INTRODUCTION
Pharmacy ethics is a system of moral principles that affects how pharmacists make decisions related to pharmacy practice.1,2,3 Also, it is concerned with what is good for individuals and society as a whole, and has been described as a moral philosophy.1 Pharmacy ethics encompasses a reasonably well-established definition by national and international professional organizations which have largely defined it through codes of ethics.4,5,6,7 A study by Chaar et al. found that it is vitally important to have moral reasoning skills to balance personal values with principles of professional ethics to be able to make ethical and reasonable decisions in pharmacy practice.8
Many countries have well established ethical guidelines like the United Kingdom, Australia and USA, yet little is known about ethics in pharmacy, and what pharmacists find ethically problematic in their work.9,10,11 Having a Pharmacy Code of Ethics in Jordan, is significant in order to guide pharmacists in their relationship with their patients, healthcare professionals and the society.12,13,14 It is important that pharmacists follow the bioethical principles of beneficence, non-maleficence, autonomy and justice, which form the fundamental basis of their role and responsibilities in provision of healthcare.8,13,15 These values provide the basis for an ethical framework, in which awareness of responsibilities can take place.13,15 Other factors also play a role in decision making, including culture and moral reasoning capabilities.
The American Pharmaceutical Association stated that “Pharmacists are healthcare professionals who assist individuals in making the best use of medications. This Code, prepared and supported by pharmacists, is intended to state publicly the principles that form the fundamental basis of the roles and responsibilities of pharmacists. These principles, based on moral obligations and virtues, are established to guide pharmacists in relationships with patients, healthcare professionals, and society”.5 So, when pharmacists allow business objectives to influence and control their conduct, the commitment to these concepts can be compromised.16 For instance, pharmacists face this kind of conflict in a number of ways including: when deciding whether or not to sell over-the-counter treatments that are not needed; when deciding whether or not to recommend less expensive generic medications; or when deciding whether or not to report a colleague that they feel has acted unethically.16,17
With the evolution of the profession, and the increased focus on patient-centered care services, more ethical challenges are expected to arise. In the United Kingdom, Australia and USA for example, pharmacists are encouraged to carry out more services, such as medication management review (MMR), medication therapy management (MTM) or medicine use review.18,19,20,21 Such services are expected to involve more ethical challenges.18 In Jordan, the introduction of the PharmD degree in 2011 in the country, led to more pharmacists working in the hospital sector and delivering higher level of patient care to the community.21 Higher level patient care and interaction is expected to involve higher numbers of ethical dilemmas.21
A study by Cooper et al., conducted in the United Kingdom, noted that there was a wide variation in pharmacists’ ability to identify and describe ethical issues.18 In Croatia, pharmacy ethical practice has developed relatively slowly with research findings demonstrating a need to aid pharmacists in their decision making processes.11 Another study conducted in Iran evaluated pharmacists’ attitude toward the principles of bioethics, emphasizing the need for further research in the area of pharmacy ethics.22 In Saudi Arabia, Al-Arifi investigated community pharmacists’ perceptions and attitudes toward ethical issues and shed light on the need for Saudi health authorities to implement a code of ethics for pharmacy practice.17 This is similar to what is found in the majority of Middle East countries.17,23 In Qatar for example, there is no professional pharmacy association or society that controls, represents or supports the practice of pharmacy.23 This has meant that pharmacists in Qatar have no code of ethics to guide their practice.24
In Jordan, the Pharmacy Code of Ethics, published by the Jordanian Pharmacists Association, consists of a set of principles that pharmacists should adhere to in their practice. It ensures that they act with fairness and equity in the allocation of any health resources made available to patients. It guides pharmacists to maintain priorities of the safety, wellbeing and best interests of those who they provide their services for. This would motivate them to act at all times with integrity in their dealings with patients. In addition, it focuses on the collaborative relationship between pharmacists and other healthcare professionals to ensure that patients, and the public at large, get the best possible care.4 There is a paucity of previous published studies that have explored community pharmacists’ attitudes towards pharmacy practice in Jordan.
Therefore, the aim of this study was to investigate pharmacists’ attitude, needs and barriers towards applying ethical principles published by the Jordanian Pharmacists Association in the Jordanian Pharmacy Code of Ethics. A secondary aim was to identify any differences in attitudes between pharmacists practicing in the busy capital of Jordan, Amman, and in the second largest, less advanced city in north Jordan, Irbid.
METHODS
A cross-sectional, descriptive survey of community pharmacists was conducted in two of the largest cities in Jordan (Amman and Irbid). The selection of these two cities came with the Jordanian Pharmacists Association report stating that the highest number of community pharmacies in Jordan is located mostly in these two distinct geographical areas.4 In addition, it has been reported by the department of statistics in Jordan for the year 2017 that the highest population in Jordan is concentrated in these two cities (Amman followed by Irbid).25 The data were collected between January and August 2017, using a structured self-administered questionnaire. Ethics approval was obtained from the Faculty of Pharmacy, Applied Science Private University Ethics Committee (reference: 2017/2018/1).
A convenience sample of registered community pharmacists located in Amman and Irbid were chosen to participate in the study and respond to the survey. Community pharmacies were visited by a research assistant who explained the purpose of the study and provided the participant information statement. Following the reading of the information statement, verbal consent was sought from the pharmacists before study participation. The information statement contained important information, including the purpose of the study, the fact that participation was voluntary and did not pose any risk to the respondents, that the collected data would be published anonymously, with no indication to respondents’ identity, in addition to whom to contact if any questions were raised. Pharmacists who consented to participate were handed the questionnaire. The completed questionnaires were placed in sealed envelopes by the participants. The questionnaire was followed-up for collection by the researcher on a later date that ranged from one to two weeks. The closed envelopes containing the completed surveys were then delivered to the research team. To avoid social bias, the research assistant did not reveal her own profession to be pharmacy. Returned questionnaires were completed anonymously. Non-respondents were visited to collect their uncompleted questionnaire.
