INTRODUCTION
Patients admitted to hospital undergo various investigations, procedures and prescribed medications to manage their medical conditions. Prescribing medications during admission require initiating medication(s) for the current medical condition(s) as well as continuing patients’ pre-existing medications for any underlying medical conditions. In some cases, the patients’ pre-existing medications, could be the reason for admission and discontinuation or dosing adjustment of the offending medications may be required. A formal process to obtain an accurate and complete list of medications that patient was previously taking (including prescription medications, over-the-counter, supplements and herbal preparations) is defined as admission medication reconciliation.1 Information is obtained through various sources: patient, caregiver, hospital records, health-care providers and community pharmacists.
During discharge, an accurate patients’ discharge medication list is prepared based on comparison of admission medication reconciliation list, medications prescribed in the ward, and medications planned at discharge with the agreement of physicians, patients and caregivers. These changes have to be documented and communicated to patients or caregivers. These processes are collectively defined as discharge medication reconciliation.1
Medication reconciliation is a highly complex and time-consuming process, demanding significant skills. The American Society of Health-System Pharmacists (ASHP) recommends pharmacists who are uniquely qualified, to lead, establish and maintain effective medication reconciliation processes in hospitals.2 In additional, pharmacists are able to communicate with community pharmacist counterparts to obtain and relay relevant medication details.3
Medication reconciliation lists are used to compare with discharge prescription orders either in same health-care facilities, primary care physicians or community pharmacies; and any inconsistencies between both lists are identified as medication discrepancies. Discrepancies that are without any clinical rationale or without the attending physicians consciously altering the therapy are defined as unintentional discrepancies; which are categorized as medication errors.4,5 Such medication errors among adult patients discharged from the general medical wards ranged from 23% to 70%.6 7 8 9 10 11 12 13-14 The most common medication error at discharge was found to be unintentional omission of medications.10,11,13 Medication review during patient’s home visit by pharmacists within 2 week of hospital discharge revealed variety of medication issues such as untreated indication, improper doses and medications with no indication.15 It has been reported that unintentional medication changes or unintentional medication omission that are not correct during discharge contributed readmission in adult patients.16,17. Unintentional omission of insulin human isophane during discharge caused patient’s blood sugar rise to 517 mg/dL and vomiting at nursing home which resolved after restarting insulin therapy.13 Unintentional increase of clonazepam dose; caused lethargy in patient and subsequently fall at nursing home.13
Hence, the aim of this study was to modulate interventions to reduce percentage of patients with one or more medication errors during discharge.
METHODS
Study design and setting
We conducted a prospective, quasi-experimental, pre-post intervention study to evaluate the effectiveness of a pharmacist-led quality improvement (QI) program for reducing medication errors during hospital discharge.
This study was conducted in nine adult general medical wards at a 990-bedded tertiary care public hospital in Ipoh, Malaysia. These wards have a total of 276 beds with multiple medical specialities such as cardiology, nephrology, neurology, haematology, endocrinology and pulmonology.
Prior to the study, each medical ward has one ward pharmacist assigned to work during office hours (8.00 am to 5.00 pm) on weekdays. The ward pharmacists’ core responsibilities are to perform medication reconciliation at admission, review medication therapy, prevent medication errors and participate in clinical ward rounds. During daily medication review, all medications prescribed in ward are reviewed for correct doses, formulations, route of administrations, indications, contraindications, compatibilities, side-effects, interactions, efficacy, monitoring, adherence issues and evidence-based treatment. Medication-related issues identified as mentioned above are discussed with attending physicians during ward rounds to optimize medication therapy based on an individual patient’s condition. Ward pharmacists perform discharge medication reconciliation during discharge; comparing admission medication reconciliation lists, ward medications are compared and discharge plans. Patient-related issues (adherence, social support, preferences etc.) are identified. Attending physicians are consulted and the discharge medication reconciliation list is obtained. Bedside discharge medication counselling is done to communicate medication changes and other medication-related information.
