INTRODUCTION
Diet related diseases are on the rise worldwide. Poor diet increases risk for chronic and metabolic diseases such as obesity and dyslipidemias. Dietary patterns analysis (DP) has emerged as a useful method for the description of relationships between diet and health. The principal component analysis method (PCA) extracts correlation coefficients between foods or dietary elements to classify subjects in groups according to their consumption 1,2.
Evidence based on prospective studies indicates that prudent DP (high intakes of fruits, vegetables, whole grains and fish, and low intakes of saturated fats) were associated with decreased cardiovascular disease in the general population, while those DP with high intake of red or processed meats, sugars or alcoholic beverages were associated with an increased risk 3,4. The evidence is still inconsistent, especially in young and healthy people; only a few epidemiological studies have demonstrated association between DP and serum lipid concentrations 5,6. Therefore, low consumption of fruits, vegetables and fiber, and high consumption of energy, sugars, saturated fats and animal protein increase the risk of chronic non-communicable diseases such as obesity, considered as a public health problem worldwide. Since 2009, a cross-sectional study revealed that DP including cereals, small fish, crackers, fruits-vegetables, and olive oil were related to a beneficial cardiovascular disease risk profile, in contrast with those DP with sweets, red meat, margarine, nuts with salt and cheese, which were related to an unfavorable risk profile in adults 7.
A recent meta-analysis determined that prudent DP have positive effects on biomarkers associated with adiposity, insulin resistance and especially with inflammation in adults 8. Also, in a multi-city cohort study, authors reported that a prudent DP was associated with reduced plasma concentrations of apo B, total cholesterol and LDL-cholesterol, but a western DP, characterized by higher intake of eggs, pastry-cakes, pizza, snacks, refined grains, red meat, vegetable oils and poultry was not 9.
Mexican adults have reported a rapid increase in hypercholesterolemia, hypertriacylglyceridemia and low HDL-cholesterol trends since past decades 10, being the most common lipid abnormality low HDL-cholesterol, a condition that promotes cardiovascular risk factors for morbidity and mortality in addition to the burden of chronic diseases in Mexico 11.
According to the last National Health and Nutrition Survey carried out in 2016 (ENSANUT 2016), the prevalence of abdominal obesity in Mexican adults was 65.4% for men and 87.7% for women. It is known that obesity increases the risk for diabetes mellitus 12,13. Particularly in young healthy adults in Mexico, researchers have found that abdominal obesity is the most prevalent metabolic syndrome component 14.
With respect to diet, the first study of adherence to the World Health Organization dietary recommendations in Mexico reported the presence of a double burden of malnutrition in some segments of the population. A very low percentage of Mexican adults (< 35%) consume the recommended intake of fruits and vegetables, making Mexico one of the countries with the lowest consumption of fruits and vegetables worldwide 12. This dietary situation seems to remain currently, since ENSANUT 2016 reported that one-half of the adults in Mexico eat fruits while only 42.3% eat vegetables. In contrast, the food group with the highest consumption was sweetened beverages 15. These conditions make diet poor in quality; therefore, the study of DP has special interest.
For this study, our principal aim was to identify major dietary patterns associated with central-obesity and serum lipid concentrations in healthy Mexican adults.
MATERIAL AND METHODS
PARTICIPANTS
The data used in this study were obtained from 102 healthy adults. During seven months follow-up, a sample of 102 from a total of 134 adult school-workers (76% participation rate) completed anthropometric and dietary data. LDL-, HDL- serum total cholesterol and triacylglycerides were determined in all subjects for analysis.
All participants denominated "administrative staff" carried out activities such as laboratory technicians, clerks, cleaning or maintenance in the School of Medicine of the Autonomous University of the State of Mexico, located in the central region of México.
Participants eligible for inclusion were men or women, aged 20-70 years old, with body mass index (BMI) ≥ 20 kg/m2 according to the World Health Organization (WHO) criteria, who agreed to provide a serum-sample as well as to participate in dietary and anthropometric evaluations. Health or previous disease conditions in each participant was registered, but it was not considered as an exclusion criteria. The study was approved by the Ethics Committee of the School of Medicine (CONBIOETICA15CEI03420140313). Written informed consents were obtained from all participants prior to their voluntary participation.
Gender, age, physical activity, smoking habits, concomitant medication and level of education were obtained from a self-administered questionnaire. To compare variables between sexes, Student's t test was used for age, BMI and WC; Chi-square Fisher's exact test was used to compare physical activity, smoking, concomitant medication and level of education. No statistically significant differences were observed for age, physical activity, concomitant medication or level of education by sex. BMI and WC were considered for obesity diagnosis.