Study tools
The questionnaire was designed and developed following a careful review of the literature and previous studies related to ethics in the community pharmacy setting.11,17,22 Different scenarios were used in previously developed questionnaires regarding ethics in pharmacy, assessing attitude and barriers towards practice. Similar scenarios were used while developing the survey questions in this study. These questions were then pre-tested by pharmacists with experience in ethics research. A draft of the questionnaire was piloted by ten practicing pharmacists to assess readability, understandability, questionnaire design (suitability of the different segments of the questionnaire) and the length of the questionnaire. Based on the result of the pilot study, the questionnaire was modified and the final version was ready to be sent to the selected pharmacies.
The survey questionnaire consisted of a brief introduction of the study followed by forty-two questions. The questions consisted of closed ended, and multiple-choice questions. The questionnaire was constructed to include three sections: the first section collected demographic data of the study participants, including age, gender, education (highest degree), years of experience, number of working hours per week, average number of adult patients who visit the pharmacy per day, and type of pharmacy (polyclinic pharmacy, next to a supermarket/ shopping mall, independent pharmacy or other (specified).
The second section of the questionnaire consisted of several scenarios obtained from the literature review conducted for this study based on pharmacy practice and ethical dilemmas experienced in different countries.11,17,22 Such scenarios were used to evaluate pharmacists’ attitude and practice aspects toward ethical issues using a 5-point Likert scale with responses ranging from 1=strongly agree to 5= strongly disagree, or 1= very highly interested to 5= not interested at all, to assess pharmacists’ agreement with the presented reaction of the pharmacist in each scenario.
The third section was designed to determine the level of ethical practice knowledge of study participants by asking them about whether they had received previous education on ethics in pharmacy practice in Jordan, whether they discussed healthcare issues with their patients, as a part of respect for patient autonomy and promotion of their right to self-determination and recognition of individual self-worth by encouraging them to participate in decisions about their health. Also, this section reported how often, if any, this information was documented in their pharmacy records.
Furthermore, this section investigated barriers that restricted pharmacists from explaining ethical issues to their patients, which ethical information resources were currently available at the pharmacists’ practice sites at the time of the study, resources perceived as important and helpful in caring for the patients, and to whom would participants refer to for advice about their ethical dilemmas once identified.
The Jordanian Pharmacy Code of Ethics was obtained by the research team from the Jordanian Pharmacists Association. The scenarios were formulated according to the stated principles. A revision by an expert in Jordanian pharmacy practice was conducted to ensure that these scenarios represented relevant ethical principles in Jordanian practice.
Sample size
The sample size was calculated based on the current number of pharmacists registered in Amman (11,318) and Irbid (2,051), which were provided by the Jordanian Pharmacists Association. The number of registered pharmacists in both cities was approximately 13,369. The sample size was calculated by the online sample size calculator, using 5% margin of error, 95% confidence level and a response distribution of 50%. The minimum sample size calculated was 372 for Amman and 324 for Irbid.
Data analysis
The data from each of the returned questionnaires were coded and entered into the SPSS version 21 (Chicago, IL, USA), which was used for statistical analysis. Descriptive statistics including percentages, means, and frequency distribution were calculated for each of the questions. Descriptive and univariate correlation analyses, with the Pearson correlation coefficient (r), were used to find correlations at the 5% significance level. A p-value of <0.05 represented a significant difference.
RESULTS
Respondents’ socio-demographic and practice characteristics
A total of 750 questionnaires were distributed to community pharmacies in both Amman and Irbid. Most participants (n=704, Amman n=486; Irbid n=218) consented to participate in the study and completed the survey questionnaire (all questions were answered by all of the participants) giving a response rate of 93.8%. The mean age of the respondents was 30.7 (SD 8.2), with more than half of the respondents being females (Table 1). Significantly, more pharmacists from Amman had PhD and/or Masters Degrees than from Irbid (p<0.001). Pharmacists from Amman had more patients visiting their pharmacies than pharmacists from Irbid (p=0.009), and they had a higher number of pharmacy technicians working at their pharmacies (p=0.005). More respondents from Amman were managers or supervisors, and more of them had their pharmacies located next to a supermarket, a shopping mall or a clinic (p<0.001 for all). A related point to consider is that pharmaceutical care in Jordan is provided to patients regardless of the pharmacist’s position whether the pharmacist in charge was the pharmacy owner, supervisor, or a locum pharmacist.
