Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.21 no.65 Murcia ene. 2022 Epub 28-Mar-2022
https://dx.doi.org/10.6018/eglobal.481541
Originals
Prevention of sexually transmitted infections among young people and the importance of health education
1 Enfermero. Doctorando en Enfermería por la Universidad del Estado de Rio de Janeiro (UERJ), Rio de Janeiro, RJ, Brasil laerciodl28@hotmail.com
2 Enfermera. Especialista em Enfermería en Salud de la Famiília por el Programa de Residencia de Enfermería en Salud de la Famiília de la Universidad del Estado de Rio de Janeiro (UERJ), Rio de Janeiro, RJ, Brasil..
3 Enfermera. Doctora en Enfermería. Profesora Asociada del Departamento de Fundamentos de Enfermería de la UERJ, Rio de Janeiro, RJ, Brasil.
4 Enfermera. Alumna de Máster del programa de Posgraduación em Enfermería de la UERJ, Rio de Janeiro, RJ, Brasil.
5 Alumna de Grado de Enfermería de la UERJ. Bolsista de Iniciación Científica del CNPq, Rio de Janeiro, RJ, Brasil.
Objective:
To analyze sexual practices and the adoption of prevention practices for sexually transmitted infections among university students.
Method:
A descriptive, cross-sectional and quantitative study, carried out in a public higher education institution, located in the city of Rio de Janeiro. A sample of 173 students from the Nutrition, Medicine, Nursing and Biological Sciences courses was selected from the matrix research database.
Results:
There was predominance of young women (76.88%), aged between 18 and 23 years old (84.39%), sexually active (78.03%), who did not use condoms continuously with sTable (47.22%) and casual (30.36%) partners; the majority negotiated condom use (37.78%); never performed a test to detect HIV (56.07%) and denied previous occurrence of STIs (91.33%).
Conclusion:
The low adherence of young people to condoms with sTable and casual partners is a risky sexual behavior that can contribute to acquiring STIs. Expansion of the provision of timely testing and intensification of educational activities in the university environment are necessary practices to reduce the group's vulnerability to STIs.
Keywords: sexually transmitted diseases; young adult; sexual behavior; students; education in health
INTRODUCTION
Sexually Transmitted Infections (STIs) are caused by microorganisms such as viruses, fungi and bacteria and their main form of transmission is sexual. There is a high incidence of STIs, being considered one of the most common public health problems worldwide. In the social and health context, they represent an important cause of morbidity and mortality, although their visibility has only increased since the 1980s with the emergence of AIDS1.
The STI terminology − replacing the expression Sexually Transmitted Disease (STD) − has been used more frequently in order to warn about the possibility of being a carrier of any of these infections even if the individual remains asymptomatic2.
A number of studies show that, of the 4,500 new cases of infections by the Human Immunodeficiency Virus (HIV) in adults worldwide recorded in 2016, 35% occurred among young people aged 15 to 24 years old and that, every week, approximately six thousand women aged between 15 and 24 years old are infected with HIV3. In Brazil, the Epidemiological Bulletin of the Ministry of Health (Ministério da Saúde, MS)4 has recorded an increase in the number of AIDS cases among young people aged from 15 to 24 years old and indicates that most of the cases reported in the country were recorded in the age group of 20 to 34 years old, showing the need for preventive and health education actions aimed at this specific group2.
Considering the epidemiological aspects, STIs represent an important problem in the sexual and reproductive health of young people, and may trigger some health problems such as infertility, pelvic inflammatory diseases, cervical cancer and infections in newborns2. One of the main ways to prevent the occurrence of new infections is through the continuous use of condoms5.
Young people are considered a vulnerable group to acquire an STI, considering the presence of Risk Sexual Behaviors (RSBs), such as early initiation of sexual life, discontinuous or incorrect use of condoms, occurrence of multiple partners, and use of alcohol and/or drugs. In addition to that, considering the social changes involved, factors related to entering the university environment can increase the occurrence of risky sexual behaviors6.
