INTRODUCTION
Some studies have identified that clinical pharmacy service provides many benefits regarding health outcomes, such as a reduction in post-discharge hospital visits and an improvement in biochemical and physiological parameters.1,2 However, there are few controversial results regarding the benefits of clinical pharmacy services: e.g., no difference in quality of life; cholesterol levels; glycated haemoglobin levels; treatment and hospitalization costs; or the magnitude of improvement in physiological parameters, such as diastolic (DBP) or systolic blood pressure (SBP) after assessing clinical pharmacy services.3-6 Such controversial findings may be justified by the influence of different characteristics of studies, patients, professionals involved, service, health system, and even the socio-cultural context.
In clinical practice, clinical pharmacy services can differ from a basic intervention to a complex one, depending on patient needs and health service characteristics.7 The complexity and variability of different interventions leads to a multiplicity of possible results, which explains the differences in characteristics observed and results of the interventions.8
Cardiometabolic health conditions are highly prevalent in adults and elderly individuals both worldwide and in Brazil, highlighting the importance of the relationship among the characteristics of studies and services and, most importantly, the clinical impact of clinical pharmacy service on patients.9,10 Therefore, scoping reviews that map the studies and study characteristics in a comprehensive way are important tools to qualitatively identify such possible relationships. In contrast, by conducting subgroup or meta-regression analysis, systematic reviews with meta-analyses may help explain the different results identified. To the best of our knowledge, there are no updated systematic reviews that have considered these aspects of clinical pharmacy services performed in Brazil, without restriction for health condition or study type.
Therefore, we aimed to map clinical pharmacy services conducted in Brazil regardless of age, health condition, and setting, and to analyze the clinical impact of clinical pharmacy services among patients with cardiometabolic diseases (cardiovascular diseases and metabolic diseases).
METHODS
This study was conducted as a two-step review. First, a systematic scoping review performed for a broad research question. Second, to answer a specific question related to cardiometabolic diseases, studies identified from the systematic scoping review were then summarised by meta-analyses. Details of the scoping review protocol have been published, and details of the meta-analysis are registered in PROSPERO (CRD42020172041).11
Systematic scoping review
The scoping review was conducted following the Cochrane Collaboration and Joanna Briggs Institute recommendations and was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for scoping review.12-14
The PubMed, LILACS, and Scopus, that includes Embase and grey literature, were searched in March 2019 and updated in March 2020. The search strategies are available in a public repository.15 These electronic searches were complemented by a manual search of the reference list of the included studies. The research question was structured in the PCC format (i.e., population, concept, and context): i) Population: patients regardless of age, sex, or health condition. ii) Concept: studies reporting outcomes and process measures regarding the impact of pharmacist-led interventions with one or more of the following services, regardless of differences in terminologies: health screening, health education, pharmaceutical dispensing, management of minor illness, drug monitoring, medication reconciliation, medication review, and medication therapy management. Studies that described a clinical pharmacy service but did not report the effect of pharmacist-led interventions were excluded. iii) Context: Brazil.
The included study designs were both randomised (RCT, randomized clinical trial) and non-randomised assessments (interventional or observational). Although quasi-experimental studies are considered non-randomised clinical trials, in this review, studies that included two groups of participants were categorised as non-randomised controlled trials (NRCTs) and those that included one group of participants were categorised as quasi-experimental studies without a real control. Publications in non-Roman characters (i.e., Russian, Japanese, or Chinese) were excluded.
Two researchers independently screened the titles and abstracts of retrieved studies to identify irrelevant records. During the second stage, two researchers independently evaluated full-text articles according to defined inclusion and exclusion criteria. Discrepancies were discussed to reach consensus and a third researcher was consulted as a referee when needed.
Data extraction was performed by two reviewers using an ad hoc data extraction tool. The extracted data included specific details about (i) study, service, and participant characteristics (author names, year of publication, federate unit, university, healthcare setting, nature of service, and professionals involved), tools used in the intervention (e.g., educational material), information source, time of follow-up, number of meetings, funding, sample size, age group, target morbidity; (ii) methodological aspects (e.g., study design reported or study design followed); and (iii) reported clinical, humanistic, and economic outcomes, and process measures. All clinical, humanistic, and economic outcomes and process measures related to pharmacist-led intervention were extracted. The parameters used to evaluate clinical pharmacy services in these studies were analytical and comparative; therefore, descriptive and non-analytical outcomes were not considered. Any disagreements between the reviewers were resolved through consensus or by a third reviewer.
The data were processed and presented in either diagrams or tables, accompanied by a narrative summary using descriptive statistics (i.e., absolute values, frequency, medians, and interquartile ranges [IQR 25% and 75%]).
Meta-analysis
The studies to be included in the meta-analyses were identified during the systematic scoping review. The research question was structured according the PICO format (i.e. population, intervention, comparator, and outcome), as follows: i) Population: adult or elderly patients with cardiometabolic diseases; ii) Interventions: clinical pharmacy service conducted in Brazil; iii) Comparator: absence of clinical pharmacy services or usual care; and iv) Outcomes: clinical changes in SBP, DBP, fasting blood glucose, capillary glucose, triglycerides, total cholesterol (TC), low-density lipoprotein (LDL) cholesterol, and high-density lipoprotein (HDL) cholesterol.
Study designs included were the same as those included in the systematic scoping review. Follow-up time was not considered as an inclusion criteria.
