Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 no.2 mar. 2007
Odontogenic calcificant cystic tumor: A report of two clinical cases
Daniel Reyes, Julio Villanueva, Sebastián Espinosa , Marco Cornejo
Departamento de Cirugía y Traumatología Maxilofacial, Facultad de Odontología, Universidad de Chile, Santiago de Chile. Unidad de Cirugía Maxilofacial, Hospital Clínico San Borja-Arriarán, Santiago de Chile
ABSTRACT
Odontogenic Calcificant Cystic Tumor (OCCT) is an infrequent injury. It arises from odontogenic epithelial rests present in the maxilla, jaw or gum. Gorlin and col. described the OCCT for first time as an own pathological entity in 1962. Clinically, the OCCT represents 1% of the odontogenic injuries. It is possible to be found from the first decade to the eighth decade. It affects in same proportion the maxilla and the jaw, being the most common in the dented zones, with greater incidence in the first molar area.
Two case reports of OCCT in two different ages, both in female individuals, one at 5 years old and the other at 35 years old are presented. Enucleation of the tumor was the treatment chosen. The purpose of this article is to present a review of the literature related to these two cases of OCCT and its treatment, putting an emphasis on its aetiology, biological behaviour and treatment.
Key words: Odontogenic tumors, odontogenic calcificant cystic tumor, Gorlin cyst.
RESUMEN
El tumor odontogénico calcificante quístico (TOCQ) es una lesión poco frecuente. Ésta deriva de restos epiteliales odontogénicos presentes en los maxilares, mandíbula o encía.
El TOCQ fue descrito por primera vez como una entidad patológica propia por Gorlin y col. en 1962. Clínicamente, el TOCQ corresponde al 1% de las lesiones odontogénicas. Se puede manifestar desde el primer año hasta la octava década de la vida. Afecta por igual los maxilares y la mandíbula, siendo más común en las zonas dentadas, con incidencia algo mayor en las zonas anteriores al primer molar.
Se presentan 2 casos clínicos de TOCQ en dos etapas de la vida, ambos en el sexo femenino, uno a los 5 y el otro a los 35 años de edad. El tratamiento fue la enucleación del tumor.
El objetivo de este artículo es presentar una revisión de la literatura a propósito de dos casos de TOCQ y su tratamiento, atendiendo a la bajísima incidencia de esta lesión, poniendo énfasis en su etiología, comportamiento biológico y tratamiento.
Palabras clave: Tumores odontogénicos, tumor odontogénico calcificante quístico, quiste de Gorlin.
Introduction
In agreement to the new classification of the World Health Organization (WHO) (2005), the Odontogenic Calcificant Cystic Tumor constitutes a benign cystic neoplasia that presents an epithelium similar to an Ameloblastoma, with ghosts cells which may display calcifications in it (1). It is a rare lesion arising from epithelial odontogenic rests present in the maxilla, mandible or gum (2-10).
Clinically, the OCCT corresponds to 1% of the odontogenic injuries (4,8), the age range between 5 and 92 years old (1), although some authors describe them between the first year and the eight decade (11). Several articles have informed that the greater incidence takes place in the second decade (2,4,5,11), but other authors have noticed a bimodal distribution with a second peak of incidence in the sixth and seventh decade of life (11). It does not have predilection for race or sex (1,2,12), affecting in same proportion the maxilla and the jaw (1), with more recurrence in the dented zones, and greater incidence in relation to the first molar (2,4,7). It can be found in an extra-osseal or intra-osseal location (1,2,4,8,10,13). The extra-osseal injuries are well-defined, smooth pink colorated mucous, above 4 cm. diameter (1). On the other hand, the intra-osseal injuries produce buccal and lingual cortical expansion (2). The most frequent sign is a swelling of variable consistency, painless at palpation (2), which many times it becomes a radiographic finding. Ganglion commitment does not exist.
Radiographically, radiolucid unilocular (1,2) and, occasionally, multilocular images are seen (3,11,13) with well-circumscribed limits that contains diffuse radiopacities areas (2,11). In younger patients the injuries can be confused with a developing odontoma or ameloblastic fibroodontoma (2). Extra-osseal OCCT may show oval forms and sometimes there is displacement of adjacent teeth (1). On the other hand, intra-osseal OCCT is a radiolucid, well-defined image (1). Near a 50% of the cases there are radioopacities in the center of the lesion, teeth dislacerations and root resorptions. Intra-osseal OCCT in relation to un-erupted teeth has been reported (1).