Currently, it is understood that comprehensive care for people with STIs should result from the combination of different services through combined prevention. This, in turn, comprises three strategic areas: individual and collective prevention, provision of diagnosis and treatment, and management. Thus, access to education in health, condom use, timely testing for STIs and vaccination are some examples of the essential prevention components in the management of STIs2, thus justifying conduction of this research.
Most of the studies that evaluate university students present a sample consisting of courses in the health area6,7. Investigating students in the biomedical area becomes opportune considering that, even if they are students in the health area, the theme is little improved during college or in their work process, which can directly reflect on the young university students' sexual behaviors.
Given this context, the objective of this research was to analyze the sexual practices and those for the prevention of sexually transmitted infections adopted by university students.
MATERIAL AND METHOD
This is a descriptive and cross-sectional study with a quantitative approach, carried out in a higher education institution located in the municipality of Rio de Janeiro, Brazil. The study is integrated into the research entitled Sexuality and vulnerabilities of young people in times of sexually transmitted infections. It is added that the authors of this study participated in the stages of data collection and storage of the research data and that the research coordinator authorized the use of the data to carry out this study. The matrix research was carried out in a public higher education institution located in the municipality of Rio de Janeiro between 2018 and 2019.
The sample selected from the matrix research database for this study is of the intentional non-probabilistic type, composed of students attending the Nutrition, Medicine, Nursing and Biological Sciences courses, teaching units that make up the university's biomedical center, totaling 173 participants. As inclusion criteria, the participants were students of both genders, aged between 18 and 29 years old, regularly enrolled in undergraduation courses at the institution, which was the research locus. Students who were absent due to illness or enrollment cancellation during the data collection period did not participate in the research.
The choice of the sample set for this research is justified, considering the author's interest in knowing the sexual practices and those for the prevention of STIs among undergraduate students in the health area. It is added that, considering the participation of the main author in the residency in Family Health Nursing, after data collection, an educational activity was carried out with the group of students related to the prevention of STIs.
To capture the data in the matrix research, a self-administered structured questionnaire with 60 closed questions was used, previously validated by the “Survey of Knowledge, Attitudes and Practices in the Brazilian Population”, carried out by the Ministry of Health in 2008, 2011 and 2013 in the form of a population survey aimed at people between 15 and 64 years of age8. The Data Collection Instrument (DCI) was adapted by the researchers to the specificities of the population group under study (university students between 18 and 29 years old) and contained socioeconomic and behavioral variables and those referring to knowledge and prevention of STIs.
It is worth mentioning that, aiming at internal validity and reliability, the DCI was previously tested, carrying out a pilot test with 10 university students to verify objectivity, clarity and relevance to the objectives proposed. Thus, during the assessment by experts on the subject matter, adjustments were made to the questionnaire, and the instruments used in the pilot test phase were discarded. Considering that this study is part of a larger research study, ten socioeconomic variables were selected from the DCI: fifteen on sexual practices and five on prevention practices that met the objective of this research.
Data collection for this research took place at two moments, in 2018 and 2019, between the students' classes, with the purpose of not disturbing the dynamics in the classrooms. The mean time to answer the DCI was 20 minutes. After collection, the data were tabulated and organized in the Excel program from Microsoft Office 2013 for Windows. Most of the variables selected for this study were qualitative and dichotomous.
For data treatment and analysis, the resources of descriptive statistics with uni- and bi-variate analysis were used. The results were presented in absolute and percentage frequencies, and discussed in the light of the (inter)national scientific literature.
The research was previously submitted and approved by the Research Ethics Committee of the institution where the research was conducted, with consubstantiated opinion number 3,396,324. The participants had already signed the Free and Informed Consent Term (FICF) after being informed about the potential risks, benefits, objectives and purposes of the research, as provided for in Resolution 466/2012.