Discharge prescription are ordered by house officers (qualified doctor practising under supervision after first year of graduation) through electronic ordering system. If discharge prescriptions are ordered after officer hours, patients collected their medications from the hospital outpatient pharmacy.
Medication error detection
Discharge medication reconciliation list is compared with prescription order by ward pharmacist either on the same day of patient discharge (prescription ordered within office hours) or the following morning (prescription ordered after office hours). Any discrepancies detected by ward pharmacist are discussed with the attending physician in the ward and decided if the discrepancies are intended or unintended.5 Unintended discrepancies are recorded by ward pharmacist as medication error in the data collection sheet provided. Medication errors that are detected the following morning by ward pharmacist are non-intercepted medication. Non-intercepted errors are errors that reached patient.18 Type of medication errors (wrong dosing, wrong drug, unintentional omission or addition of medication) for this study are adapted based on work by Pippins et al. (2008) and classified as shown in Online appendix 1. Although the research pharmacist retrieved information on the prescription medications, over-the-counter medications as well as supplements and herbal preparations, this study only focused on prescription medicines only for the purpose of medication error identification.
All prescribing errors detected were reviewed for clinical significance by two senior pharmacists and a medical specialist independently. Errors were categorized into two categories: clinically significant or non-clinically significant. Clinically significant errors are errors that would cause detrimental effect to patients’ health, treatment delay and ineffective treatment if not detected and corrected before reaching patients (Code E – I). The coding are based on National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP).19 Any differences in coding were discussed and a consensus agreement was reached among the three reviewers.
Improvement team
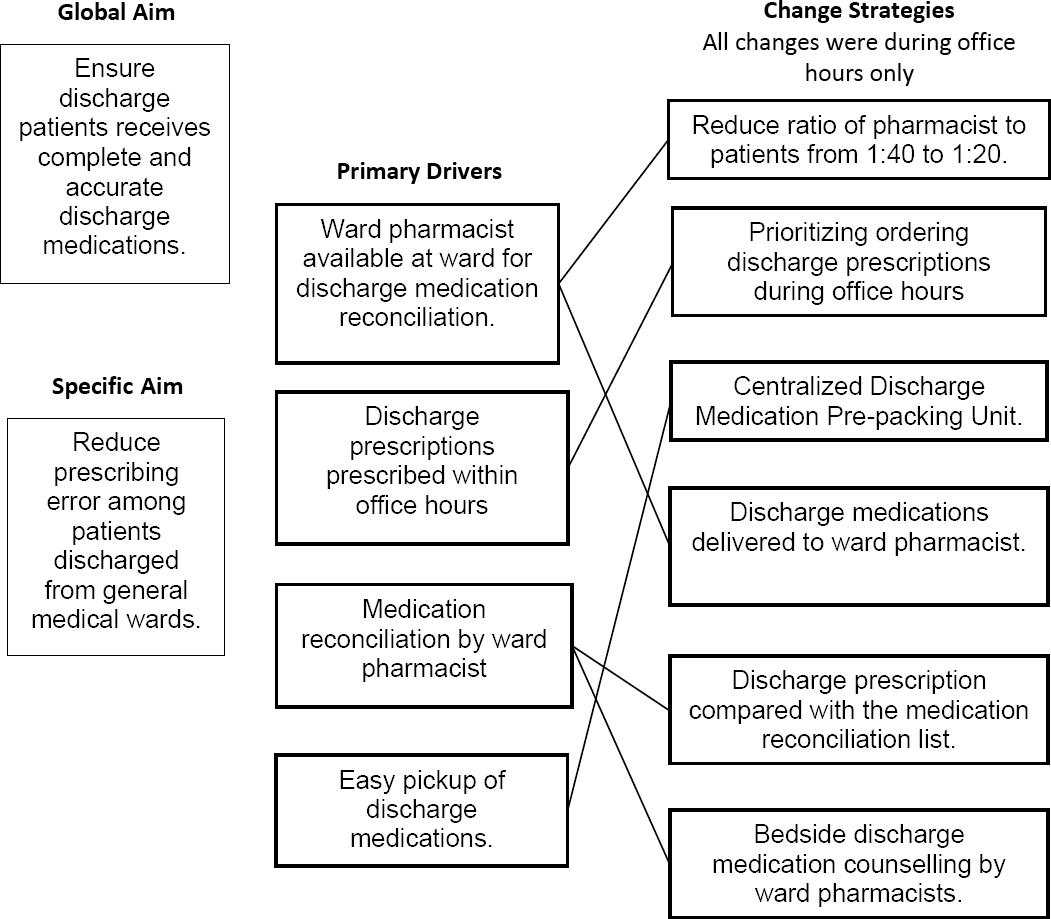
The pharmacy department initiated this QI program. The improvement team consisted of the manager of medical department, manager of the pharmacy department, physicians and pharmacists. A key driver diagram was developed as depicted in Figure 1.