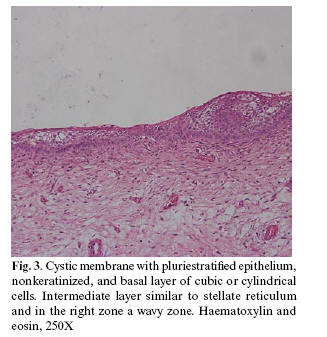
Microscopically, the epithelial component is constituted by an external layer of cylindrical basal cells and an internal layer resembling reticulum remembres (2,4,8,10,14). In both types of OCCT, the cystic wall is linear as a thin ameloblastic epithelium with big epithelial eosinophils cells without visible nuclei, known as "ghosts cells" and that may be calcified (1,2,5,8,11,14-16). In the adjacent connective tissue, odontogenic epithelium proliferation and displasic dentin can be seen (1).
The treatment of the OCCT is the enucleation of the injury without recurrence in most of the cases (1,2,4,5,7-10). Intra-osseal variety recurrence has been report (1).
The purpose of this article is to present two cases of OCCT, in two different ages.
Case 1
A 5-year-old female without relevant medical history presented an asymptomatic swelling on the left cheek of two months of evolution.
The extraoral examination denoted an increase in volume in the left cheek that rises to the wing of the nose not involving the nasolabial line. Skin of the zone had no compromise.
The intraoral examination presented an increase in volume, hard at palpation that occupied the buccal aspect in relation to the left superior temporal canine and that includes from the left zygomatic alveolar crest up to 1 cm. before the middle line, 3.5 cm. of diameter and from the bottom of the buccal aspect to the attached smooth surface asymptomatic gum, showing no suppuration, low growing and normal mucous aspect. There was not systemic compromise.
The CT scan showed an osteolitic injury of cystic aspect, expansion of bony tables without infiltration of soft tissues (Fig. 1).
Incisional biopsy was made under general anaesthesia. Diagnosis revealed odontogenic calcificant cystic tumor, where a cystic membrane had non-keratinized pluristratified epithelium, palsied basal cells layer and a tendency to form stellate reticulum. Basophilic calcifications with round forms are observed and hyaline and eosinophilic material with some ghosts cells adjacent to it. Dentinoid and enamel tissues in relation to the interdental papillae were described (Fig 2,3). Pathologist proposed development of an odontoma in that zone. During the enucleation of the tumor, heavy walls were observed which facilitated its complete excision.
After the surgical treatment and a year follow up, there were no complications and no clinical and radiographic signs of recurrence.
Case 2
A 35-year-old female without relevant medical history was referred to our service for an asymptomatic swelling in the right cheek of one year of evolution.
The extraoral examination denoted a right facial swelling.
There was no compromise of the skin.
The intraoral examination presented cortical expansion in the buccal aspect, hard at palpation, that occupied the bottom of the buccal aspect from approximately 1,5 cm. anterior to the right tuberosity to the middle line and from the bottom of the lobby to the attached smooth surface gum. Asymptomatic, slowly growing with normal mucous was observed in relation to it.
The radiographic exams showed a radiolucent, unilocular with defined margins and with diffuse calcifications in its centre in relation of the right superior canine (un-erupted).
Incisional biopsy was made under local anaesthesia. The histopathologic diagnosis was odontogenic calcificant cystic tumor. Similar findings were seen as in case 1.
Later, under local anaesthesia, it was made the surgical enucleation of the tumor. During the intervention, heavy walls were observed which facilitated its complete extirpation.
The postoperative evolution was satisfactory without complications after one year following. No signs of recurrence were seen.
Discussion
The incidence of the OCCT represents 1% of all cysts in the maxillofacial territory (4,8). Gorlin and al described it in 1962 (7-16).
In relation to the morphoanatomy, the location of the OCCT could be intra-osseal or extra-osseal (1,2,4,8,10,13). Both cases presented correspond to intra-osseal variant and the common sign for both cases was an increase of asymptomatic non-tender swelling, without ganglion compromise.
Aetiology is very controverted. The principal characteristic of the OCCT is the presence of ghost cells, which can also be found in other injuries, such as Malherbe calcificant epithelioma of the skin, ameloblastic fibroodontoma, complex and compound odontoma, craneofaringioma, meloblastoma and carcinoma(1,8). The nature of these cells is not clearly known. Nevertheless, the accepted theory is that there would be a squamous metaplasia of the epithelium with the subsequent queratinization that could be normal or aberrant (8). Radiographically, unilocular (1,2) and, occasionally, multilocular images are seen (3,11,13) with well-circumscribed limits that contains diffuse radiopacities areas (1,2,11). Both cases presented a radiolucid unilocular image of defined margins. Only the second case showed diffuse calcifications in its centre.
Both cases were in women, the first was diagnosed on the first decade of life and the second to the fourth decade of life, both in maxilla, in dented areas and in the anterior zone.