RESULTS
The study included 173 undergraduate biomedical students from a public institution located in the municipality of Rio de Janeiro. The social characteristics of the students show that 133 (76.88%) are female; 146 (84.39%) are aged between 18 and 23 years old; 97 (56.07%) are single and without affective relationships; 169 (97.69%) did not have children; 142 (82.08%) declared themselves heterosexual; 141 (81.50%) did not work; 91 (52.60%) declared themselves white-skinned; 118 (68.21%) considered themselves religious, predominantly followers of the Catholic (39.83%) and Evangelical (38.98%) religions; and 138 (79.77%) lived with their parents.
When asked about sexual practices, 135 (78.03%) answered that they were sexually active and 95 (70.37%) used condoms in the first sexual intercourse that occurred between the ages of 15 and 18 years old (71.85%), with no difference between the gender. As for sexual partners, 73 (54.07%) reported that they had never had more than one sexual partner in their entire lives; 100 (74.07%) denied having had sexual intercourse with more than one partner in the same period; 112 (82.96%) denied having sex with men and women in the same period; and 82 (60.74%) reported not using condoms in all their sexual relations.
Condom use, type of sexual partner and condom negotiation are described in Table 1.
Table 1. Distribution of the students attending a public university according to the type of sexual partner, condom use and negotiation. Rio de Janeiro, 2021.

Source: Database of the Youth Sexuality and Vulnerability Survey in Times of Sexually Transmitted Infections. Note: NI - Not Reported; NA - Not Applicable.
As for the use of condoms in all sexual relations, it was verified that there is a greater number of university students who are married or with a sTable partner who do not use condoms in all sexual relations, when compared to single students, as described in Table 2.
Table 2. Distribution of the university students in a public institution according to marital status and condom use in all sexual relations. Municipality of Rio de Janeiro, 2021 (n=135).

Source: Database of the Youth Sexuality and Vulnerability Survey in Times of Sexually Transmitted Infections
By associating condom negotiation and its use in all sexual relations, it was verified that the students who fully or partially negotiate do not use condoms in all sexual relations, as shown in Table 3.
Table 3. Condom use and negotiation in all sexual relations by university students attending a public institution. Municipality of Rio de Janeiro, 2021. (n=63).
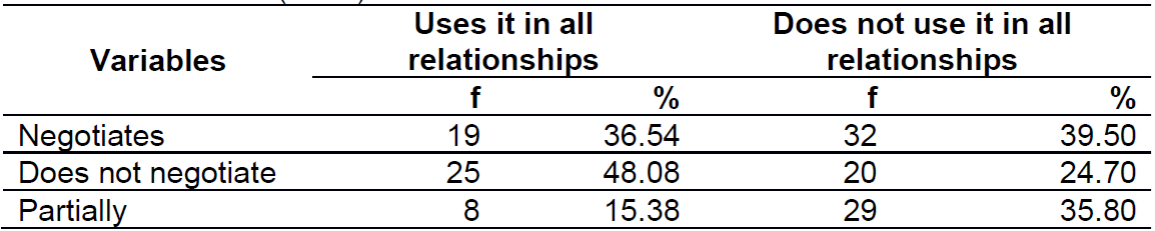
Source: Database of the Youth Sexuality and Vulnerability Survey in Times of Sexually Transmitted Infections.
When the young women in the study were asked about use of the female condom, 97 (97.98%) reported never having used it during sexual intercourse.
As for the use of alcohol or drugs before the last intercourse, 41 (65.08%) admitted it. When asked about the possibility of acquiring an STI, 96 (55.49%) university students stated it was little possible and 28 (16.18%) believed that it was impossible to acquire an STI.
Regarding the occurrence of STIs in the investigated group, 158 (91.33%) denied any event. Among the STIs mentioned by the participants, candidiasis (42.86%), HPV (28.57), herpes (14.29%), syphilis (7.14%) and chlamydia (7.14%) stand out.
When asked about testing to detect HIV, 97 (56.07%) reported never having been tested. The students who had already underwent the test pointed out the following reasons: blood donation, betrayal, curiosity, admission exam or request provided for in a public tender. Such exams were performed after unprotected sexual intercourse and after the recommendation of a health professional.
