff, L. S. The CES-D scale: A self-report depression scale for research in the general population. Applied psychological measurement. [Internet]. 1977. [acceso: 29/10/2020]. 1(3), 385. Disponible en: https://doi.org/10.1177/014662167700100306 [ Links ]
23. Cohen, S., Kamarck, T., Mermelstein, R. A global measure of perceived stress. Journal of health and social behavior, [Internet]. 1983. [acceso: 29/10/2020]. 24(4), 385. Disponible en: https://doi.org/10.2307/2136404 [ Links ]
24. González, M. T., Landero, R. Factor structure of the Perceived Stress Scale (PSS) in a sample from Mexico. Spanish Journal of Psychology. [Internet]. 2007. [acceso: 29/10/2020]. 10(1), 199. Disponible en: https://pubmed.ncbi.nlm.nih.gov/17549893/ [ Links ]
25. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. [Internet]. 2006. [acceso: 30/10/2020]. 22;166(10):1092. Disponible en: https://doi.org/10.1001/archinte.166.10.1092 [ Links ]
26. Secretaria de Salud. Reglamento de la ley general de salud en materia de investigación para la salud. 1987 [Internet]. [acceso: 03/11/2020]. Disponible en: http://mail.repssguerrero.gob.mx/ipo2019/transparencia/3er_trim/Frac_I/REGLAMENTO_DE_LA_LEY_GENERAL_DE_SALUD_EN_MATERIA_DE_PROTECCION_SOCIAL_EN_SALUD.pdf [ Links ]
27. World Medical Association. Declaración de Helsinki - Principios éticos para las investigaciones médicas en seres humanos. 64ª Asamblea General. Fortaleza, Brasil. 2013. [Internet]. [acceso: 05/11/2020]. Disponible en: http://repositorio.mederi.com.co/bitstream/handle/123456789/386/Declaracion-Helsinki-2013-Esp.pdf?sequence=1 [ Links ]
28. Instituto Nacional de Estadística y Geografía (INEGI). Salud y seguridad social: Derechohabiencia. [Internet]. 2020. [acceso: 28/04/2021]. Disponible en: https://inegi.org.mx/temas/derechohabiencia/ [ Links ]
29. Lei, L., Huang, X., Zhang, S., Yang, J., Yang, L., Xu, M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Med Sci Monit. [Internet]. 2020. [acceso: 15/11/2020]. 26: e924609-1. Disponible en: https://doi.org/10.12659/MSM.924609. [ Links ]
30. Elbay RY, Kurtulmus A, Arpacioglu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. [Internet]. 2020. [acceso: 15/11/2020]. 290:113130. Disponible en: https://doi.org/10.1016/j.psychres.2020.113130 [ Links ]
31. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. [Internet]. 2020. [acceso: 25/11/2020] 6;17(5):1729. Disponible en: https://doi.org/10.3390/ijerph17051729 [ Links ]
32. Dong XC, Li JM, Bai JY, Liu ZQ, Zhou PH, Gao L, et al. Epidemiological characteristics of confirmed COVID-19 cases in Tianjin. Zhonghua Liu Xing Bing Xue Za Zhi. [Internet]. 2020. [acceso: 06/12/2020]. 10;41(5):638-641. Disponible en: https://doi.org/10.3760/cma.j.cn112338-20200221-00146. [ Links ]
33. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. [Internet]. 2020. [acceso: 22/12/2020]. 30;36(4):e00054020. Disponible en: https://doi.org/10.1590/0102-311X00054020 [ Links ]
34. Parrado-González A, León-Jariego JC. COVID-19: Factores asociados al malestar emocional y morbilidad psíquica en población española. Rev Esp Salud Pública. [Internet]. 2020. [acceso: 07/02/2021]. 94: 8 e202006058. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32507849/ [ Links ]
35. Johnson MC, Saletti-Cuesta L, Tumas N. Emociones, preocupaciones y reflexiones frente a la pandemia del COVID-19 en Argentina. Ciência & Saúde Coletiva. [Internet]. 2020. [acceso: 09/02/2021]. 25, 2447-2456. Disponible en: https://doi.org/10.1590/1413-81232020256.1.10472020 [ Links ]
36. Comisión Económica para América Latina y el Caribe. América Latina y el Caribe ante la pandemia del COVID-19: efectos económicos y sociales. 2020. [Internet]. [acceso: 08/02/2021]. Disponible en: https://repositorio.cepal.org/handle/11362/45337 [ Links ]
37. Lozano-Vargas, A. Impacto de la epidemia del Coronavirus (COVID-19) en la salud mental del personal de salud y en la población general de China. Rev de Neuropsiquiatr. [Internet]. 2020. [acceso: 20/12/2020]. 83(1), 51. Disponible en: http://dx.doi.org/10.20453/rnp.v83i1.3687 [ Links ]
38. Foa EB, Street GP. Women and traumatic events. J Clin Psychiatry. [Internet]. 2001. [acceso: 28/12/2020]. 62 Suppl 17:29-34. Disponible en: https://pubmed.ncbi.nlm.nih.gov/11495093/ [ Links ]
39. Choi EPH, Hui BPH, Wan EYF. Depression and Anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. [Internet]. 2020. [acceso: 28/12/2020] 25;17(10):3740. Disponible en: https://doi.org/10.3390/ijerph17103740 [ Links ]
Received: March 03, 2021; Accepted: April 24, 2021











 texto en
texto en 