Due to the clinical characteristics of this injury, the differential diagnosis of the OCCT must be done regarding to ameloblastoma, dentigerous cyst and keratocyst. In more advanced stages it could be confused with calcifying epithelial odontogenic tumor, fibroodontoma, adenomatoid odontogenic tumor and partially mineralized odontoma (2).
In relation to the treatment, it must be conservative by means of enucleation or local resection, given its low rate of recurrence (1,2,4,5,7-10,16). The lack of recurrence depends on the excision completion. In both cases, a conservative treatment was decided, making the complete enucleation of the tumor. No complications were reported during a year follow-up. However, further one-year controls must be done during 10 years for possible recurrences.
Acknowledgements: The authors wish to express their gratitude to Dr. Benjamín Martinez for the disinterested in the help histological processing of the tissue samples and for the photography.
References
1. Praetorius F, Ledesma-Montes C. Calcyfing cystic odontogenic tumour. En: Barnes L, Eveson JW, Reichart P, Sidransky D Eds. Who classification of tumours. Pathology and genetics. Head and neck tumours. Chapter 6. Lyon: IARC; 2005. p. 313. [ Links ]
2. Sapp PJ, Eversole RL, Wysocki PG, eds. Patología Oral y Maxilofacial Contemporánea. Madrid: Ediciones Harcourt; 1998. p. 138-9.
3. Erasmus JH, Thompson IO, van Rensburg LJ, van der Westhuijzen AJ. Central calcifying odontogenic cyst. A review of the literature and role of advanced imaging techniques. Dentomaxillofac Radiol 1998;27:30-5.
4. Orsini G, Fiorini M, Rubini C, Piattelli A. Peripheral calcifying odontogenic cyst. J Clin Periodontol 2002;29: 83-6.
5. Tse KM, To EW. Central calcifying cyst. Case report. Aust Dent J 1995;40:357-9.
6. Yoshiura K, Tabata O, Miwa K, Tanaka T, Shimizu M, Higuchi Y, et al. Computed tomographic features of calcifying odontogenic cysts. Dentomaxillofac Radiol 1998; 27:12-6.
7. Rodrigues E, Ramôa F, Quezada D, Shih M, Agustin P, Paes de Almeida O. Calcifying odontogenic cyst: clinicopathological features and immunohistochemical profile of 10 cases. J Oral Pathol Med 2003;32:163-70.
8. López VC, Knezevic MR, Barrero MV, Díaz JM, Báez O, Castellano JJ. Tumor odontogénico de células fantasma (variante intraósea): a propósito de un caso. Med Oral 1998; 3:101-6.
9. Moleri AB, Moreira LC, Carvalho JJ. Comparative morphology of 7 new cases of calcifying odontogenic cyst. J Oral Maxillofac Surg 2002;60:689-96.
10. Johnson A 3rd, Fletcher M, Gold L, Chen SY. Calcifying odontogenic cyst: a clinicopathologic study of 57 cases with immunohistochemical evaluation for cytokeratin. J Oral Maxillofac Surg 1997;55:679-83.
11. Rushton VE, Horner K. Calcifying odontogenic cyst – a characteristic CT finding. Br J of Oral and Maxillofac Surg 1997;35:196-8.
12. Gorlin RJ, Pinborg JJ, Clausen FP, Vickers RA. The calcifying odontogenic cyst – a possible analogue of the cutaneous calcifying epithelioma of malherbe. Oral Surg Oral Med & Oral Path 1962;15:1235-43.
13. Toida M. So – called calcifying odontogenic cyst: review and discussion on the terminology and classification. J Oral Pathol Med 1998;27:49 -52.
14. Zeitoun IM, Dhanrajani PJ, Mosadomi HA. Adenomatoid odontogenic tumor ariding in a calcifying odontogenic cyst. J Oral Maxillofac Surg 1996;54:634-7.
15. Limongelli WA, Anilesh K, Pulse CL, Zegarelli D. Surgical treatment of central epithelial ghost cell tumor. NY State Dent J 1997;63:42-6.
16. Álvarez GS, Jimenez MF, Gómez TFJ, Vecino AFJ, Fernandez SC. Calcifying odontogenic cyst. Associated with complex odontoma: case report and review of the literature. Med Oral Patol Oral Cir Bucal 2005;10:243-7.
![]() Correspondence:
Correspondence:
Dr. Daniel Reyes Court
Dpto. de Cirugía y Traumatología Maxilofacial,
Facultad de Odontología,
Universidad de Chile,
Calle Olivos 943 - Independencia
Santiago de Chile
E –mail: reyescourt@yahoo.es
Received: 12-02-2006
Accepted: 5-11-2006