The performance of cytopathological and gynecological examinations among the women who participated in the study are described in Table 4.
DISCUSSION
According to data from the 2018 Higher Education Census, 14.9% of the university students are enrolled in undergraduate courses in the areas of health and well-being, are predominantly female, white-skinned, and the most frequent age is 19 years old. The findings of this research are similar to those of the Census9. The current trend is for young people to enter university at an earlier age; this is considered a defining moment in their lives, characterizing the initial contact with the world of work10.
Regarding skin color, in this study, 91 (52.60%) declared themselves white-skinned, corroborating the 2010 Demographic Census in which 47.7% of the population declared themselves white-skinned and 43.1%, brown-skinned11.
Upon entering university, young people can have their sexual behavior influenced by different factors, such as new friends and interaction with people with different lifestyle habits from their own and their newly acquired freedom10. Lack of access to safe information, absence of discussions in opportune environments such as the university and early initiation of sexual life are described as factors that increase the chance of acquiring HIV among young people12.
Young university students are categorized as an at-risk population segment when considering the probability of developing RSBs, due to the weak sense of vulnerability and to the little attention received due to the low morbidity and mortality rates, when compared to other population groups7,13.
A number of research studies show that most university students are sexually active and that they had their first sexual relation when aged between 12 and 17 years old7,10. A literature review carried out with 123 articles evidenced that, in young people, sexual initiation ranged between the ages of 13 and 18 years old, with a mean of 15 in most of the studies, results that are close to those of this research14. Thus, early initiation of sexual activity, associated with other factors, makes the young person vulnerable to STIs15.
The male condom is the most popular contraceptive method among young people. It is a device that is easy to handle and freely distributed by the public health services, and its use is directly related to the chances of contracting an STI; on the other hand, the female condom is difficult to be found in public services for free distribution and, often, even for purchase in pharmacies and related stores10,16. A study carried out in the United States in 2017 showed that many high school students are involved in risky behaviors for sexual health, associated with unplanned pregnancy and sexually transmitted infections, such as HIV. Regarding adherence to condom use in the last intercourse, its use was higher among heterosexual students (56.1%) than among gays, lesbians and bisexuals (39.9%). Prevalence was also higher among heterosexual male students (61.8%) than among heterosexual women (49.6%)17.
A study carried out with university students indicates that most of the women did not have sexual relations using female condoms, corroborating the findings of the research. Difficulty of access, availability, handling and cost are pointed out as the main reasons for the device to have lower adherence among women, making the male condom more popular18.
Advanced age, partner's age or the use of any contraceptive method are factors pointed out for not using condoms in the first sexual relation16. Among the reasons listed by young people for not using the device are trust in the partner, use of other contraceptive methods, choice of partner, religious issues and the stigma of reduced sexual pleasure12,19.
A number of research studies1)(10)(18)(19 indicate that unprotected sex is more common among young people with sTable relationships, corroborating the findings of this research, that women are less likely to negotiate its use, and that there is a reduction in use of the device with increasing age. However, it should be noted that having a sTable partner is not a safe way to avoid STIs, and that the likelihood of contracting STIs is directly related to continued condom use10.
Regarding condom use negotiation, young people who negotiate do not do so continuously. A number of research studies indicate that condom use negotiation is more present in casual relationships and that women are at a disadvantage when negotiating with their partners, considering gender issues, power relations and historical differences between men and women10,20.
Considering the consumption of (il)licit drugs, it is known that abusive use of alcohol can affect judgment, decisions and discernment20. A number of studies indicate that use of alcoholic beverages is directly related to the higher prevalence of RSBs and that use of illicit drugs in the last sexual relation increased by more than 100% the chance of presenting some RSB7,20.
In the investigated group, young people find it little possible or impossible to acquire an STI. A study carried out with university students from 80 undergraduate courses in Rio Grande do Sul identified HPV, genital herpes and gonorrhea as the most frequent among young people7, corroborating the findings of this study. Previous history of STIs and having the first sexual relation at a young age are identified as significant variables among young people with STIs22.