Phase 1: Pre-Intervention
This study was conducted over a period of 9 months in three phases. In the first phase, pre-intervention data on prescribing errors during hospital discharge were collected on 4 consecutive weekdays (Mondays to Thursdays) on selected weeks in each month over a 3-months period (July, August and September 2017) as decided by the researchers. We selected the study points of 4 consecutive weekdays for data collection based on availability of all nine-ward pharmacists and no presence of public holidays in the selected week.
Discharge prescriptions from medical wards that are received by ward pharmacists or outpatient pharmacists by 10 pm weekdays were printed and collected for the purpose of this study. Discharge prescriptions which were not collected on the same date of prescriptions order date were excluded.
Discharge pres criptions after office hours are screened by outpatient pharmacists in the routine manner for correct dosing regime based on standard dosing references. Errors detected are corrected subsequently either by the prescribers, or by the pharmacists, who would have contacted the prescribers (adhering to standard protocol), in the electronic ordering system. Errors detected were highlighted using red ink ball pen on printed prescriptions.
Discharge prescriptions during office hours and after hours are compared with the discharge reconciliation medication list by ward pharmacists. If the ward pharmacists detected any unintentional discrepancies, it was discussed with the attending physician in the ward. Unintentional discrepancies are recorded as medication errors. Unintentional discrepancies in discharge prescription after office hours are recorded as non-intercepted errors; hence patients are contacted to provide correct medications and prescriptions. All medication errors detected are corrected in the electronic ordering system by ward pharmacists.
All nine ward pharmacists that are involved in data collection had at least a minimum of 3 years of working experience in the medical wards.
An instructive letter from the Chief Pharmacist was issued to the ward pharmacists and outpatient pharmacists during each point of study as a reminder to collect discharge prescriptions as proposed above. All pharmacists involved in the data collection were briefed for a maximum of 30 minutes per session before each point of data collection.
Phase 2: Quality Improvement
Phase 2, the intervention phase was conducted over three-months (October to December 2017) and no data was collected during this phase. Pre-intervention data of medication errors at discharge were presented to managers of both the pharmacy and medical department. Subsequently, the following improvement measures were implemented:
The number of ward pharmacists was increased in all medical wards from one to two to accommodate a ratio of pharmacist to patients of 1 to 15-20.
House officers were instructed to prioritize ordering discharge prescriptions within office hours in order for the ward pharmacists to complete discharge medication reconciliation process.
Ward pharmacists performed discharge medication reconciliation (compared all prescriptions ordered by house officers against the discharge medication reconciliation list) and provide bedside discharge medication counselling. In the past, this was an ad hoc activity where only about 5-10% of the ward pharmacists’ total working time per day was allocated for this activity. As a quality improvement strategy, this was emphasized as part of the ward pharmacists’ routine responsibilities.