Table 1. Demographic and other characteristics of the study sample (n= 704), comparing participants from Amman and Irbid
| Amman (n= 486) | Irbid (n=218) | P value | ||
|---|---|---|---|---|
| Age (years); mean (SD) | 30.66 (8.22) | 30.60 (8.6) | 0.9261 | |
| Gender; n (%) | 0.1072 | |||
| Male | 233 (46.2) | 86 (39.6) | ||
| Female | 260 (53.8) | 131(60.4) | ||
| Educational level | <0.0012 | |||
| BSc | 377 (77.6) | 197 (90.8) | ||
| MSc | 57(11.7) | 7 (3.2) | ||
| PhD | 17 (3.5) | 0 (0.0) | ||
| Diploma | 35 (7.2) | 8 (3.7) | ||
| Number of years since pharmacy graduation | 0.8352 | |||
| < 5 | 235 (48.8) | 110 (50.9) | ||
| 5 - 10 | 159 (33.0) | 62 (28.7) | ||
| 11 - 15 | 26 (5.4) | 14 (6.5) | ||
| 16 - 20 | 26 (5.4) | 13 (6.0) | ||
| >20 | 36 (7.5) | 17(17.9) | ||
| Experience as a pharmacist | 0.6982 | |||
| < 5 | 236 (54.1) | 116 (53.7) | ||
| 5 - 10 | 138 (28.4) | 56 (25.9) | ||
| 11 - 15 | 33(6.8) | 13 (6.0) | ||
| 16 - 20 | 23(4.7) | 13(6.0) | ||
| >20 | 29(6.0) | 18(8.3) | ||
| Number of adult patients who visit the pharmacy per day | 0.0092 | |||
| < 50 | 194(40.2) | 62 (28.6) | ||
| 51 - 100 | 206 (42.7) | 116 (53.5) | ||
| >100 | 83(17.2) | 38 (17.5) | ||
| Number of hours worked per week; mean (SD) | 47.08 (13.58) | 45.39(9.16) | 0.1011 | |
| Number of pharmacists who work in the pharmacy at any one shift | 0.1122 | |||
| 0 | 7 (1.4) | 1 (0.5) | ||
| 1 | 261 (53.8) | 103 (47.7) | ||
| >1 | 217 (44.7) | 111(51.4) | ||
| Number of pharmacy technicians who work in the pharmacy at any one shift | 0.0052 | |||
| 0 | 212 (43.9) | 86 (39.8) | ||
| 1 | 191(39.5) | 110 (50.9) | ||
| >1 | 80 (16.6) | 20 (9.3) | ||
| Position | 0.0002 | |||
| Employee pharmacist | 323(66.6) | 176 (81.9) | ||
| Pharmacy manager/supervisor | 86(17.7) | 1 (0.5) | ||
| Pharmacy owner | 75(15.5) | 36 (16.7) | ||
| Pharmacy setting | 0.0002 | |||
| Supermarket or shopping mall pharmacy | 86 (18.9) | 2 (0.9) | ||
| Polyclinic pharmacy | 74 (16.3) | 2 (0.9) | ||
| Independent pharmacy | 291(64.1) | 210 (98.1) | ||
| Have you received any kind of education or training about Jordanian ethical practice in the past? Yes | 318 (66.5) | 185 (86.0) | < 0.0012 | |
| Have you ever been accessed for ethical information at practice site? Yes | 265(56.6) | 52 (24.3) | <0.0012 | |
| How often do you record ethical concerns in your pharmacy? | <0.0012 | |||
| Never | 41 (8.7) | 15 (7.0) | ||
| Rarely | 103 (21.8) | 61 (28.4) | ||
| Sometimes | 171 (36.2) | 104 (48.4) | ||
| Often | 105 (22.2) | 26 (2.1) | ||
| Very often | 52 (11.0) | 7 (3.3) |
1t-independent test;
2Chi-square test
The majority of respondents from Amman (66.5%) and Irbid (86.0%) reported receiving previous education on ethics concerning pharmacy practice services in Jordan (p<0.001). In Amman, more than half (56.6%) of the pharmacists reported that they had access to ethical information resources at their practice site versus 24.3% from Irbid (p<0.001). There was a significant difference (p<0.001) between both cities with regards to pharmacists receiving previous education or training on the Jordanian Code of Ethics, and the frequency of their documentation of ethical concerns (Table 1).
Attitude towards specific ethical scenarios
The frequency of occurrence of specific ethical problems in both Amman and Irbid revealed interesting differences between the two cities (Table 2). In response to the survey scenarios, results showed that in Amman and Irbid, the majority of pharmacists (Amman= 52.0%, Irbid= 84.2%, p< 0.001) disagree/strongly disagree with dispensing a drug if the patient did not really need the treatment. The majority of pharmacists (Amman=63.3%, Irbid=89.8%, p<0.001) would not sell (disagree/strongly disagree) an over-the-counter medication if they suspected any drug abuse by the patient.
Table 2. Assessing pharmacists’ attitude towards specific ethical scenarios from both Amman (n= 486) and Irbid (n=218).