As a way of preventing STIs, HIV and viral hepatitis, the MS recommends combined prevention that articulates biomedical, behavioral and structural interventions. Considering the expansion of the term “safe sex”, combined actions are proposed between testing for STIs, pre- and post-exposure prophylaxis, condom use, early diagnosis and adequate treatment of STIs, harm reduction, antiretroviral treatment, immunization and prevention of vertical transmission2.
Screening for STIs must be performed annually in people under 30 years of age, through rapid tests in asymptomatic individuals. In this study, there was a significant number of young people who had never performed rapid testing. A number of research studies indicate that most young people do not undergo the HIV test and that, among the reasons, fear of a possible positive diagnosis or not wanting to know about the infection stand out23,24.
In the investigated group, it is noticed that, although young people are aged between 18 and 23 years old, most of the women report having undergone the Pap smear. A number of studies indicate that performing a gynecological examination in asymptomatic and non-pregnant women can generate overdiagnosis, anxiety and unnecessary costs, and is not routinely recommended, and screening should be avoided before the age of 2525,26. However, the nurse should encourage the woman to go to the health unit to carry out timely STI screening through rapid tests and gynecological examination2,27.
In Brazil, the screening method for cervical cancer is the cytopathological examination, which must be carried out annually in the first two years; if both results are negative, every three years. Collection must be carried out in women aged from 25 to 64 years old who have already started their sexual life25. Educational actions, information about the test before it is performed, and good care provided by trained health professionals are cited as strategies to favor women's adherence to the Pap smear test10.
Considering the importance of offering actions aimed at preserving the health of the young population, the Family Health Strategy (FHS) implemented by the MS arises to reorganize the health care model, and its practices prioritize actions of prevention, promotion and recovery of users based on care integrality and longitudinality28. The purpose of health promotion is to collaborate with the confrontation of social determinants of health through the expansion of knowledge, (self-)care and autonomy. Group activities, general guidelines and integration between different sectors, such as articulation between health and education through the School Health Program (Programa Saúde na Escola, PSE), are some of the strategies adopted by the FHS to promote health29.
Among the various activities developed by the FHS teams, health promotion actions rely on the adoption of educational actions and activities with the aim of strengthening the individual's self-care through the control of the social determinants of health30. Regarding rapid testing, the nurse has technical and legal competence to request and perform the exam, for pre- and post-test counseling, report issuance, referrals and scheduling31.
Educational practices must be conducted considering a relationship of dialog and respect between educator and student. The search for reflection on a reality in a continuous and active process within the humanizing educational context provides for its transformation. The learning process needs to articulate scientific knowledge, common sense and the individual so that the information has, in fact, some meaning and is incorporated in people's lives29.
A number of studies indicate that the educational activities with young people developed by FHS professionals provide opportunities for the exchange of ideas, knowledge and experiences, as well as they strengthen the bond between young people and professionals28.
Education in health is a resource used by health professionals to exert a positive impact on people's lives. Sexual education constantly encounters barriers based on the argument that it promotes promiscuity and the early initiation of sexual life; however, its main result is to contribute to reducing the risk of STIs and unwanted pregnancies28.
Education in health is indispensable for the promotion of healthy habits and prevention; however, it is fundamental for nurses to be able to seek appropriate and assertive strategies during their work process29. Among some of the strategies used to carry out education in health, conversation circles are considered to facilitate the process, as they help to strengthen ties and increase adherence to the activity and provide constant feedback28. Another strategy is to include the young person in the planning of activities by choosing the themes to be worked on, making the young person active in the elaboration of activities developed by the FHS29.
In addition to that, it is fundamental that health education actions are interdisciplinary with the multidisciplinary team, breaking the logic of fragmented care, with practices that are disconnected from public policies and focused on the disease29.
Sexual health in educational institutions depends on a multidisciplinary team to promote, protect and restore young people's health. Inserted in the school environment, the nurse can act as a mediator, supporting educational actions and working with teachers in the articulation between school, family and community30. In this scenario, it is considered that the FHS nurse is indispensable for strengthening combined prevention and for reducing the number of STIs among young people.