Study selection and data extraction were performed by one researcher and reviewed by another researcher. Multiple publications of results from the same study were grouped to avoid data overlap.
Meta-analyses were performed using the R v. 3.6.3/R studio 1.2.5033 software, using the READR, META, and METAFOR packages.16-18 To conduct meta-analyses, transitivity assessment was performed by comparing the inclusion and exclusion criteria of the PICO of parameters. Meta-analyses were conducted using the inverse of variance method. The Sidik-Jonkman method was used to estimate tau2, and the Higgins inconsistency test (I2) was used to assess heterogeneity, considering a random model adjusted by Hartung-Knapp during the process. The results were summarised according to the mean for quasi-experimental studies (i.e., mean difference between pre and post-intervention), and the mean difference for comparative studies (i.e., mean difference between the differences pre- and post-intervention) with 95% confidence interval and a prediction interval.19 The prediction interval can be defined as the expected range of true effects in similar studies carried out in the future.20
The population was categorised into subgroups for analyses. Sensitivity analyses were conducted using the leave-one-out method, and meta-regression could be conducted in a meta-analysis with I2>50% and at least 10 studies to explain the heterogeneity. In addition, statistical and visual (i.e., funnel plot) analyses of publication bias could be conducted only in case of feasibility: meta-analyses with at least 10 studies, different sample sizes, and results.21
According to Cochrane Collaboration ‘Meta-analysis should only be considered when a group of studies is sufficiently homogeneous in terms of participants, interventions and outcomes to provide a meaningful summary'.12 Therefore, data were grouped by outcome, population, and study type and presented in tabular format.
Critical evaluations of the risks of bias of the studies included in the meta-analyses were conducted by two independent reviewers using the second version of the Cochrane tool for assessing risk of bias in randomised trials and Risk of Bias in Non-randomised Studies of Interventions (ROBINS-I) tool.22,23 In the absence of consensus, disagreements were resolved by a third researcher.
The quality of the evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group for each cardiometabolic outcome investigated in randomised and non-randomised studies, which were classified as ‘high', ‘moderate', ‘low', and ‘very low'. Usual care was assumed to be the common comparator.24
Data sharing and data accessibility
The data that support the findings of this study are openly available in OSF (public repository) at http://doi.org/10.17605/OSF.IO/MXZTH.15
RESULTS
Eighty publications (71 studies) were included in the systematic scoping review (Figure 1). The included and excluded publications as well as the detailed characteristics of the studies, services, and patients are available in a public repository (15). The studies were published between 2004 and 2020, with 41 studies published after 2012. The most commonly reported study design was quasi-experimental without a real control (n=29), followed by RCT (n=13). A total of 7,402 patients were included, and the median number of patients per study was 71 (IQR 47.5-131). The region with the greatest number of studies was the Southeast (n=33), and there were no studies from the North region.
Most studies included adult and elderly patients (n=47) with hypertension (n=18) or diabetes (n=10). The main sources of information were patient interviews (n=61) and medical records (n=25).
Clinical pharmacy services were mostly provided in an outpatient setting (n=45) through the association of more than one service (n=63) and for median duration of 240 days (IQR 180-365). The most provided clinical pharmacy service was regarding medication therapy management (n=62), followed by therapeutic drug monitoring (n=21), and medication review (n=26). Some clinical pharmacy services comprised multiple services. Of the included studies, 34 reported services only by pharmacists, 22 reported services from pharmacists working with doctors, and 15 reported services from multi-professional teams that included pharmacists.
There were 120 clinical outcomes, 82 process measures, 18 humanistic, and 2 economic outcomes. Most studies reported process measures (n=59), followed by clinical (n=44), humanistic (n=12), and economic (n=3) outcomes. The outcomes and process measures, according each study, are available in a public repository.15
Regarding process measures, resolution of drug related-problem (DRP) (n=29), the agreement of healthcare professionals to pharmacist`s intervention (n=11), and therapeutic adherence by Morisky or Hayness and Sackett scale (n=4) were major representative categories (Figure 2).