| Statement | Strongly agree | Agree | Neutral | Disagree | Strongly disagree | p-value | |
|---|---|---|---|---|---|---|---|
| 1. A customer asks for an over-the-counter treatment. After talking to the patient you come to the conclusion that s/he does not really need the treatment, but you give him/her the medication. | Amman | 47 (9.7) | 92 (19.0) | 93 (19.3) | 180 (37.3) | 71 (14.7) | 0.000 |
| Irbid | 4 (1.9) | 25 (11.6) | 5 (2.3) | 169 (78.2) | 13 (6.0) | ||
| 2. The prescription states a specific brand of drug. You do not have this in stock but you have a generic clinically equivalent brand in stock. Will you inform the patient before you dispense the generic drug? | Amman | 207(42.8) | 206 (42.6) | 50 (10.3) | 17(3.5) | 4 (0.8) | 0.118 |
| Irbid | 60 (27.8) | 134 (62.0) | 9 (4.2) | 13 (6.0) | 0 (0.0) | ||
| 3. After questioning, a patient makes it known s/he is going to use the medication she/he is asking to buy against guidelines (e.g. hydrocortisone cream for his/her face). Will you dispense the drug? | Amman | 28 (5.8) | 76 (15.8) | 126 (26.1) | 179 (37.1) | 73 (15.1) | 0.012 |
| Irbid | 0(0.0) | 66 (30.6) | 20 (9.3) | 112 (51.9) | 17 (7.9) | ||
| 4. A customer wants to buy an over-the-counter medicine you suspect s/he might be abusing (may be this appears likely after speaking to him/ her about it) and the customer does not want an alternative. Will you dispense the drug? | Amman | 20(4.1) | 65 (13.5) | 92 (19.0) | 163 (33.7) | 143 (29.6) | 0.000 |
| Irbid | 2(0.9) | 14(6.5) | 6 (2.8) | 107 (49.5) | 87 (40.3) | ||
| 5. The husband or wife, or another close family member (other than the parent of a child) of a patient asks for confidential information about that patient’s treatment. Will you tell them? | Amman | 67 (13.9) | 114 (23.6) | 108 (22.4) | 90 (18.6) | 104 (21.5) | 0.000 |
| Irbid | 3 (1.4) | 19 (8.8) | 7 (3.2) | 53 (24.5) | 134 (62.0) | ||
| 6. Someone comes into the pharmacy/phones asking you to identify a particular tablet that does not belong to him/her and you are able to identify the tablet. Will you identify that for the patient? | Amman | 95 (19.8) | 209 (43.5) | 115 (24.0) | 38 (7.9) | 23 (4.8) | 0.000 |
| Irbid | 105 (48.6) | 83 (38.4) | 15 (6.9) | 10 (4.6) | 2 (0.9) | ||
| 7. You believe that withholding the truth from, or deliberately misleading, a patient would mean s/he would be compliant with a treatment you believe is very important to him/her. Are you going to hold the truth? | Amman | 60 (12.6) | 177 (37.2) | 140 (29.4) | 72 (15.1) | 27 (5.7) | 0.287 |
| Irbid | 7 (3.2) | 91 (42.1) | 32 (14.8) | 79 (36.6) | 7 (3.2) | ||
| 8. You feel something a colleague has done is unethical and you talk to your colleague, but still s/he does not change his/her behavior. Will you report this to your manager? | Amman | 131 (27.4) | 205 (42.9) | 98(20.5) | 32 (6.7) | 11 (2.3) | 0.214 |
| Irbid | 47 (21.8) | 118 (54.6) | 11 (5.1) | 35 (16.2) | 5 (2.3) | ||
| 9. A parent of a patient asks for confidential information about his/her son/daughter’s treatment. Will you inform the parents? | Amman | 155 (32.2) | 170 (35.3) | 91 (18.9) | 37 (7.7) | 28 (5.8) | 0.479 |
| Irbid | 29 (13.6) | 122 (57.0) | 25 (11.7) | 35 (16.4) | 3 (1.4) | ||
| 10. A doctor is prescribing, on private scripts, medication you suspect s/he is abusing. You’ve already talked to him/her about it but s/he has clearly ignored you. Will you dispense it? | Amman | 37 (7.7) | 87 (18.1) | 89 (18.5) | 155 (32.2) | 111 (23.1) | 0.000 |
| Irbid | 2 (0.9) | 23 (10.6) | 17 (7.9) | 116 (53.7) | 57 (26.4) | ||
| 11. You suspect a pharmacist you work with is using prescription medicine from the controlled drugs cabinet without a prescription. You already talked to him/her about it but s/he clearly ignored. Will you report this to your manager? | Amman | 144 (29.9) | 173 (36.0) | 101 (21.0) | 41 (8.5) | 21 (4.4) | 0.000 |
| Irbid | 61 (28.2) | 118 (54.6) | 6 (2.8) | 29 (13.4) | 2 (0.9) | ||
| 12. A consultant asks you to dispense a drug for an unreported indication and tells you s/he knows it is used for this indication with great effect in USA. Will you dispense the drug? | Amman | 31 (6.4) | 151 (31.4) | 133 (27.7) | 123 (25.6) | 43 (8.9) | 0.000 |
| Irbid | 64 (29.6) | 104 (48.1) | 26 (12.0) | 21 (9.7) | 1 (0.5) | ||
| 13. A member of the public comes to the pharmacy and asks for some controlled or RX medications or large quantities. Will you dispense it! | Amman | 24 (5.0) | 81 (16.9) | 99 (20.7) | 127 (26.5) | 148 (30.9) | 0.000 |
| Irbid | 0 (0.0) | 10 (4.6) | 8 (3.7) | 43 (19.9) | 155 (71.8) | ||
| 14. A terminally ill patient asks you for a diagnosis or prognosis, telling you s/he does not feel the doctor is telling the whole truth. You know the full case history. Will you tell the patient the truth? | Amman | 78 (16.3) | 145 (30.3) | 125 (26.1) | 77 (16.1) | 54 (11.3) | 0.000 |
| Irbid | 1 (0.5) | 32 (14.8) | 21 (9.7) | 61 (28.2) | 101 (46.8) | ||
| 15. Disclosing to a mother information on contraceptive usage by a daughter | Amman | 53 (11.2) | 99 (21.0) | 152 (32.2) | 112 (23.7) | 56 (11.9) | 0.000 |
