Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.2 mar./abr. 2006
Multiple sclerosis as first manifestation in oral and facial
area:
Presentation of four cases
Esclerosis multiple como primera
manifestacion en el territorio oral y facial:
Presentación de cuatro casos
Lola Gallud 1, José V. Bagan2, Angeles Cervelló3, Yolanda Jiménez4,Rafael Poveda5, Carmen Gavalda6
(1) Stomatologist Doctor, Stomatology Department, Hospital
General Universitario
(2) Professor of Mouth Medicine, Universidad de Valencia. Head of Stomatology Department,
Hospital General Universitario
(3) Head of Neurology Department, Hospital General Universitario
(4) Associate Professor of Mouth Medicine, Universidad de Valencia. Senior Professor Stomatology Department,
Hospital General Universitario
(5) Senior Professor, Stomatology Department, Hospital General Universitario
(6) Associate Professor of Mouth Medicine, Universidad de Valencia
ABSTRACT
Multiple sclerosis (MS) is a chronic inflammatory disease of
the central nervous system, whose etiology is unknown, and which is
characteristic by the appearance of a diverse neurological symptomatology
consisting of outbreaks or gradual deterioration and lesions in any location of
the brains white matter which may provoke the after-effect of a definitive
demyelination of the area.
The disease affects young people, with its appearance being
most frequent between 20 and 40 years of age, in temperate and cold climates,
and with a man-woman rate of 0.46 / 0.67.
The magnitude of this disease lies in the fact that it is the
primary cause for permanent disablement among young adults.
We are presenting 4 cases of MS whose initial symptom of the
disease was the appearance of paraesthesia in the maxillofacial area, affecting
one or more ramifications of the trigeminal nerve, and a progression time
varying from 15 days to one year.
All the patients were clinically diagnosed, with their
diagnostics being confirmed both with magnetic resonance imaging as well as
through the study of their cerebrospinal fluid (CSF) and the evoked potentials (EPs).
Manifestations in the oral and facial area were the first
manifestation of the disease in all cases.
Key words: Facial paraesthesia, multiple sclerosis.
RESUMEN
La esclerosis múltiple (EM) es una enfermedad
inflamatoria crónica del sistema nervioso central de etiología no conocida
caracterizada por la aparición de sintomatologia neurológica diversa en forma
de brotes o de deterioro progresivo y de lesiones en cualquier localización de
la sustancia blanca cerebral que pueden dejar como secuelas la desmielinización
definitiva de la zona.
Esta enfermedad afecta a gente joven siendo más frecuente su aparición entre
los 20 y 40 años, en climas templados y fríos y con una relación hombre-mujer
de 0,46 / 0,67.
La importancia de esta enfermedad radica en que es la primera causa de invalidez
permanente en adultos jóvenes.
Presentamos 4 casos de EM cuyo síntoma de inicio de la enfermedad fue la
aparición de parestesias en el territorio maxilo-facial afectando a una o más
ramas del trigémino y de tiempo de evolución que oscilaba entre 15 días y un
año.
Todos los pacientes fueron diagnosticados clínicamente siendo confirmado el
diagnostico, tanto con la resonancia magnética como con el estudio del liquido
cefalorraquídeo (LC) y los potenciales evocados (PE).
Las manifestaciones en el territorio oral y facial fueron la primera manifestación
de la enfermedad en todos los casos.
Palabras clave: Parestesia facial, esclerosis múltiple.