CONCLUSION
In this study, it was possible to assess the sexual practices and those for the prevention of STIS adopted by university students. The findings show that there was predominance of women, aged between 18 and 23 years old, who present risky sexual behaviors and low adherence to condom use in sexual relations, both with sTable and casual partners. In addition to that, considering the concept of combined prevention, there is a significant number of young people who have never been tested for HIV.
Thus, it is necessary to expand the offer of timely testing for STIs, in view of the low adherence of the investigated group to the exam, as well as to intensify educational practices in the university environment to favor the dissemination of information and reduce the students' vulnerability to STIs.
Conducting this research only with university students in the biomedical area is a study limitation, and replication with young people from other areas of knowledge is opportune. However, the findings are similar to other studies that show low adherence to condom use and the assumption of risky behaviors by the young collective.
This study can contribute to encouraging new research studies related to the performance of educational practices among young people, considering the need to reformulate the existing practices. In addition to that, the discussion on the prevention of STIs in this population group highlights the importance of creating and formulating specific public policies to contribute to reducing the number of STI cases in this population group.
REFERENCES
1. Spindola T, Teixeira RS, Sodré CP, Santana RSC, André NLNO, Costa SW. Condutas de jovens universitários frente a prevenção de infecções sexualmente transmissíveis: perspectiva de gênero. Rev Paraninfo Digital [Internet] 2017 [cited 2020 May 11];27. Avaiable from: http://www.index-f.com/para/n27/279.php [ Links ]
2. Ministério da Saúde (Br). Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Protocolo Clínico e Diretrizes Terapêuticas Infecções Sexualmente Transmissíveis. Brasília: Ministério da Saúde, 2019. [cited 2020 Oct. 25] Avaiable from: http://www.aids.gov.br/pt-br/pub/2015/protocolo-clinico-e-diretrizes-terapeuticas-para-atencao-integral-pessoas-com-infeccoes [ Links ]
3. World Health Organization. Communities at the center, 2019. Avaiable from: https://www.unaids.org/sites/default/files/media_asset/2019-global-AIDS-update_en.pdf [ Links ]
4. Ministério da Saúde (Br). Secretaria de Vigilância em Saúde. Boletim Epidemiológico: HIV AIDS 2019. Brasília (DF): Ministério da Saúde. 2019. Avaiable from: http://www.aids.gov.br/pt-br/pub/2019/boletim-epidemiologico-de-hivaids-2019 [ Links ]
5. Alirol E, Wi TE, Bala M, Bazzo ML, Chen XS, Deal C, et al. Multidrug-resistant gonorrhea: a research and development roadmap to discover new medicines. PLoS Med. 2017 [cited 2020 Oct. 25];14(7):e1002366. Avaiable from: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002366 [ Links ]
6. Scull TM, Keefe EM, Kafka JM, Malik CV, Kupersmidt JB. The understudied half of undergraduates: Risky sexual behaviors among community college students. J Am Coll Health. 2020 [cited 2020 Oct. 25];68(3):302-312. Avaiable from: 10.1080/07448481.2018.1549554 [ Links ]
7. Gräf DD, Mesenburg MA, Fassa AG. Risky sexual behavior and associated factors in undergraduate students in a city in Southern Brazil. Rev. Saúde Pública [Internet]. 2020. [cited 2020 May 5];54:41. Avaiable from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-89102020000100235&lng=pt. [ Links ]