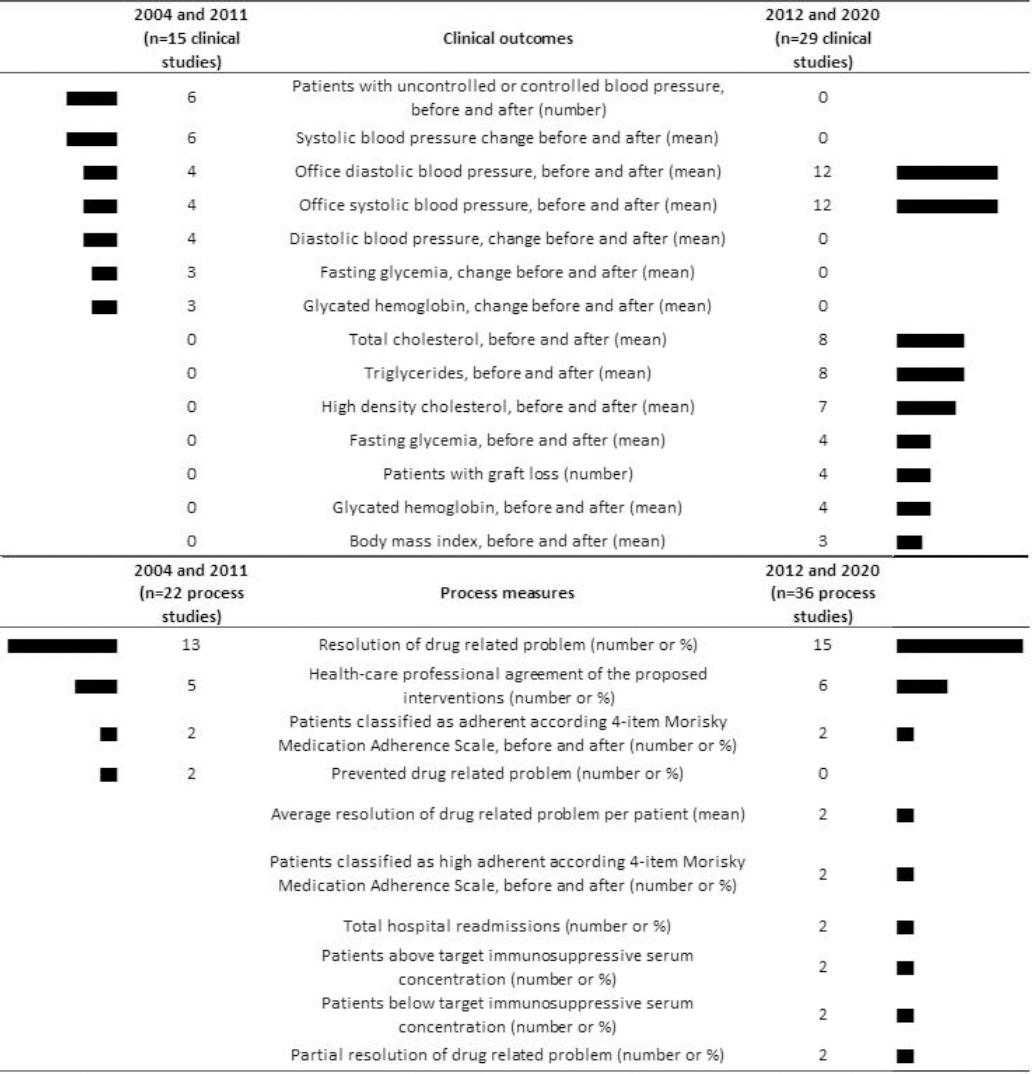
Figure 2. Clinical results and process measures most identified in the systematic scoping review, according to early and recent years
The reported clinical outcomes were mostly related to cardiometabolic diseases and its parameters. Such outcomes, for example blood pressure, were reported in a heterogeneous way in the studies. For instance, there were reports of blood pressure measurements between study time-points (e.g., before and after); measurement during office visits; measurements over 24-hours, daily, and overnight; and measurements for patients who reached their goals or for those with reduced blood pressure. Other common clinical outcomes were body mass index and fasting blood glucose, triglycerides, TC, LDL, and HDL levels (Figure 2). Most clinical outcomes and process measures reported in recent years differ from those reported in the early years (Figure 2).
For the humanistic outcomes, the main assessment was of quality-of-life, using tools such as Short Form 36 Health Survey Questionnaire and Diabetes Quality-of-Life Measure. Economic evaluations consisted only of incremental cost-effectiveness ratio (ICER) for reduction in glycated hemoglobin (HbA1c) (USD per %) (n=2) and ICER by quality-adjusted life years (USD per quality-adjusted life years) (n=1).
Of the 71 studies included in the systematic scoping review, 20 were eligible for the systematic review and meta-analysis of cardiometabolic outcomes, which were stratified according to population (patients with hypertension, diabetes, dyslipidemia, and metabolic syndrome) and study type (comparative and non-comparative). The included and excluded studies are available in the public repository.15
Were identified 12 quasi-experimental studies, 5 RCTs, and 3 NRCTs. There were no observational studies included in the systematic review and meta-analysis because none of them met the inclusion criteria. All studies assessed medication therapy management.
ROBINS-I was used only to assess NRCTs as the tool has been developed to assess the risk of bias in the results of non-randomised studies that compare the health effects of two or more interventions. Therefore, quasi-experimental studies without a real control were considered to have a high risk of bias. In the three NRCTs, the overall bias was assessed as ‘No information', as data in at least one domain was missing, which was not enough to allow for assessment. The domains with ‘No information' were related to confounding data, deviations from intended interventions, and selection of the reported result. Domains that corresponded to ‘low risk of bias' were selection of participants into the study and classification of interventions or deviations from intended interventions; domains that corresponded to ‘moderate risk of bias' included missing data and measurement of outcomes (Table 1a).