Introduction
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system (CNS), whose etiology is unknown and which may be caused by multiple factors, and it is thought that a genetic predisposition together with immunity and environmental factors could trigger the disease. (1,2)
MS is a disease affecting young people. It appears most frequently among individuals from 20 to 40 years old, at intervals of 10 to 60 years. It affects more women than men, in a proportion of 0.67 /0.46, and it occurs in cold and warm climates. In the world distribution of the disease, Spain ranks among the countries with a high frequency and prevalence, with a rate, varying depending on studies, between 15-25 patients every 100,000 inhabitants. (3,4)
MS represents a complex clinic alteration, presenting a highly diverse symptomatology as a result of the demyelination of the CNS, and a later slow down or blocked transmission at the level of axons. Ectopic impulses may also appear, providing positive signs (paroxysms, convulsions). The combination of these negative and positive signs inform the base of its great variability and variegated clinic symptomatology. (5,6)
Given its progression in outbreaks or in the form of gradual deterioration, and in order to be able to assess its clinic severity, MS has been internationally classified in 4 subtypes.-
1. -RelapsingRemitting (RR). 2- Progressive-Relapsing (PR). 3. - Secondary-Progressive (SP) .4. - Primary-Progressive (PP).
RR is the most frequent form of presentation of MS, accounting for 85% of cases. This clinic subtype is characterized by the appearance of outbreaks resolved with or without sequelae, interspersed with periods of clinic stability. These patients may remain 10 15 years in a more or less stable condition, before progressing towards SP, with the progress of the disease in that clinic form being slow. On the contrary, in 15% of cases the disease presents a progressive (PR) or sharp (PP) progress from its inception. In those cases the disease does not progress in outbreaks, and from the very beginning there are acute relapses with occasional stabilizations and less and less improvements, with a quick progress towards disability and therefore with a worse prognosis. (1,5)
Clinically MS usually appears with a number of symptoms of neurological anomalies which settle in a mater of minutes or hours, and which frequently progress in later days, where the most frequent are: visual and oculomotor anomalies (49 %) - optical neuritis, anterior internuclear ophthalmic paralysis. Palsies (43%) in the form of partial or incomplete palsies, locomotor weakness, clumsiness in hands, etc. Paraesthesia (41%) that is, alteration of feeling such as numbness of arms, legs, face, etc. Signs of lack of motor coordination (23%), or tonic spasms. Genito-urinary dysfunction (10%), urination urge, increase of urination frequency, lack of bladder control and episodic retention of urine. Signs of brain damage (4%) such as paroxysmal ataxia and dysarthria or shaking of upper limbs. (5,6)
Once the disease has settled, the signs of neurological anomaly are usually coupled with paroxysmal alterations, such as tonic spasms and involuntary movements, nystagmus, trigeminal neuralgia, episodic dysarthria, ataxia, episodes of intense itching, etc lasting minutes or even seconds, and which lead us to catalogue patients as suffering from anxiety or even hysteria. (1,5-7)
MS is a disease difficult to diagnose given its variable forms of presentation and symptomatology. Therefore, progress in image diagnostic techniques has been crucial when it comes to accurate diagnostics. MS diagnostic is still clinical, although cranial and spinal studies through magnetic resonance imaging (MRI), evoked potentials and the analysis of the cerebrospinal fluid (CSF) are the main diagnostic exploration used for the confirmation of clinical data. (1,7,8)
Currently, the criteria followed for a definite diagnostic of MS are based on the confirmation of its progression in time and space, of its symptoms and signs. These criteria were developed by a committee of neurologists and published in 2001 by McDonald et al (9), who based their work on the magnetic resonance MS diagnostic criteria. (1,8-10)
The progress and prognosis of MS are not predictable. However, there are certain criteria which may lead us to a worse prognosis, namely: an advanced age at the appearance of the disease, being a male, the initial cerebellar or motor clinical study, the number of outbreaks in the first two years, the brief time interval between them, or family history.(11).
There are three goals in the treatment of MS: to shorten the duration of the outbreak, to alter the natural progress of the disease, and to reduce it to a symptomatic condition.
The treatment of the outbreaks has the goal of reducing the duration of relapses, an improvement of symptoms, and a prevention of complication. Treatment requires the use of steroids either orally or by pulses of methylprednisolone of 1000mg IV / day.