8. Ministério da Saúde (Br). Departamento de IST, Aids e Hepatites Virais. Pesquisa de Conhecimentos, Atitudes e Práticas (PCAP) na população brasileira 2013. [Internet] Brasília: Ministério da Saúde, 2016. [cited 2021 Jul 17]. Avaiable from: http://www.aids.gov.br/pt-br/pub/2016/pesquisa-de-conhecimentos-atitudes-e-praticas-na-populacao-brasileira-pcap-2013 [ Links ]
9. Ministério da Educação (Br). Instituto Nacional de Estudos e Pesquisas Educacionais Anísio Teixeira. Resumo técnico do Censo da Educação Superior 2019. Brasília: Ministério da Educação, 2019. [cited 2020 Oct. 25] Avaiable from: http://portal.inep.gov.br/resultados-e-resumos [ Links ]
10. Spindola T, Araújo ASB, Brochado EJ, Marinho DF, Martins ERC, Pereira TS. Sexual practices and attitudes of university students towards prevention of sexually transmitted infections. Enf Global [Internet]. 2020 [cited 2020 Oct. 25];19(2):109-40. Avaiable from: https://revistas.um.es/eglobal/article/view/382061. [ Links ]
11. Ministério da Educação (Br). Censo demográfico 2010. Brasília: Instituto Nacional de Estudos e Pesquisas Educacionais Anísio Teixeira, 2011. [ Links ]
12. Carmo BAG, Quadros NRP, Santos MMQ, Macena JKF, et al. Health education on sexually transmissible infections to Nursing College students. Rev. bras. promoç. Saúde. (Impr.) 2020 [cited 2020 Oct. 25];33:10285. Available from: https://periodicos.unifor.br/RBPS/article/view/10285/pdf [ Links ]
13. Kassie BA, Yenus H, Berhe R, Kassahun EA. Prevalence of sexually transmitted infections and associated factors among the University of Gondar students, Northwest Ethiopia: a cross-sectional study. Reprod Health. 2019 [cited 2020 Oct. 25];16(1):163. available from:10.1186/s12978-019-0815-5 [ Links ]
14. Moraes L, Franca C, Silva B, Valença P, Menezes V, Colares V. Early sexual debut and associated factor: a literature review. 2019 Psic., Saúde & Doenças [Internet]. [cited 2020 Oct. 20];20(1):59-73. Avaiable from: http://www.scielo.mec.pt/scielo.php?script=sci_arttext&pid=S1645-00862019000100005&lng=pt. http://dx.doi.org/10.15309/19psd200105 [ Links ]
15. Sales JKD, Sales JKD, Alves DA, Coelho HP, Oliveira OP, Santos RL. Fatores de risco associados ao comportamento sexual de adolescentes. REAS [Internet]. 2020 [cited 2020 Oct. 25]. Avaiable from: https://www.acervomais.com.br/index.php/saude/article/view/3382 [ Links ]
16. Grubb LK. Barrier protection use by adolescents during sexual activity. Committee on Adolescence Pediatrics [Internet] 2020 [cited 2020 Sept. 19];146(2). Avaiable from: https://pediatrics.aappublications.org/content/146/2/e2020007237 [ Links ]
17. Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B., et al. Youth risk behavior surveillance - United States, 2017. Morbidity and mortality weekly report. Surveillance summaries. 2018 [cited 2020 Oct. 10];67(8):1-114. Avaiable from: 10.15585 / mmwr.ss6708a1 [ Links ]
18. Araújo A, Spindola T, Sousa K, de-Araújo A, Martins E. Sexual health care practices of university young people. Revista de Pesquisa: Cuidado é Fundamental Online [Internet]. 2020 [cited 2021 Apr. 11];12(0):1215-1220. Avaiable from: doi: https://doi.org/10.9789/2175-5361.rpcfo.v12.8626 [ Links ]
19. Santangelo OE, Provenzano S, Grigis D, Terranova A, D'Anna G, Armetta F, et al. Why nursing students have sex without condom? A study in the university of Palermo. Clin Ter. 2020 [cited 2020 Oct. 10];171(2):e130-e136. Avaiable from: https://pubmed.ncbi.nlm.nih.gov/32141484/ [ Links ]