A Centralized Discharge Medication Pre-packing Unit was set up to facilitate packing of discharge medication to enable ward pharmacists to provide bedside dispensing and medication counselling. In the past, respective ward pharmacists had to leave the ward to return to the pharmacy to pack discharge medications. In this study, staffs at the Centralized Discharge Medication Pre-packing Unit packed the discharge medication based on discharge prescriptions ordered in the system and delivered to the wards where the QI program was implemented.
Phase 3: Post-Intervention
In phase 3, similar to the pre-intervention data collection, post-intervention data collection was done for another 3 months (January to March 2018). Outpatient pharmacists on duty were briefed before each point of data collection. The same nine designated ward pharmacists in the pre-intervention data collection were involved in the data collection process in the wards.
Study outcomes
The primary outcomes of the study were the percentage of discharged patients with: 1) medication error, 2) clinically significant medication error, and 3) non-intercepted medication error. The denominator for the primary outcomes was the total number of patients that were discharged from the nine medical wards as shown in the Equation 1-3.
Equation 1: Percentage of patients discharged with medication errors
Equation 2: Percentage of patients discharged with clinically significant medication errors
Equation 3: Percentage of patients discharged with non-intercepted medication errors
The sampling size was calculated by setting a power of 90% and significance level of 5% for independent cases using PS Power and Sample Size Calculation Version 3.0. Baseline error was assumed at a rate of 40% based on a pilot study conducted in this hospital for a month prior this study. Assuming that with a 15% decrease in discharge prescription error post-intervention, given various interventions in literature resulted in 20 – 40% of absolute reduction in rates of error in discharge prescriptions, a total of 203 prescriptions were required in each pre and post-intervention phase.20-22
Statistical analysis
The data collected at the end of each week was entered into Stata V.13 Statistical Software for analysis. Categorical data were presented as frequency with percentages, while continuous data were summarized as means with standard deviations (SD) if approximately normally distributed, or median and interquartile ranges (IQR) otherwise.
The statistical process control (SPC) chart was employed to illustrate the impact of the QI program on the primary outcomes.23 24 25-26 This method of evaluating the effectiveness of interventions to reduce prescribing errors in the primary care settings provided valuable information to managers for decision-making.27 The p-chart (p stands for percentage) was chosen to chart the percentage of patients with prescribing error as the outcome measures were binary (error versus no error) and the number of discharged patients (sample size) at each point was not constant. To enable the comparison of primary outcome measures between pre- and post-intervention phases, we calculated the mean percentage error for each phase using the total number of patients with error prescriptions and as the nominators and total discharge patients as the denominators. The upper control limit (UCL) and lower control limit (LCL) denoted the boundaries within which 99% of the data points will be found when the limits are set at a distance of 3 sigma [3 SDs] from the mean. Changes in the mean process error between phases were evaluated using the Chi-square test. Data with two-sided p-value of less than 0.05 (p<0.05) was considered statistically significant.
Ethical considerations
The study was registered with the National Medical Research Registry (NMRR) [NMRR-17-1628-36539] and code of ethics approval was obtained from Medical Research and Ethic Committee (MREC).
Attending physicians were notified of non-intercepted prescribing errors. The ward pharmacist and attending physician discuss each of these prescribing errors. Patients are contacted to provide correct medications and prescriptions. Decision was made not to contact patient by attending physician when error did not pose any harm to patient. Examples of such errors was oral prednisolone was prescribed 4 days instead of 3 days for a patient with acute exacerbation of asthma. In another error, inhaler beclomethasone was omitted from prescription order but the device was already supplied to patients during device counselling in hospital and furthermore patient has a doctor’s follow-up appointment in two weeks. All non-intercepted errors were corrected in the electronic system. One researcher followed-up with ward pharmacists regarding decision made regarding all non-intercepted errors. The prescriptions collected were labelled according to their prescription dates and stored with rest of the prescriptions received by the pharmacy for 2 years, based on instructions from the Ministry of Health Malaysia (Ref: ANM.600- 1/24/4/8 dated 3rd October 2012). Stata database and excel spreadsheets did not include any unique identifiable details for the involved patients or prescribers.