The immunomodulatory treatment, aimed at preventing the progress of the disease, differs depending on the various progressive forms of MS, with Betaferon being the most effective in the RR forms, and symptomatic treatment aimed at improving the quality of life of these young patients by reducing their symptoms and attempting to minimize their disabilities. (1,12,13).
Clinical Trials
The reason for this work is the presentation of 4 clinic cases of MS whose first manifestations were in the maxillofacial area.
The clinical cases of the four cases of MS presented by us included in table 1, with the patients having been visited in the Stomatology and Neurology Departments of the Hospital General Universitario of Valencia throughout 2004.
Our patients were 3 women and one men, aged between 27 and 54. All of them described an initial symptomatology of the appearance of tingling sensations, numbness, strange sensations in their faces affecting one or more ramifications of the trigeminal nerve, the most frequent being the second and third ramification, lasting in time although varying in intensity.
The male patient (case 1), who went to the department as soon as the first symptoms appeared, was developing his first outbreak. A multiplicity of neurological manifestations gradually appeared and made his hospitalisation necessary. On the contrary, the beginning of the three other cases was much more insidious, for the disease manifested itself only through paraesthesias, with the effect that the patients delayed reporting to the clinic. In case 4, the patient suffered from dysesthesias, that is, sensorial deficits coinciding with neuralgic pains spontaneously appearing and disappearing, without a complete disappearance of the symptoms. Throughout the course of the last year, the patient has had a severe outbreak with a feeling of dizziness, instability in walking, general discomfort, nauseas and vomits, requiring hospitalisation.
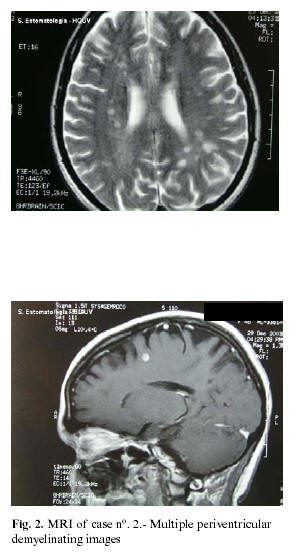
In all cases, given the clinical conjecture (fig. 1), MRI was carried out (fig. 2), a study of the CSF and of the visual, auditory and bodysensorial evoked potentials in order to be able to confirm the disease. In all of them, the MRI shows the characteristic demyelination in different locations of the white matter, with the CSF positive in cases 1 and 4, and positive evoked potentials in case 4, all of them meeting the diagnostic criteria set by Mc Donald et al (9).
Discussion
As we have already said, MS is a disease characterized by the appearance of multiple neurological symptomatology. Therefore, the appearance of PARAESTHESIAS in the oral and facial area is an ALARMING SYMPTOM which should made us suspicious of the existence of a possible neurological problem, something that would force us to focus our intervention on an early diagnostic after a thorough clinical exploration aimed at discarding any either local or general iatrogenic pathology which could be responsible for the hypoesthesia. Subsequently, we must complete our diagnose with MRI and an assessment by the neurological department aimed at confirming the MS.(1-5)
An early diagnosis is critical in the prognosis of the disease (11) because, as we have already pointed out, it is an inflammatory process which, when it becomes chronic, leads to the definitive demyelization of the area. If there is a treatment in the early stages of the process consisting of the suppression of the inflammatory outbreaks, we will be directly acting on the development of the disease and therefore improving the patients quality of life (12-13). Diagnosis is not always easy, for MS is normally considered when an optic neuritis or a diplopia appears in a young adult. However, it is hard to imagine that such a serious neurological process is behind facial paraesthesias, and it is easier to label these patients as suffering from anxiety, depression or from a temporomandibular joint pathology or muscle contracture. Sometimes they are classified as atypical facial pain (2,14), and are usually patients who, on arriving at our practice, have already seen other professionals and followed a number of ineffective treatments. Therefore, we ought to consider the progression time as longer than what we are being told and that our quick diagnosis will improve the possible quality of life of those patients.