20. Souza FMA, Muñoz IK, Visentin IC. Contexto de vulnerabilidade de gênero no uso do preservativo masculino. Finom [Internet] 2020 janeiro-julho. [cited 2020 Oct. 25];20(1). Avaiable from: http://revistas.icesp.br/index.php/FINOM_Humanidade_Tecnologia/article/view/1004 [ Links ]
21. Dallo L, Martins RA. Association between the risk of alcohol use and unprotected sex in adolescents in a city in the southern region of Brazil. Ciênc. saúde coletiva [Internet]. 2018 [cited 2020 Sept. 15];23(1):303-314. Avaiable from: https://doi.org/10.1590/1413-81232018231.14282015 [ Links ]
22. Aguirrebengoa OA, Garcia MV, Sanchez MR, D'Elia G, Méndez BC, Arrancudiaga MA et al. Risk factors associated with sexually transmitted infections and HIV among adolescents in a reference clinic in Madrid. PLoS ONE. 2020 [cited 2020 Sept. 15];15(3). Avaiable from: https://doi.org/10.1371/journal.pone.0228998 [ Links ]
23. Lima MS, Raniere JC, Paes CO, Gonçalves LHT, Cunha CLF, Ferreira GRON et al. The association between knowledge about HIV and risk factors in young Amazon people. Rev. Bras. Enferm. [Internet] 2020 [cited 2020 Oct. 25];73(5):e20190453. Avaiable from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-71672020000500182&lng=en [ Links ]
24. Fu G, Shi Y, Yan Y, Li Y, Han J, Li G, et al. The prevalence of and factors associated with willingness to utilize HTC service among college students in China. BMC public health [Internet] 2018. [cited 2020 Oct. 25]; 18(1):1050. Avaiable from: https://doi.org/10.1186/s12889-018-5953-0 [ Links ]
25. Ministério da Saúde (Br). Instituto Nacional de Câncer José Alencar Gomes da Silva. Coordenação de Prevenção e Vigilância. Divisão de Detecção Precoce e Apoio à Organização de Rede. Rio de Janeiro: INCA 2016. [ Links ]
26. Qin J, Saraiya M, Martinez G, Sawaya GF. Prevalence of potentially unnecessary bimanual pelvic examinations and papanicolaou tests among adolescent girls and young women aged 15-20 years in the United States. JAMA Intern Med [Internet]. 2020 [cited 2020 Oct 15];180(2):274-280. Avaiable from:10.1001/jamainternmed.2019.5727 [ Links ]
27. Ministério da Saúde (Br). Protocolos da Atenção Básica: Saúde das Mulheres / Ministério da Saúde, Instituto Sírio-Libanês de Ensino e Pesquisa - Brasília : Ministério da Saúde, 2016. 230 p. [ Links ]
28. Oliveira M, Lanza L. Health education: sexually transmitted diseases and pregnancy in adolescence. Revista da Faculdade de Ciências Médicas de Sorocaba. 2018 [cited 2020 Dec 12];20(3):138-141. doi: https://doi.org/10.23925/1984-4840.2018v20i3a4 [ Links ]
29. Silva RF, Engstrom EM. Comprehensive health care of teenagers by the Primary Health Care in the Brazilian territory: an integrative review. Interface - Comunicação, Saúde, Educação [online]. 2020 [cited 2021 Jan 7];24(suppl 1):e190548. Avaiable from: https://doi.org/10.1590/Interface.190548 [ Links ]
30. Brixner B, Muniz C, Renner J, Pohl H, Garcia E, Krug S. Health promotion actions in family health strategies. Cinergis [Internet]. 2017 [cited 2020 Dec 12]; 18(Supl. 1):386-390. Avaiable from: https://online.unisc.br/seer/index.php/cinergis/article/view/11182 [ Links ]
31. Silva ITS, Lima DM, Santos WN, Santos RSC, Menezes HF, Silva RAR. Análise da operacionalização da testagem rápida para o HIV realizada pelo enfermeiro. Revista Recien. 2020 [cited 2020 Dec 12];10(29):100-111. Avaiable from: https://www.recien.com.br/index.php/Recien/article/view/339 [ Links ]
Accepted: May 29, 2021; Received: September 14, 2021











 texto en
texto en 