Table 1. Characteristics of patients, prescribers, and prescriptions during the study
| Characteristics | Pre-Intervention Phase | Post-Intervention Phase | p-value |
|---|---|---|---|
| Total patients, n | 505 | 482 | |
| Gender of patients, n (%) | 0.3 | ||
| Male | 294 (58.2) | 264 (54.8) | |
| Female | 211 (41.8) | 218 (45.2) | |
| Age of patients (in years), mean (SD) | 59.9 (16.2) | 58.9 (17.6) | 0.4 |
| Diagnosis on Prescription, n (%) | |||
| Cardiovascular Diseases | 176 (34.9) | 146 (30.2) | |
| Infection | 44 (8.7) | 41 (8.5) | |
| Renal Diseases | 41 (8.1) | 39 (8.1) | |
| Lung Infections | 37 (7.3) | 44 (9.1) | |
| Stroke | 30 (5.9) | 25 (5.2) | |
| Acute Exacerbations of BA or COPD | 23 (4.6) | 17 (3.5) | |
| Diabetes Related Admissions | 22 (4.4) | 30 (6.2) | |
| Blood Disorders | 22 (4.4) | 19 (3.9) | |
| Seizures | 17 (3.4) | 23 (4.8) | |
| Cancers | 10 (2.0) | 11 (2.3) | |
| Liver Diseases | 10 (2.0) | 9 (1.9) | |
| Electrolyte Imbalances | 9 (1.8) | 13 (2.7) | |
| Adverse Drug Events | 7 (1.4) | 5 (1.0) | |
| Others | 5 (1.0) | 8 (1.7) | |
| Unclear | 46 (9.1) | 24 (5.0) | |
| Missing | 6 (1.2) | 28 (5.8) | |
| Prescriber category, n (%) | |||
| House Officer | 465 (92.1%) | 440 (91.3%) | 0.6 |
| Medical Officer | 40 (7.9%) | 42 (8.7%) | |
| No. of medications, mean (SD) | 6.5 (3.2) | 6.6 (3.5) | 0.5 |
| Duration of prescription, n (%) | 0.8 | ||
| One month or more | 423 (83.8) | 406 (84.2) | |
| Less than a month | 82 (16.2) | 76 (15.8) | |
| Time of prescription order (%) | < 0.001 | ||
| Office hours | 214 (42.4) | 382 (79.3) | |
| After officer hours | 291 (57.6) | 100 (20.7) |
SD - standard deviation, BA – bronchial asthma, COPD – chronic obstructive pulmonary disease
RESULTS
During the study period, 1014 patients were discharged from nine general medical wards. Of these, 27 patients were excluded as their discharge medications were not collected on the day of discharge. Therefore, 987 patients were included in the final analysis with 505 patients in the pre-intervention phase and 482 patients in the post-intervention phase. The characteristics of patients, prescribers, and prescriptions during the study period are summarised in Table 1. All characteristics were similar in both phases, except for the percentage of discharge prescriptions that were ordered during office hours, which increased as a result of implementing the second component of the QI program.
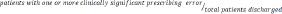
Figure 2 illustrates the impact of the QI program on percentage of patients with medication errors during hospital discharge. Study phases were directly annotated onto charts. On average, the percentage of patients with one or more errors was 32.2%, but could be as high as 42.7% or as low as 20.0%, which represented the variation found in errors from discharge prescriptions (Figure 3A). During the entire six months study period, only common variations were observed and therefore, the process was considered stable and predictable. The process remained under similar conditions after the implementation of the QI program for a period of three months. The mean percentage of error during the pre-intervention and post-intervention phases were not dissimilar (29.7% vs. 34.9%, p=0.08). Same patterns were observed in the percentage of patients with one or more clinically significant errors (Figure 3B). The process was stable and predictable, exhibiting only common cause variation, where an average 24.8% of patients experienced clinically significant errors (ranged between 15.2% and 34.4%). The mean percentage of patients with clinically significant errors during the pre-intervention and post-intervention phases were similar (23.8% vs. 25.9%, p=0.40). Figure 2C illustrates the percentage of patients with one or more non-intercepted errors. The baseline reflects common cause variation with a process mean of 22.4%. The team began implementing the QI program at the end of the pre-intervention phase of three months; during which no data were collected Subsequently, the plotted data for the post-intervention phase after implementation of the QI program strongly suggested that the percentage of patients with one or more non-intercepted errors progressed in a positive downward manner, culminating in a special cause (8 consecutive points below the baseline process mean). This special cause reflected the introduction of the QI program into a process in transition, resulting in a reduction in the mean percentage of non-intercepted errors from 22.4% to 4.1% (p<0.001), and tighter control limits (indicating less variation in the process).