Table 1. Risk of bias in non-randomised studies (A) and randomised clinical trials (B)
| A - Non-randomised studies | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Confounding | Selection of participants | Classification | Deviations | Missing data | Measurement | Selections of the reported result | Overall bias | ||||||
| Non-randomised controlled trials | |||||||||||||
| Borges, 2010 | NI | Low | Low | NI | Moderate | Moderate | NI | NI | |||||
| Correr, 2009 | NI | Low | Low | NI | Moderate | Moderate | NI | NI | |||||
| Mori, 2010 | NI | Low | Low | NI | Moderate | Moderate | NI | NI | |||||
| Quasi-experimental study without a real control | |||||||||||||
| Aquino, 2019 | High risk of bias (non-comparative study) | ||||||||||||
| Cazarim, 2016 | High risk of bias (non-comparative study) | ||||||||||||
| Lyra Jr ,2005 | High risk of bias (non-comparative study) | ||||||||||||
| Lyra Jr, 2008 | High risk of bias (non-comparative study) | ||||||||||||
| Nunes, 2012 | High risk of bias (non-comparative study) | ||||||||||||
| Rigoni, 2015 | High risk of bias (non-comparative study) | ||||||||||||
| Silva, 2013 | High risk of bias (non-comparative study) | ||||||||||||
| B - Randomised clinical trial | |||||||||||||
| Randomisation | Deviations | Missing data | Measurement of the outcome | Selection of the reported result | Overall bias | ||||||||
| Azevedo, 2017 | Some concerns | Some concerns | Low | Some concerns | Some concerns | High | |||||||
| Castro, 2006 | Some concerns | Some concerns | Low | Low | Some concerns | High | |||||||
| Obreli-Neto, 2011 | Some concerns | Some concerns | Low | Low | Some concerns | High | |||||||
| Paulo, 2016 | Some concerns | Some concerns | Low | Low | Some concerns | High | |||||||
| Plaster, 2012 | Some concerns | Some concerns | High | Low | Some concerns | High | |||||||
| NI: No information. | |||||||||||||
All RCTs were considered to have a ‘high risk of bias' according to ROB 2 as four had ‘some concerns' in multiple domains (i.e., randomisation, deviations, and selection of the reported result) and one study also presented a high risk of bias owing to missing data in one domain. Although all studies were randomised, none of them mentioned allocation concealment. All studies were unmasked to patient and investigators; however, none of them mentioned absence or balance in deviations from intervention. Regarding the selection of the reported results, no study presented a pre-specified plan (Table 1b).
The meta-analyses performed are summarised in Table 2 and Table 3. The individual results are presented, but the synthesis results of meta-analyses (diamond) are not, owing to high heterogeneity and wide prediction intervals were identified that decreased the validity of syntheses. Despite this high heterogeneity, meta-analyses were conducted to identify the limitations of the current studies. We identified high heterogeneity, even in subgroup analyses stratified by population, which may be related to the characteristics of clinical pharmacy services, time of intervention, age of patients (adults or elderly people), and the severity of the disease at baseline. Despite the significant improvement reported in the confidence interval for individual studies, this finding was not corroborated by the wide prediction interval of meta-analyses. Considering individual studies, the outcomes improved with longer follow-up time and when a larger sample size was used.25,26
Table 2. Data of cardiometabolic outcomes in randomised and non-randomised controlled trials, heterogeneity, and prediction interval
| Study | Experimental | Control | MD | 95%CI | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Total | Mean | SD | Total | Mean | SD | ||||
| Systolic blood pressure (Prediction interval: -36.08; 15.45), mmHg | Diabetes (I2 = 30%) | ||||||||
| Paulo 2016, 6-month | 47 | -4,20 | 15,00 | 42 | -2,60 | 14,00 | -1,60 | (-7,63; 4,43) | |
| Correr 2009, 12-month | 50 | -6,88 | 16,78 | 46 | -11,90 | 26,60 | 5,02 | (-3,96; 14,00) | |
| Metabolic syndrome (I2 = 0%) | |||||||||
| Plaster 2012, 6-month | 34 | -13,00 | 3,00 | 29 | 5,00 | 4,00 | -18,00 | (-19,77; -16,23) | |
| Azevedo 2017, 6-month | 33 | -11,40 | 17,29 | 30 | 5,80 | 20,90 | -17,20 | (-26,73; -7,67) | |
| Hypertension (I2 = 90%) | |||||||||
| Castro 2006, 6-month | 30 | -17,00 | 20,00 | 34 | -12,00 | 19,00 | -5,00 | (-14,59; 4,59) | |
| Mori 2010, 9-month | 21 | -8,80 | 10,50 | 24 | 1,10 | 5,30 | -9,90 | (-14,87; -16,23) | |
| Obreli-Neto 2011, 36-month | 97 | -23,00 | 17,08 | 97 | -0,40 | 13,57 | -22,60 | (-26,94; -18,26) | |