| Irbid | 20 (9.3) | 129 (60.0) | 24 (11.2) | 40 (18.6) | 2 (0.9) | ||
| 16. Dispensing natural health products when their efficacy and safety have not been demonstrated by a regulatory authority? | Amman | 22 (4.6) | 79 (16.6) | 106 (22.3) | 155 (32.6) | 113 (23.8) | 0.003 |
| Irbid | 0 (0.0) | 6 (2.8) | 8 (3.7) | 59 (27.6) | 140 (65.4) | ||
| 17. Dispensing sleeping aids (i.e. Xanax® (Alprazolam)) for sleeping disorder without prescription. | Amman | 19 (4.0) | 29 (6.1) | 53 (11.1) | 101 (21.2) | 275 (57.7) | 0.000 |
| Irbid | 0 (0.0) | 7 (3.3) | 1 (0.5) | 18 (8.5) | 186 (87.3) | ||
| 18. Proposing brands instead of generic drugs? | Amman | 52 (10.9) | 152 (31.9) | 174 (36.6) | 78 (16.4) | 19 (4.0) | 0.714 |
| Irbid | 0 (0.0) | 40 (18.9) | 41 (19.3) | 98 (46.2) | 33 (15.6) | ||
| 19. Disclosing side effect of a drug to a patient? | Amman | 68 (14.3) | 165 (34.7) | 130 (27.3) | 77 (16.2) | 36 (7.6) | 0.299 |
| Irbid | 8 (3.7) | 94 (43.7) | 64 (29.8) | 42 (19.5) | 7 (3.3) | ||
| 20. If a child has prescription for serious drug and has the money for paying it, do you dispense it to him? | Amman | 22 (4.6) | 104 (21.8) | 127 (26.6) | 131 (27.5) | 93 (19.5) | 0.000 |
| Irbid | 4 (1.9) | 61 (28.4) | 22 (10.2) | 54 (25.1) | 74 (34.4) | ||
| Very highly Interested | Interested | Neutral | Not interested | Not interested at all | |||
| 21. If you just finished your work and on your way to your home, suddenly a patient called you for a help and advice, you will help the patient. | Amman | 231 (48.2) | 190 (39.7) | 38 (7.9) | 12 (2.5) | 8 (1.7) | 0.000 |
| Irbid | 174 (82.1) | 37 (17.5) | 0 (0.0) | 0 (0.0) | 1 (0.5) | ||
| 22. Call a doctor if you noticed that there is something wrong in the prescription (about the name of drug for his indication or the dose) in front of the patient. | Amman | 231 (48.2) | 171 (35.7) | 55 (11.5) | 14 (2.9) | 8 (1.7) | 0.419 |
| Irbid | 134 (63.2) | 46 (21.7) | 14 (6.6) | 17 (8.0) | 1 (0.5) | ||
| 23. If a patient asked you for a drug that you don’t have now, and he wants it instantly, you refer the patient to another pharmacy that you know that it has this drug. | Amman | 166 (34.7) | 187 (39.1) | 92 (19.2) | 22 (4.6) | 11 (2.3) | 0.000 |
| Irbid | 153 (72.2) | 51 (24.0) | 5 (2.4) | 2 (0.9) | 1 (0.5) | ||
| 24. If a patient asked you to tell him the lethal dose of certain drug, you will give him all the information he/she asked for. | Amman | 112 (23.4) | 78 (16.3) | 99 (20.7) | 84 (17.5) | 106 (22.1) | 0.000 |
| Irbid | 7 (3.3) | 27 (12.7) | 13 (6.1) | 41 (19.3) | 124 (58.5) | ||
Most respondents reported that they would not (disagree /strongly disagree) dispense a controlled drug without a legal prescription, as it is illegal to dispense such drug class without prescription, (Amman=57.4% versus Irbid=91.7%, p<0.001). More pharmacists from Irbid (75.0%, p<0.001) versus Amman (27.4%) would not (disagree /strongly disagree) inform a terminally ill patient if they asked for a diagnosis in case their doctor decided to hide such information. Also, about half (agree /strongly agree) of pharmacists (from both cities) said that they would withhold the truth about medication side effects if that would make the patient more compliant with their medication. As for generic drugs, the majority (agree /strongly agree) from both cities (Amman 85.4% versus Irbid 89.8%) would inform the patient before they dispense a generic drug if the prescription stated a specific brand of medication and it was not found in stock. Most respondents said they would report (agree /strongly agree) to their manager if they perceived their colleague was doing something unethical, after talking to the colleague in question first. (Amman= 70.3%, Irbid= 76.4%).
Most respondents had a negative (disagree /strongly disagree) response towards dispensing a medication to patients if it is against the international guidelines and therapeutics management of a specific condition (Amman=52.2%, Irbid=59.8%). About 78% (agree /strongly agree) of respondents from Irbid would sell a medication for an unreported indication in the guidelines if recommended by the consultant; conversely; only 37.8% of pharmacists from Amman would do the same, showing a significant difference (p<0.05) between the two cities.
Perceived attitudes toward certain practice scenarios
The majority of participants disagreed/strongly disagreed with dispensing natural health products if their efficacy and safety had not been demonstrated by a regulatory authority (Amman 56.4% versus Irbid 93.0%). Community pharmacists in Amman, perceived an ethical dilemma when they were asked about disclosing to a mother, information on contraceptive usage by her daughter. Many pharmacists from Amman (32.2%) agreed/strongly agreed to disclose the information to the mother, while a clear majority from Irbid (69.3%) agreed/strongly agreed to disclose such information. Most of the participants disagreed/strongly disagreed with dispensing sleeping aids (i.e. alprazolam) for sleeping disorders without a prescription (Amman 78.9% versus Irbid 95.8%; Table 2).