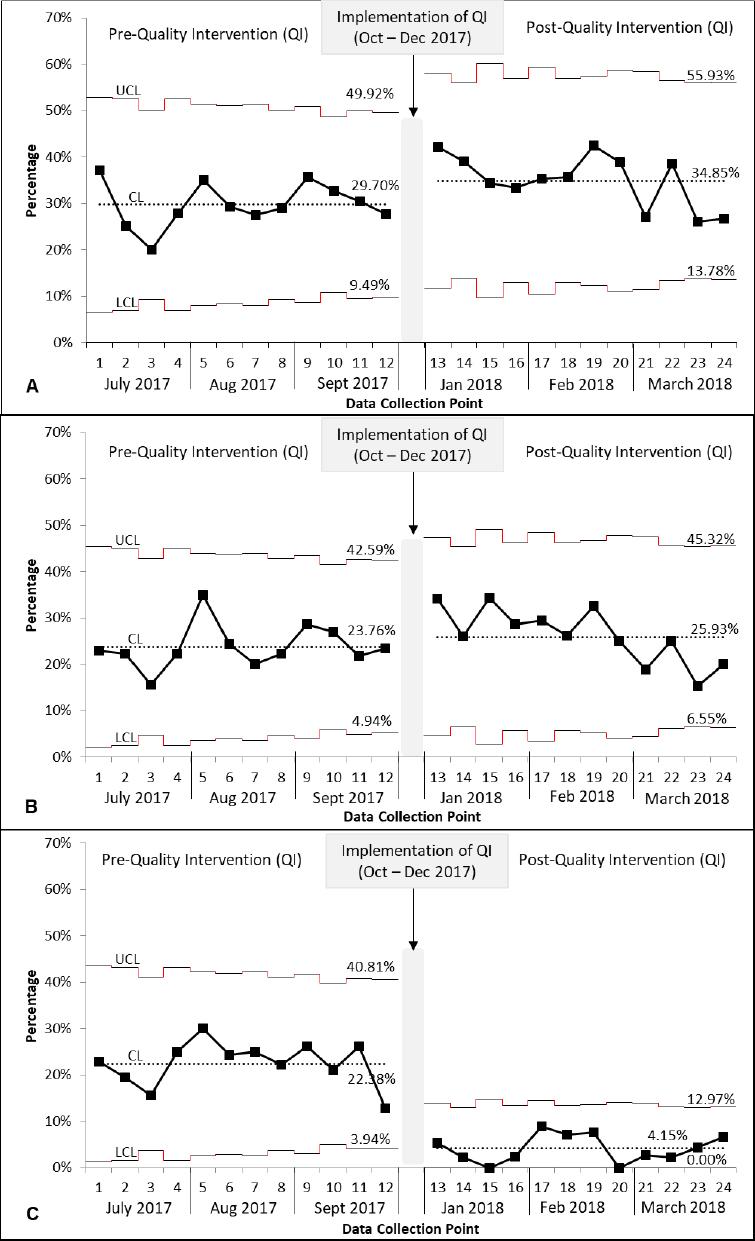
Figure 2. p-chart illustrating serial percentages in pre-intervention phase (July to September 2017) and post-intervention phase (January to March 2018) of patients discharged with one or more medication errors (A), clinicall significant medication errors (B) and non-intercepted medication errors (C).