| Diastolic blood pressure (Prediction interval: -22.50; 13.20), mmHg | Diabetes (I2 = 78%) | ||||||||
| Paulo 2016, 6-month | 47 | -4.40 | 11.00 | 42 | -4.90 | 10.00 | 0.50 | (-3.86; 4.86) | |
| Correr 2009, 12-month | 50 | -1.80 | 11.50 | 46 | -9.80 | 14.90 | 8.00 | (2.64; 13.36) | |
| Metabolic syndrome (I2 = 0%) | |||||||||
| Azevedo 2017, 6-month | 33 | -3.90 | 9.76 | 30 | 3.10 | 11.90 | -7.00 | (-12.39; -1.61) | |
| Plaster 2012, 6-month | 34 | -8.00 | 3.00 | 29 | 1.00 | 4.00 | -9.00 | (-10.77; -7.23) | |
| Hypertension (I2 = 79%) | |||||||||
| Castro 2006, 6-month | 30 | -10.00 | 10.00 | 34 | -6.00 | 14.00 | -4.00 | (-9.91; 1.91) | |
| Mori 2010, 9-month | 41 | -9.40 | 8.60 | 34 | -2.70 | 5.70 | -6.70 | (-9.96; -3.44) | |
| Obreli-Neto 2011, 36-month | 97 | -14.80 | 14.60 | 97 | -1.90 | 9.30 | -12.90 | (-12.90; -9.46) | |
| Total cholesterol (Prediction interval: -8.96; 56.32), mg/dl | Diabetes (I2 = not applicable) | ||||||||
| Paulo 2016, 6-month | 47 | -9.57 | 31.30 | 42 | 0.40 | 39.00 | -9.97 | (-24.78; 4.84) | |
| Metabolic syndrome (I2 = 92%) | |||||||||
| Azevedo 2017, 6-month | 33 | 8.40 | 38.70 | 30 | -3.60 | 41.90 | 12.00 | (-7.97; 31.97) | |
| Plaster 2012, 6-month | 34 | -23.00 | 7.81 | 29 | 1.00 | 6.08 | -24.00 | (-27.43; -20.57) | |
| Hypertension (I2 = not applicable) | |||||||||
| Obreli-Neto 2011, 36-month | 97 | -16.60 | 26.40 | 97 | 4.40 | 32.10 | -21.00 | (-29.27; -12.73) | |
| LDL-cholesterol (Prediction interval: -90.52; 81.87), mg/dl | Diabetes (I2 = 63%) | ||||||||
| Azevedo 2017, 3-month | 33 | 10.90 | 26.10 | 30 | -3.10 | 34.90 | 14.00 | (-1.35; 29.35) | |
| Plaster 2012, 6-month | 34 | -35.00 | 5.57 | 4 | 29.00 | 129.00 | -64.00 | (-190.53; 62.53) | |
| Paulo 2016, 6-month | 47 | -8.20 | 26.80 | 42 | -0.80 | 33.70 | -7.40 | (-20.15; 5.35) | |
| Hypertension (I2 = not applicable) | |||||||||
| Obreli-Neto 2011, 36-month | 97 | -10.40 | 41.70 | 97 | 2.80 | 11.30 | -13.20 | (-21.80; -4.60) | |
| HDL-c (Prediction interval: -4.77; 22.25), mg/dl | Diabetes (I2 = not applicable) | ||||||||
| Paulo 2016, 6-month, both sex | 47 | 0.63 | 7.80 | 42 | 0.26 | 17.00 | 0.37 | (-5.23; 5.97) | |
| Metabolic syndrome (I2 = 0%) | |||||||||
| Azevedo 2017, 6-month, both sex | 33 | 5.30 | 24.80 | 30 | -3.20 | 12.70 | 8.50 | (-1.11; 18.11) | |
| Plaster 2012, 6-month, men | 10 | 7.00 | 2.65 | 12 | -4.00 | 3.00 | 11.00 | (8.64; 13.36) | |
| Plaster 2012, 6-month, women | 24 | 7.00 | 1.73 | 17 | -4.00 | 3.00 | 11.00 | (9.41; 12.59) | |
| Hypertension (I2 = not applicable) | |||||||||
| Obreli-Neto 2011, 36-month, both sex | 97 | 10.00 | 7.50 | 97 | 0.00 | 3.00 | 10.00 | (8.39; 11.61) | |
| Triglycerides (Prediction interval: -125.16; 54.73), mg/dl | Diabetes (I2 = not applicable) | ||||||||
| Paulo 2016, 6-month | 47 | -8.83 | 86.90 | 42 | 9.70 | 85.00 | -18.50 | (-54.28; 17.22) | |
| Metabolic syndrome (I2 = 84%) | |||||||||
| Azevedo 2017, 6-month | 33 | -42.20 | 88.60 | 30 | 21.70 | 85.70 | -63.90 | (-106.95; -20.85) | |
| Plaster 2012, 6-month | 34 | -21.00 | 14.10 | 29 | -33.00 | 114.00 | 12.00 | (-29.63; 53.63) | |
| Hypertension (I2 = 0%) | |||||||||
| Mori 2010, 9-month | 18 | -1.90 | 31.70 | 15 | 48.70 | 71.30 | -50.60 | (-89.54; -11.66) | |
| Obreli-Neto 2011, 36-month | 97 | -53.50 | 133.00 | 97 | -1.90 | 9.70 | -51.60 | (-78.12; -25.08) | |
| Fasting glycemia (Prediction interval: -74.21; 14.08), mg/dl | Metabolic syndrome (I2 = 77%) | ||||||||
| Azevedo 2017, 6-month | 33 | -7.50 | 47.20 | 30 | 14.90 | 37.10 | -22.40 | (-43.26; -1.54) | |
| Plaster 2012, 6-month | 34 | -68.00 | 13.80 | 29 | -8.00 | 78.30 | -60.00 | (-88.87; -31.13) | |
| Diabetes (I2 = 0%) | |||||||||
| Correr 2009, 12-month | 50 | -20.10 | 42.60 | 46 | 4.30 | 61.60 | -24.40 | (-45.76; -3.04) | |
| Borges 2010, 12-month | 33 | -36.80 | 92.10 | 31 | -20.70 | 89.10 | -16.10 | (-60.50; 28.30) | |
| Hypertension (I2 = not applicable) | |||||||||
| Obreli-Neto 2011, 36-month | 97 | -27.20 | 43.00 | 97 | 1.10 | 21.60 | -28.30 | (-37.87; -18.73) | |
| HbA1c (Prediction interval: -3.74; 1.58), % | Diabetes (I2 = 70%) | ||||||||
| Paulo 2016, 6-month | 47 | -0.12 | 1.40 | 42 | 0.41 | 2.00 | -0.53 | (-1.26; 0.20) | |
| Correr 2009, 12-month | 50 | -2.20 | 2.20 | 46 | -0.30 | 1.70 | -1.90 | (-2.68; -1.12) | |
| Borges 2010, 12-month | 33 | -0.90 | 1.50 | 31 | 0.50 | 1.50 | -1.40 | (-2.14; -0.66) | |
| Hypertension (I2 = not applicable) | |||||||||
| Obreli-Neto 2011, 36-month | 97 | -0.70 | 0.75 | 97 | 0.00 | 0.50 | -0.70 | (-0.88; -0.52) | |
CI: confidence interval; MD: mean difference; SD: standard deviation.