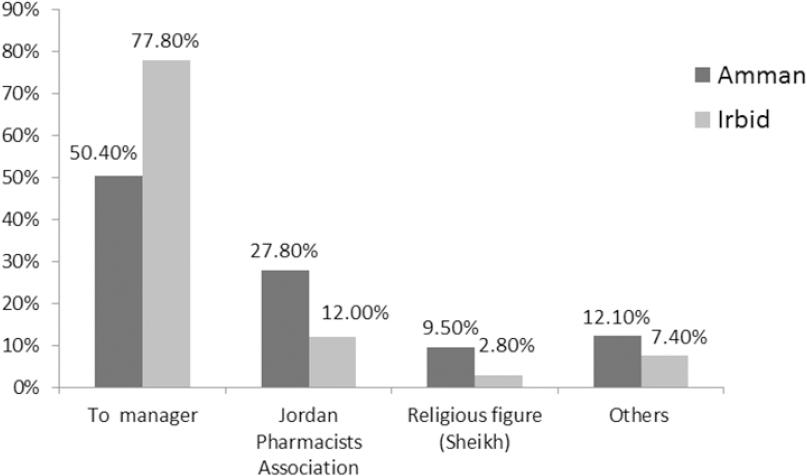
In addition, majority of participants (Amman= 87.9%, Irbid= 99.6%) agreed/strongly agreed to help their patients after their official working shifts, and majority (Amman= 83.9%, Irbid= 84.9%) were interested/ highly interested in calling the patient’s doctor if they noticed that there was something wrong with the prescription. In Irbid, majority of pharmacists (61.8%) disagreed/strongly disagreed with the statement about proposing brands instead of generic drugs, in contrary to only 20.4% of pharmacists from Amman (p=0.714). In Irbid, about 77.8% of pharmacists were not interested in talking about the lethal dose of certain drugs if they suspected abuse by the patients versus only 39.6% in Amman (p< 0.05; Table 2). Pharmacists from both cities stated that they would refer their ethical dilemmas once identified, mostly to their managers, followed by Jordanian Pharmacists Association (Figure 1).
Perceived barriers for discussing ethical issues with patients
Barriers that limited pharmacists from discussing ethical issues with their patients included: lack of time (Amman 43.0%, Irbid 27.0%) and lack of reliable resources (Amman 15.0, Irbid 17.0%). Lack of ethical knowledge (such as lack of knowledge of basic Jordanian ethical standards), lack of skills in making ethical decisions (including the ability to identify the ethical problem), inability to identify the values or legal constraints involved in each scenario and inability to develop options for action were reported as other barriers by the participants preventing them from performing their role in this area (Figure 2).
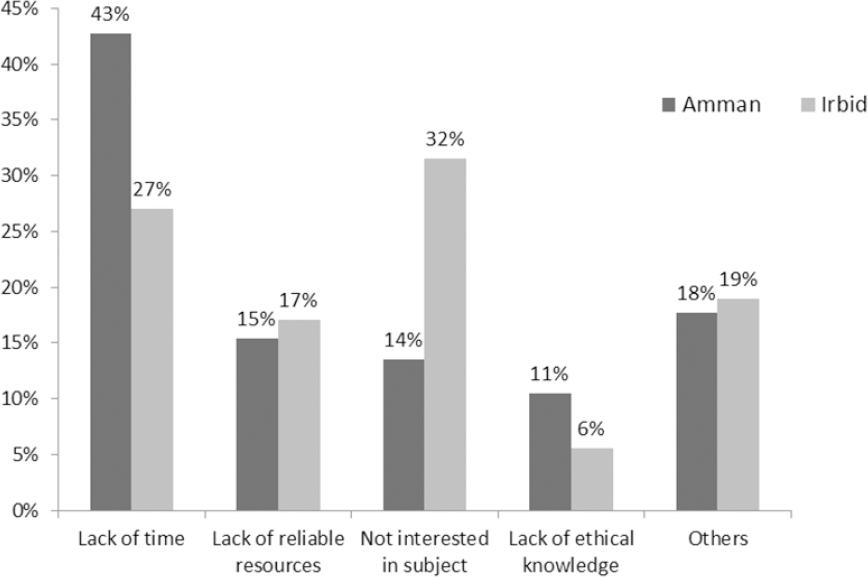
Figure 2. Pharmacists from Amman (n=486) and Irbid (n=218) reported barriers that limited their interaction with their patients regarding ethical dilemmas
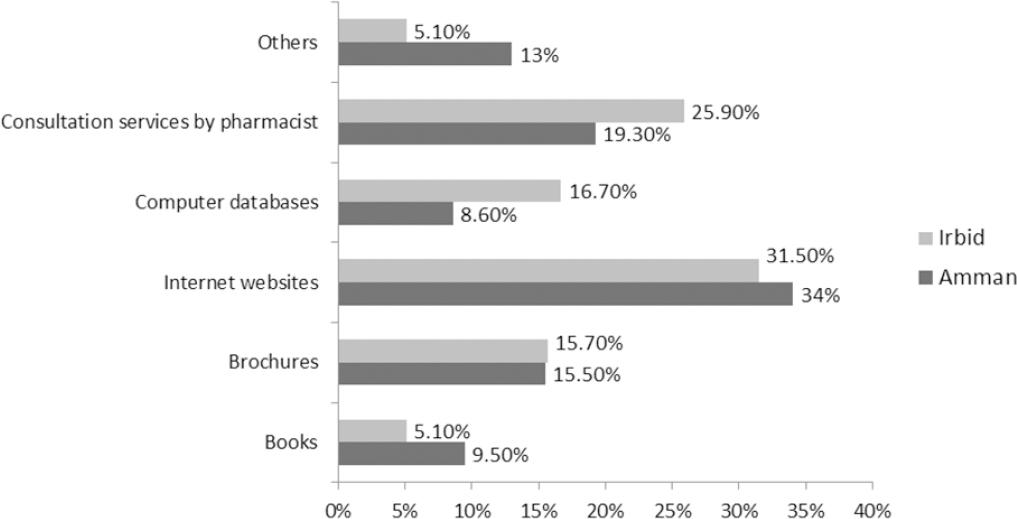
Pharmacists reported that they mostly use the Internet as a resource to help them in resolving ethical issues concerning their patients (Amman 43.0% vs. Irbid 31.5%). This was followed by discussions with their peers and other health care professionals about the ethical issue (Amman 19.3% vs. Irbid 25.9%). Brochures designed by the Jordanian Pharmacists Association discussing ethical principles were also mentioned (Amman 15.5%, Irbid 15.7%). Few pharmacists referred back to written materials and books (Amman 9.5%, Irbid 5.1%; Figure 3).