Patients had a median of 7 (interquartile range, IQR 4, 9) medications in their discharge prescriptions. Total medications prescribed in the pre-intervention was 3264 and in post-intervention was 3192. Extend of error per patient ranged from 1 to 6. With the implementation of QI program, total non-intercepted errors reduced significantly from 176 (5.4%) to 28 (0.9%) (p<0.001). Most of discrepancies detected, 99.6% (512/514), by ward pharmacists was accepted by the attending physicians as unintentional discrepancies and as medication errors. Eight of the errors were not corrected in the electronic ordering system as errors was considered not clinically significant by attending physicians and all of it involved wrong duration of medications. Some examples of clinically significant medication errors were summarized in Online appendix 2.
Types of errors are summarized in Table 2. In both pre-intervention and post-intervention phase, the most common type of errors was omission of medication, wrong dose and wrong frequencies. All types of errors were similar in both phases but wrong duration significantly increased after the introduction of the QI program.
The common medication classes that were omitted were medications classified under the cardiovascular system, 57 errors (36%) followed by the alimentary tract and metabolism, 42 errors (27%) and blood and blood forming organ, 20 errors (13%). Medications that was most often omitted were sublingual glycerine trinitrate (in 15 prescriptions), atorvastatin (in 11 prescriptions), and clopidogrel (in 8 prescriptions) while various types of insulins, calcium carbonate and pantoprazole were omitted each in 7 prescriptions. Medication classes that were most often involved in other than omission of medications were alimentary tract and metabolism, and cardiovascular systems, involving 104 errors (29%), and 86 errors (24%) respectively. Various types of insulins 23 errors (6%), frusemide 21 errors (6%), acetylsalicylic acid 19 errors (5%), metformin errors (5%) and calcium carbonate 12 errors (3%) topped the list of medications of other than omission errors. A complete list of medications according to class and medications involved in the discharge prescribing errors, were sub-categorised as shown in Online appendix 3 and Online appendix 4 respectively.
DISCUSSION
The intervention program successfully attained high percentage of patients with medication errors that was intercepted and corrected at discharge. The major component of this QI program was the complete reconciliation of medications at admission to discharge including bedside discharge medication counseling by ward pharmacists. In various studies; pharmacists play an important role in medication error reduction through discharge medication reconciliation.28-35 A recent randomized control trial which included pharmacists to completed the medication management plan in the medical discharge summaries, reduced at least one medication error by an absolute risk reduction of 47%.20
Table 2. Discharge Prescribing Errors by Sub–category Pre and Post-Quality Improvement ProgramTotal medication prescribed: Pre, N=3264 and Post, N=3192
| Type of Errors errors (%) | Pre | Post | p-value |
|---|---|---|---|
| Total Error | 231 (7.1) | 281 (8.8) | 0.03 |
| Total Error Per Patient | |||
| None | 355 (70.3) | 314 (65.2) | |
| 1 | 103 (20.4) | 88 (18.2) | |
| 2 | 29 (5.7) | 57 (11.8) | |
| 3 | 11 (2.2) | 13 (2.7) | |
| 4 | 2 (0.4) | 10 (2.1) | |
| 5 | 1 (0.2) | 0 | |
| 6 | 4 (0.8) | 0 | |
| Total Clinically Significant Errors | 172 (5.3) | 182 (5.7) | 0.1 |
| Clinically Significant Errors Per Patient | 0.4 | ||
| None | 385 (76.2) | 357 (74.1) | |
| 1 | 89 (17.6) | 88 (31.3) | |
| 2 | 19 (3.8) | 34 (7.05) | |
| 3 | 7 (1.4) | 7 (1.5) | |
| 4 | 2 (0.4) | 3 (0.6) | |
| 5 | 2 (0.4) | 0 | |
| 6 | 1 (0.2) | 0 | |
| Non-Intercepted Errors | 176 (5.4) | 28 (0.9) | < 0.001 |
| None | 392 (77.6) | 465 (95.9) | |
| 1 | 79 (15.6) | 15 (3.1) | |
| 2 | 19 (3.8) | 3 (0.6) | |
| 3 | 9 (1.8) | 1 (0.2) | |
| 4 | 2 (0.4) | 1 (0.2) | |