Table 3. Data of cardiometabolic outcomes in quasi-experimental studies, heterogeneity, and prediction interval
| Study | Total | Mean difference between before-after | SD | 95%CI | |
|---|---|---|---|---|---|
| Systolic blood pressure (Prediction interval: -35.23; 5.19). mmHg | Diabetes (I2 = 98%) | ||||
| Zatta 2017, 2-month | 18 | -5.00 | 21.63 | (-14.99; 4.99) | |
| Nunes 2012, 3-month | 58 | -5.20 | 18.60 | (-9.99; -0.41) | |
| Aquino 2019, 12-month | 47 | -10.00 | 36.87 | (-20.54; 0.54) | |
| Zubioli 2013, 12-month | 50 | -30.40 | 2.78 | (-31.17; -29.63) | |
| Dyslipidemia (I2 = not applicable) | |||||
| Silva 2013, 6-month | 14 | -27.00 | 13.30 | (-33.97; -20.03) | |
| Hypertension (I2 = 90%) | |||||
| Souza 2008, 2-month | 9 | -3.61 | 9.70 | (-9.94; 2.72) | |
| Cazarim 2016, 12-month | 104 | -7.20 | 18.00 | (-10.66; -3.74) | |
| Rigoni 2015, NR | 40 | -11.00 | 24.47 | (-18.58; -3.42) | |
| Lyra Jr 2008, 12-month | 30 | -18.00 | 18.38 | (-24.58; -11.42) | |
| Lyra Jr 2005, 12-month | 30 | -18.00 | 2.30 | (-18.82; -17.18) | |
| Souza 2007, 12-month | 44 | -18.60 | 17.72 | (-23.84; -13.36) | |
| Souza 2009, NR | 10 | -25.00 | 19.50 | (-37.09; -12.91) | |
| Diastolic blood pressure (Prediction interval: -22.41; 5.59). mmHg | Diabetes (I2 = 99%) | ||||
| Zatta 2017, 2-month | 18 | -4.00 | 10.80 | (-8.99; 0.99) | |
| Nunes 2012, 3-month | 58 | -1.70 | 9.40 | (-4.13; 0.73) | |
| Aquino 2019, 12-month | 47 | -2.00 | 23.40 | (-8.69; 4.69) | |
| Zubioli 2013, 12-month | 50 | -21.90 | 2.30 | (-22.51; -21.23) | |
| Dyslipidemia (I2 = not applicable) | |||||
| Silva 2013, 6-month | 14 | -11.00 | 4.60 | (-13.41; -8.59) | |
| Hypertension (I2 = 91%) | |||||
| Souza 2008, 2-month | 9 | -2.70 | 5.50 | (-6.33; 0.85) | |
| Cazarim 2016, 12-month | 104 | -4.40 | 10.70 | (-6.45; -2.35) | |
| Rigoni 2015, NR | 40 | -4.50 | 15.00 | (-9.15; 0.15) | |
| Souza 2007, 12-month | 44 | -9.10 | 11.60 | (-12.52; -5.68) | |
| Lyra Jr 2008, 12-month | 30 | -12.00 | 14.70 | (-17.27; -6.73) | |
| Lyra Jr 2005, 12-month | 30 | -12.00 | 3.00 | (-13.07; -10.93) | |
| Souza 2009, NR | 10 | -16.50 | 17.50 | (-27.35; -5.65) | |
| Total cholesterol (Prediction interval: -95.18; 37.05). mg/dl | Diabetes (I2 = 54%) | ||||
| Nunes 2012, 3-month | 58 | -32.90 | 41.61 | (-43.61; -22.19) | |
| Aquino 2019, 12-month | 47 | -7.00 | 91.25 | (-33.09; 19.09) | |
| Zubioli 2013, 12-month | 50 | -23.70 | 5.87 | (-25.33; -22.07) | |
| Dyslipidemia (I2 = not applicable) | |||||
| Silva 2013, 6-month | 14 | -63.00 | 35.59 | (-81.65; -44.35) | |
| Hypertension (I2 = not applicable) | |||||
| Cazarim 2016, 12-month | 104 | -18.10 | 40.10 | (-25.81; -10.39) | |
| LDL-cholesterol (Prediction interval: -143.39; 89.48). mg/dl | Dyslipidemia (I2 = not applicable) | ||||
| Silva 2013, 6-month | 14 | -62.70 | 29.05 | (-77.92; -47.48) | |
| Diabetes (I2 = 87%) | |||||
| Zubioli 2013, 12-month | 50 | -12.30 | 4.80 | (-13.63; -10.97) | |
| Nunes 2012, 3-month | 58 | -28.70 | 33.75 | (-37.39; -20.01) | |
| Aquino 2019, 12-month | 47 | -6.90 | 29.98 | (-15.47; 1.67) | |
| HDL-cholesterol (Prediction interval: -9.80; 12.72). mg/dl | Diabetes (I2 = 97%) | ||||
| Nunes 2012, 3-month, both sex | 58 | 3.60 | 18.96 | (-1.28; 8.48) | |
| Zubioli 2013, 12-month, both sex | 50 | 5.97 | 1.40 | (5.58; 6.36) | |
| Aquino 2019, 12-month, women | 36 | -0.50 | 4.35 | (-1.92; 0.92) | |
| Aquino 2019, 12-month, men | 11 | -1.90 | 4.88 | (-4.78; 0.98) | |
| Dyslipidemia (I2 = not applicable) | |||||
| Silva 2013, 6-month, both sex | 14 | -1.60 | 14.80 | (-9.35; 6.15) | |
| Triglycerides (Prediction interval: -147.45; 32.11). mg/dl | Diabetes (I2 = 15%) | ||||
| Nunes 2012, 3-month | 58 | -72.40 | 129.69 | (-105.78; -39.02) | |
| Aquino 2019, 12-month | 47 | -33.00 | 172.17 | (-82.22; 16.22) | |
| Zubioli 2013, 12-month | 14 | -48.10 | 14.31 | (-55.59; -40.61) | |