DISCUSSION
To our knowledge, this is the first study conducted in Jordan to explore community pharmacists’ attitude in relation to ethical pharmacy practice in the country. The study investigated pharmacists’ attitudes towards applying the major ethical principles published by the Jordanian Pharmacists Association in the Jordanian Code of Ethics, including: beneficence, maleficence, autonomy and justice. With the influx of the Syrian refugees into Jordan, and the presence of high numbers of people from surrounding countries, a culture of diverse populations exists in Jordan.17,26 The existence of a healthcare system based on a set of pre-identified and approved ethical principles is needed to address the different ethical issues arising.
Based on the pharmacy literature, five decision-making approaches are identified, including clinical, managerial, ethical, economical, and legal problem-solving approaches.27,28 In an ethical decision-making approach, the main focus is achieving a morally defensible solution to the problem.8,28 Using an economic decision-making approach, the goal is to maximize the cost-effectiveness with a solution that is most profitable or least costly, depending on the situation.13,28 The legal approach to decision-making is straightforward, and simply involves taking actions that are deemed to be acceptable under the law.13 Each approach uses a similar general process consisting of: identifying the problem and defining it, suggesting solutions, making a choice, and assessing the results of the choice.28 The general process of the abovementioned methods differ in two main aspects: first, in how the problem is framed, and second, in the intended outcome of the decision.27,28 In this study, a bioethical approach was the main ethical foundation used to understand the reasoning and behavior of Jordanian pharmacists; although it is important to acknowledge that in practice, all decision-making approaches may often overlap to determine a final decision.28 29-30
The scenarios used in this study were formulated according to established Code of Ethics. For example, the scenario about “proposing brands instead of generic drugs”, represented the principle of respect for a patient’s autonomy to select either of the drugs after informing patients of the available alternatives. The study revealed that not all pharmacists know enough about the Jordanian Code of Ethics. This was proven by the finding that only 66% of the study sample in Amman and 86% from Irbid self-reported having received education or training about Jordanian ethical practice in the past. The pharmacists did not follow the Code of Ethics when identifying resolutions for the ethical issues they faced during their work.
Results of this study are interesting and unique as they also compare the two biggest cities in Jordan, Amman- the most populated and busy capital, and Irbid, a representative of another large, less advanced city in the country. Results based on these two most populated cities in the country pave the way for policy makers to take the measures needed for community pharmacists to gain the best possible benefits from the Code of Ethics that exists in the country.
Interestingly for example, more pharmacists from Irbid (77.7%) declared that they would sell a medication for an unreported indication in the guidelines, if recommended by the consultant, compared to Amman (37.8%). Pharmacists from both cities reported a similar ‘approving’ attitude toward dispensing a generic drug if the prescription stated a specific brand name and it was out of stock. The availability of multinational products on the Jordanian medicine market, including international and national products, play a role here. As a result, this may lead to a number of ethical concerns. A study by Al-Arifi found that 31.0% of pharmacists would dispense a clinically equivalent medication when the pharmacy was out of stock of the brand stated in the prescription; comparable to 29.0% in another local study.17,26
Pharmacists’ resources for information on ethics are important. More pharmacists from Amman reported having access to ethical information resources at their practice site compared to Irbid. Many pharmacists from both cities used the Internet as their source of ethical information when needed to help in dealing with their patients. The Jordanian Pharmacists Association has the ‘Good Pharmacy Practice’ booklet on its website, which contains some useful information on the topic. Anecdotal comments indicated that, this was unknown to many of the pharmacists. The Jordanian Ministry of Health has the ‘pharmacy laws and regulations’ published on its website. Other Internet resources contain international code of ethics. Pharmacists checked these websites looking for laws and regulations in order to decide on how they can deal with ethical dilemmas.
Pharmacists indicated that discussions with their peers and healthcare professionals was a useful resource they referred to, for resolving different ethical dilemmas, indicating positive shared decision making in the pharmacist-patient-doctor confidential therapeutic relationship. The least used resource was books about ethics in pharmacy. In the Al-Arifi study, it was also found that using books about ethics (37.7%) followed by Internet websites (31.1%) and brochures (26.8%), were the major resources used.