![]() Correspondence
Correspondence
Dra. Lola Gallud Romero
E-mail: gallud_lola@ono.com
Received: 5-03-2005
Accepted: 20-12-2005
References
1. Antigüedad A, Zarranz JJ, Mendibe MM. Enfermedades Desmielinizantes. En: Zarranz JJ, eds Neurología. España: Elsevier; 2003. p. 593-612. [ Links ]
2. Raymond D. Adams, Maurice Víctor, eds. Principios de Neurología. Barcelona: Reverté S.A; 1988. p. 714-21. [ Links ]
3. Kurtzke John.F Epidemiología de la Esclerosis Múltiple. En Raine Cedric S, McFarland Henry F, Tourtellotte Walace W, eds. Esclerosis Múltiple. Bases clínicas y patogénicas. Madrid: Edimsa; 2000. p. 91-131. [ Links ]
4. Mallada Frenchin J. Epidemiología descriptiva de la Esclerosis Múltiple en España. En: Fernández O, Bello P, eds cuadernos de Esclerosis Múltiple. Madrid: Alcora publicidad S.L.; 2004. p. 58-66. [ Links ]
5. Whitaker John N,Mitchell Galen W. Características clínicas de la Esclerosis Múltiple. En Raine Cedric S, McFarland Henry F, Tourtellotte Walace W, eds. Esclerosis Múltiple. Bases clínicas y patogénicas. Madrid: Edimsa; 2000. p. 3-19. [ Links ]
6. Luchinetti Claudia F, Rodríguez Moses. Patogénia de la enfermedad inflamatoria desmielinizante. En Fernández O, Bello P, eds Cuadernos de Esclerosis Múltiple. Madrid: Alcora publicidad S.L.; 2004. p. 131-54. [ Links ]
7. Duane E Haines ed. Principio de neurociencia. Madrid: Elsevier Science ; 2003. p. 101-3. [ Links ]
8. Poser Charles M, Brinar Vesna V. Criterios diagnósticos para la Esclerosis Múltiple. Una revisión histórica. En: Fernández O, Bello P, eds. Cuadernos de Esclerosis Múltiple. Madrid: Alcora publicidad S.L. Editores; 2004. p. 217-46. [ Links ]
9. McDonald W, Compson A, Edan G, Hartung H, Lublin F, McFarland H, et al. Recommended Diagnostic Criteria for Multiple Sclerosis.;guidelines from the international panes on diagnosis of multiple sclerosis. Ann Neurol 2001;50:121-7. [ Links ]
10. Donald W Paty. Técnicas de Resonancia Magnética útiles en la Esclerosis Multipke. En Fernández O, Bello P, eds. Cuadernos de Esclerosis Múltiple. Madrid: Alcora publicidad S.L.; 2004. p. 395-412. [ Links ]
11. Arbizu Urdiain T, Martínez Yelamos S. Evolución y pronostico de la Esclerosis Múltiple. En Fernández O, Bello P, eds. Cuadernos de Esclerosis Múltiple. Madrid: Alcora publicidad S.L.; 2004. p. 247-54. [ Links ]
12. Gonsette Richard E. Tratamiento precoz de la progresión en la Esclerosis Múltiple. En: Fernández O, Bello P, eds. Cuadernos de Esclerosis Múltiple. Madrid: Alcora publicidad S.L.; 2004.p. 471-87. [ Links ]
13. Donald E, Goodkin. Esclerosis Múltiple terapias actuales modificadoras de la enfermedad. En Raine Cedric S,McFarland Henry F, Tourtellotte Walace W, eds. Esclerosis Múltiple. Bases clínicas y patogénicas. Madrid: Edimsa; 2000. p. 307-20. [ Links ]
14. Chemaly D, Lefrancois A, Perruse R. Oral and maxillofacial manifestations of multiple sclerosis. J Can Dent Assoc 2000;6611:600-5. [ Links ]











 texto en
texto en