| Dyslipidemia (I2 = not applicable) | |||||
| Silva 2013, 6-month | 14 | -92.00 | 106.23 | (147.64; -36.36) | |
| Glycemia (Prediction interval: -247.56; 199.46). mg/dl | Diabetes (I2 = 83%) | ||||
| Zatta 2017, 2-month | 18 | -9.00 | 52.11 | (-33.07; 15.07) | |
| Nunes 2012, 3-month | 58 | -13.90 | 81.21 | (34.80; 7.00) | |
| Zubioli 2013, 12-month | 50 | -39.50 | 6.58 | (-41.32; -37.68) |
CI: confidence interval; SD: standard deviation.
Sensitivity analyses by leave-one-out method and meta-regression were not conducted, considering the small size of subgroups (number of studies and participants). It was not possible to conduct statistical and visual analyses of publication bias for any meta-analysis as the requirements of a minimum number of studies or different results and sample sizes were not met. However, considering that most studies have identified a beneficial effect of clinical pharmacy services, regardless of low statistical power, a publication bias, which can be qualitatively identified, might exist.
Considering the high risk of bias; heterogeneity; and imprecision for all outcomes, populations, and study types identified for most studies, the general quality of the evidence (GRADE) for cardiometabolic outcome reported is ‘very low'.
DISCUSSION
From the systematic scoping review, were identified 71 studies that assessed the efficacy or effectiveness of clinical pharmacy services for patients regardless of age, health conditions and system that included 20 different clinical conditions, mainly cardiometabolic diseases. Our findings corroborate with an overview of systematic reviews with meta-analysis without country restrictions that identified a predominance of cardiovascular disease (73.9% of meta-analyses).27
In the Brazilian scenario, publications regarding to clinical pharmacy services were first published in 2004, which can be justified by the fact that the recognition of pharmaceutical care in Brazil only occurred in 2002.28 This does not indicate an absence of patient care before this year, but it demonstrates the effects of its recognition and the encouragement of clinical practice. The number of studies related to clinical pharmacy services further increased, mainly after 2012.
The increased role and autonomy of pharmacists may reflect changes in the pharmaceutical academic education regarding increased emphasis on patient care (Resolution CNE/CES n. 2/2002 and Resolution CNE/CES n. 6/2017), increased multi-professional residences (Law n. 11,129/2005), regulation of professional practice in clinical settings (i.e., federal council of pharmacy resolutions n. 499/2008, 505/2009, 585/2013, and 586/2013), and the implementation of Qualifar-SUS, a programme aimed to include and consolidate clinical pharmacy services in the Brazilian healthcare system (Ordinance n. 1,214/2012), among other actions.29-36
Bonetti et al. mainly reported clinical outcomes (37.6%), followed by process measures, primarily adherence and hospital admissions (15.3%), which was partially corroborated by our findings.27 Although, process measures related to hospital admission were only found in two studies, these measures, mainly DRP and healthcare professional agreement with pharmacist intervention, as well as clinical outcomes, were highly prevalent. Despite the unquestionable relevance of humanistic and economic outcomes , a low number of studies assessed these types of outcomes. This finding could be justified by to the difficulty of robustly assessing quality of life or health-related quality of life, considering the extension of tools and time for completing questionnaire (in general, it requires 8-15 minutes to be filled in). Moreover, to assess economic outcomes, greater expertise from researchers related to economic health assessment is needed.