It is clear that accessibility of resources on ethics is an issue in Jordan, which is to be expected in a country with a pharmaceutical care system still under development. Providing pharmacists with reliable resources on ethics, and training them on how to use them is vital. Education on pharmacy ethics is not limited to the provision of theory about ethics, but also on training the pharmacists on where to find such information, and how to apply it, to make a suitable decision before making a recommendation and providing information to their patients.11,17,31
An updated code of ethics in the country is essential.17 The current code of ethics in Jordan was established in 2008 by the Jordanian Pharmacists Association, to guide community pharmacists to deal with their patients and other healthcare professionals following good pharmacy practice.4 These standards were set to achieve the ethical and professional practice needed to positively reflect the professional image of the role of the pharmacist to patients and society at large.4 It is important to note that these standards were not published on a large scale to be acknowledged by all pharmacists in the country. The Jordanian Pharmacists Association is the responsible body in the domain of pharmaceutical ethics, and hence should take the lead in this area. Having a well prepared, contemporary pharmacy code of ethics would support and protect healthcare professionals, and enhance the status of the profession and the healthcare system as a whole.32 The existing code of ethics needs not only to be published broadly, but to be highlighted to the pharmacists through workshops conducted on the national level. Anecdotal comments from the participants indicated that such workshops would be helpful for them to learn about the different and most important ethical issues happening in the country, as lack of familiarity with the topic hinders their ability to easily specify such issues.
Pharmacy schools in the country have a role in this area as well. Courses on ethics with extensive focus on ‘ethical dilemmas’ identified in the country need to be introduced into the pharmacy curricula at the university undergraduate level.24,33 Continuous professional development and educational programs would also be valuable.17,31,34 In addition, a large scale study involving Jordanian pharmacists and the public is needed to assess pharmacist’s familiarity and adherence to the Code of Ethics.
Findings from this study were similar to others with regards to the high number of pharmacists dispensing a doctor-prescribed drug in cases where the patient did not really need it. Other studies, including Al-Arifi, and Deans et al., reported similar findings.17,26 In Saudi Arabia, around 43.0% of pharmacists admitted to selling an over-the-counter medication to a patient who does not really need it.17 In the European countries, a lower proportion was reported; ranging from 13.0% in the UK to 17.7% in Croatia.11,26 In a developing country, where making a living is not so easy for pharmacists, selling over-the-counter drug in the case where it is not really needed, or dispensing an alternative brand medication to a prescribed drug, is appealing. However, despite the influence of financial gain and economic burden, there should be a desire to respect the autonomy of the patient.17
Implementation of the local code of ethics and professional conduct is desired in all healthcare sectors, and in all of the cities in all countries.35 However, differences in perceptions of pharmacy practice were found between the Jordanian cities in this study. Participants perceived an ethical dilemma when they were asked about disclosing to a mother information on contraceptive usage by a daughter. Such results were not surprising considering previous findings from Saudi Arabia, where the majority of the study respondents (69.2%) agreed to supply and disclose information regarding hormonal contraception when presented with a similar scenario.17 In the United Kingdom, the situation was different, as only 21.0% of pharmacists agreed to supply/disclose information about hormonal contraception use.36 Cultural and religion background differences may affect ethical decision making by pharmacists influencing their decision over whether or not to disclose information regarding hormonal contraception. Such differences between the countries are expected, but what was surprising in the findings reported in this study, the differences noted between the cities of the one country. Such outcomes deserve further investigation in future research.
Our findings highlighted a gap between actual professional practice and what pharmacists perceived as their ethical responsibilities. A set of barriers that limited pharmacists from discussing ethical issues with their patients was revealed for the first time. The reported barriers were similar across both cities, Amman and Irbid. Lack of time, lack of reliable resources, and lack of ethical knowledge were the most commonly identified barriers. These findings were consistent with the findings of previous studies.8,14,28
Study limitations included pharmacists answering to some of the scenarios presented in the questionnaire in such a way to show that they have high ethical and moral standards. In addition, using closed ended questions in the questionnaire could have implied that ethics in Jordan is about applying principles rather than about shared decision making in the pharmacist-patient-doctor confidential therapeutic relationship. Future studies can benefit from incorporating open-ended questions regarding shared decision making in ethics. This study assessed the attitude/perception toward certain scenarios but did not assess real practice and whether the pharmacists utilized the decision- making process following the principals of professional ethics found in the country. Another limitation is the absence of a direct question regarding the existence of the current Code of Ethics in the country and familiarity of the participants with it. Future studies should focus on assessing pharmacists’ familiarity and compliance with the code of ethics set in the country.
CONCLUSIONS
Majority of participating pharmacists in Jordan reported receiving previous education on ethics concerning pharmacy practice. More pharmacists from Amman than Irbid have access to ethical information resources at their practice site. Important differences in attitude between pharmacists in Amman and Irbid were found, as, for example, more pharmacists from Amman agreed with dispensing a drug if the patient did not really need it compared to Irbid. The same finding was reported with selling an over-the-counter medication in the case of suspicion of drug abuse by the patient and with dispensing natural health products when their efficacy and safety have not been demonstrated by a regulatory authority.
Certain barriers that limited pharmacists from discussing ethical issues with their patients were identified. Lack of time and reliable resources were amongst the most important barriers identified. Jordanian Pharmacist Association should take the lead in conducting workshops to educate pharmacists from all cities in Jordan on the existing Code of Ethics and help them overcome the existing barriers. Results of this study are important and call onto the authorities and policy makers in the country to widely distribute the current pharmaceutical code of ethics and support its integration into the pharmacists’ day to day practice.