| 6 | 4 (0.8) | 0 | |
| Types of Errors | |||
| Omission of Medication | 91 (39.4) | 69 (24.6) | 0.2 |
| Wrong Dose | 64 (27.7) | 84 (29.9) | 0.07 |
| Wrong Frequency | 28 (12.1) | 44 (15.7) | 0.05 |
| Wrong Duration | 10 (4.3) | 48 (17.1) | <0.001 |
| Medication Not Indicated | 20 (8.7) | 6 (2.1) | 0.1 |
| Wrong Formulation | 9 (3.9) | 13 (4.6) | 0.3 |
| Wrong Drug | 6 (2.6) | 9 (3.2) | 0.4 |
| Polypharmacy | 1 (0.4) | 3 (1.1) | 0.3 |
| Wrong Instruction | 0 | 3 (1.1) | 0.1 |
| Wrong Route | 1 (0.4) | 2 (0.7) | 0.5 |
| Omission of Instruction | 1 (0.4) | 0 | 0.9 |
In a recent systematic review, during discharge medication reconciliation; median clinical significant error (discrepancies) identified was 34% (IQR 28% - 49%).36 The median percentage of patients with one or more clinically significant errors was 45% (IQR 31% - 56%).36 Average percentage of patients in this study with one or more clinically significant errors was 24.8% and accounted to 5.5% of the total medication errors identified during discharge. The low percentages could have been contributed to medications in wards were reviewed by pharmacist daily in this setting and errors such as dosing adjustments, contraindications and polypharmacy were already intervened much earlier before discharge. Pharmacists detected significantly higher errors involving incorrect duration in the pre-QI phase, we hypothesized that the attentiveness of ward pharmacist increased with the implementation of the QI program.
The most common error, identified during discharge medication reconciliation in this study was omission of medications, 160 (31.2%). This result is in line with other studies, that reported, omission of medications as the most common type of medication errors during discharge which ranged from 85% to 23%.7,10,12
Limitations
The results of this study should be viewed in the light of some limitations. The study was conducted only on weekdays, therefore excluding the percentage of medication errors on weekends, whereby, staffing of physicians and medical officers are lower.
Percentage of discharge patients prescribed with at least one or more errors remained similar and consistent as other components that affect prescribing of discharge medications were not addressed in this QI program. House officers who are responsible for ordering discharge medications are scheduled on a 4-weekly rotation to each medical ward. House officers only require to prioritize ordering discharge and not involved in any other component of the QI program. In order to improve overall medication error, house officers should also be an important part of the QI component.
Interventions that have not been implemented in our setting but have been implemented elsewhere proven to have reduced prescribing error at discharge, such as planning the discharge medications during ward rounds and computerized discharge assistance to ease prescribing discharge medications.21,22,37,38 Giving constructive feedback and training on a regular basis for house officers, who are involved in prescribing discharge medication but rarely discuss these plans with their specialists or medical officers, has also shown a reduction overall errors in discharge prescription order.39,40
Implications and future research
The discharge medication reconciliation service by ward pharmacists continues at the medical wards in this hospital. Discharge medication reconciliation service by ward pharmacists have been expanded to two pediatric wards and two surgical wards.
Sustainability of this service can be tested using similar method use in the study in the future. Future study can also include other components such as training, feedback, allowing other than house officer to order discharge medication can be used to explore overall reduction in discharge medication errors. Other areas of research are to explore (i) implication of medication error in discharge medication on patients’ outcome and (ii) cost implication of pharmacist to prevent clinically significant medication errors at discharge.