A discrepancy was also observed between the measures reported in recent and early years. Although in the early years there was a predominance of outcomes related to blood pressure and its variations, in recent years, the variations in the way of assessing blood pressure have decreased and outcomes related to dyslipidemia have been assessed to a greater extent. For process measures, the early publications (2004-2011) show an emphasis on DRP and the acceptance of health professionals following pharmaceutical recommendations, whereas in the recent years (2012-2020), adherence assessments were also reported. This discrepancy suggests a change in the perception of researchers about central measures but simultaneously prevents the comparison of the effect of clinical pharmacy services between recent and early studies.
In the study by Bonetti et al., most clinical outcomes were cardiometabolic parameters. Here, a variety of outcomes related to the same parameter (e.g. SBP reported by mean difference, and patients that reached the SBP goal or who decreased SBP) were identified, which hinders the comparison of their results with those of other studies. Thus, this finding highlights the importance of clinical pharmacy service studies to follow the ‘core outcome set' (COS) for each disease, improving the consistency and relevance of new findings and enabling the results of trials to be compared and combined. ‘COMET - Core Outcome Measures in Effectiveness Trials' defines COS as a set of essential outcomes as an agreed minimum set that must be selected, collected, measured, and reported in all RCTs regarding a particular condition or intervention.37
Significant improvements in the confidence interval for the outcomes of SBP and DBP, HbA1c, fasting glucose, HDL-cholesterol, and triglycerides (continuous outcomes) were reported in individual studies. However, these results were not confirmed by the prediction interval, suggesting that future studies may report results contradictory to those identified in this review.The review conducted by Martinez-Mardones et al. in patients with cardiometabolic diseases identified benefits for control of blood pressure, diabetes, and TC outcomes (dichotomous outcomes), presenting more consistent results than this review, possibly because they considered different outcomes as well as a larger number of studies from different countries.38
Tan et al. conducted an international systematic review of RCTs on cardiometabolic outcomes.2 The authors identified methodological limitations like those of Brazilian studies (i.e. allocation concealment), suggesting how the effect of these limitations can be underestimated by researchers or even because of the difficulty of implementing this care. Notably, most researchers agree on the importance of randomisation to reduce the risk of bias while assessing the characteristics of participants unevenly distributed between groups. However, it seems that only few researchers recognise that for the randomisation process to be reliable, it is also necessary to guarantee allocation concealment to prevent professionals from directing patients to groups.
A great heterogeneity among the studies was identified, even in populations with the same health problems. This heterogeneity may be due to population size as well as due to differences in intervention time. In quasi-experimental, RCTs, and NRCTs, a decrease in SBP and DBP was observed with an increase in intervention time. In this context, considering clinical parameters that depend on changes in lifestyle, and chronic drug therapy use as well as require a longer time for their control and maintenance (i.e. total and LDL cholesterol), an appropriate intervention time is essential.39 Thus, certain outcomes may require longer intervention times for them to be the most effective interventions.
Considering this, to appropriately evaluate clinical pharmacy services and their efficacy, new studies should be conducted with efficient methods and reporting techniques. The heterogeneity of studies could have been decreased if there was a pre-planned subgroup analysis (e.g., subgroups of elderly patients and severity health problem) and a transparent description of clinical pharmacy service (e.g., following a reporting checklist such as DEPICT or PaCIR). As international reviews had similar limitations to those conducted in Brazil, these findings are relevant not only in Brazil but also globally and can be used to favour outlining global studies.
As a limitation of this review, there was a risk of missing existing studies, as in all reviews, and in the scope of clinical pharmacy services; this risk may be increased owing to low adherence to standardised terminologies, which makes it difficult to locate all studies related to clinical pharmacy services, even with comprehensive searches. Thus, to maintain consistency and not influence the predominance of a given clinical pharmacy service over another, it was chosen to include only the term ‘pharmacist', in line with the concept of scoping review (pharmacist-led services). In addition, grey literature and manual searches were conducted, and only a few studies were found.
Secondly, it was not considered all grey literature (i.e., dissertations and theses) and letters, which might compromise the coverage of findings. Nonetheless, dissertations, theses, and letters present a low probability of complete data, precluding the reliable extraction of data and risk of bias assessment.
Thirdly, there could not be an explanation in depth the possible relationships between the characteristics of studies, clinical pharmacy services, and participants and their results in view of the poor reporting of studies and the small number of studies per meta-analysis, which prevented reliable meta-regressions and sensitivity analysis.
Finally, the risk of bias of the studies included in the meta-analysis was high and prediction intervals were wide, which precluded the representation of the synthesis results of the meta-analysis.
CONCLUSIONS
Most of clinical pharmacy services were regarding medication therapy management and were provided in an outpatient setting for adults or elderly people with cardiometabolic diseases. In addition, most included studies were quasi-experimental and published by research groups from Southeast Brazil. Process measures (e.g. resolution of DRP) were widely used as indicators, followed by clinical (e.g. change in SBP), humanistic (e.g. change in quality of life score assessed by Short Form 36 Health Survey Questionnaire), and economic outcomes (ICER for reduction in HbA1c).
Regarding the clinical impact of the clinical pharmacy services, a low confidence in view of the high risk of bias or insufficient information to assess the risk of bias of the studies, reduced statistical power, heterogeneity of the studies, and wide prediction interval were identified. Although most studies suggest a potential benefit of clinical pharmacy services in cardiometabolic outcomes, larger studies with adequate design and greater homogeneity are required to confirm this potential clinical impact, as well as to better understand the services that provide the best outcomes and the population subgroups most likely to benefit from such services.