ANTHROPOMETRIC MEASUREMENTS
All measurements were performed by trained-standardized personnel using standard procedures. Body weight was recorded to the nearest 0.1 kg using a digital electronic scale (Tanita(r) model 1631); height was recorded to the nearest 0.1 cm using a wall stadiometer (Seca(r) model 1013522). BMI was computed as a ratio of weight (kg): height squared (m2). BMI cut-off points defined by the WHO according to height and sex were categorized as < 18.5: underweight; 18.5-24.9: normal; 25-29.9: overweight; and ≥ 30.0: obese 16,17. Waist circumference was expressed in centimeters, and recorded to the nearest 0.1 cm using a flexible vinyl Gülick tape at the level of midpoint between the iliac crest and the lower border of tenth rib, at the end of normal expiration in supine position. Central-obesity was defined by waist circumference ≥ 80 cm for females, and ≥ 90 cm for males according to the International Diabetes Federation criteria (IDFC) 18). The percentage of fat mass was determined by bioimpedance with the same calibrated electronic scale used for weight measurement. High body fat proportion was defined as > 25% for men and > 32% for women 19.
BIOCHEMISTRY DATA
Participants came to the Nutrition Research Laboratory facilities, after an overnight fasting for 10-12 hours. Two venous blood samples were obtained in suitable Vacutainer(r) tubes and centrifuged. Total-cholesterol, LDL-cholesterol, VLDL-cholesterol, HDL-cholesterol and triacylglycerides (mg/dl) were measured in a Selectra(r) autoanalyzer equipment by automatized enzymatic-colorimetric methods. LDL-cholesterol was calculated by the Friedewald equation. Altered serum lipid concentrations were classified according to these criteria: total-cholesterol: ≥ 200 mg/dl; triacylglycerides: ≥ 150 mg/dl; LDL-cholesterol: ≥ 150 mg/dl; and low HDL-cholesterol: ≤ 50 mg/dl for women and ≤ 40 mg/dl for men 20,21.
DIETARY ASSESSMENT
Multiple 24-hour recalls (24-h recall)
According to the information reported by each participant, frequency, type and form of food consumption were used to assess habitual dietary intakes; 24-hour recalls interviews were carried out over a seven month period, including weekdays and weekends. Household measures registered were converted into units of volume or weight according to the Mexican equivalents food system. Nutrimind(r) software 2015 was used to obtain nutrients from 144 different registered foods. Sixteen food-groups were considered depending on the foods items derived from participant's recalls: peanuts-nuts-almonds, vegetables, fruits, no fat cereals, fish and sea food, legumes, lean meat, high fat meat, alcoholic beverages, dairy products, oils and fats, saturated fats, sugars, high fat cereals and fast food (ultra-processed food).
Dietary Patterns (DP)
After categorizing 144 food-items into 16 food-groups, factor analysis by principal component analysis (PCA) procedures with Varimax orthogonal rotation were used to identify DP, based on the eating frequency of each food group. Factor loadings refer the coefficients that define the components in each DP, named according to the food-groups with the highest factor loadings. The number of factors was based on the components with an eigenvalue of 1 and the interpretability of the factors. The eigenvalues signify the amount of variance explained by each of the factors. If a food item had an absolute correlation ≥ 0.5, it was considered to load on a factor. Factorability of data was confirmed with the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy and Bartlett's test of sphericity achieving correct estimation of statistical significance. Each factor corresponds to each dietary pattern, therefore, three dietary patterns were derived: healthy-pattern, risk-pattern and empty-pattern, based on the above.
The healthy-pattern included highest consumption of nuts, almonds, peanuts, vegetables, fruits, no fat cereals and fish or sea food, although the risk pattern presented the highest consumption of cereals with fat, high fat meat, fast food and oils and fats. The empty dietary pattern included the highest intakes of alcoholic beverages and sugars. We named dietary patterns considering general dietetic recommendations for healthy adults. All dietary data were adjusted by energy intake.
Statistical analysis
Participants' characteristics were compared by gender, presented as means, standard deviations, and percentages for categorical variables. Student's t test, Chi-square test or ANOVA were used to compare means; logistic regression models were used to explore the association between DP and central-obesity (present/absent) and serum lipid concentrations (desirable/elevated) by calculating odds ratio (OR) with 95% confidence intervals (95% CI). The reference condition (OR = 1.0) represented the chances of being included in the healthy pattern, according to the different anthropometric or lipid categories. Statistical significance was considered at p < 0.05. Statistical analyses were performed with SPSS(r) 21.0 software (UAEM).
RESULTS
CHARACTERISTICS OF PARTICIPANTS
The characteristics of participants are summarized in Table 1. The mean BMI and WC were 28.3 kg/m2 and 97.1 cm for men and 26.2 kg/m2 and 85.2 cm for women, respectively. BMI and WC as continuous variables were higher in men (p < 0.05). As expected, mean of body fat mass percentage was higher among women; however, the prevalence of excessive body fat mass was not dependent on sex by classifying body fat mass percentage. Also, there were no significant differences between women and men on age nor physical activity, concomitant medication and educational level (p > 0.05). Smoking habit was more prevalent in males.
Table I Characteristics of participants
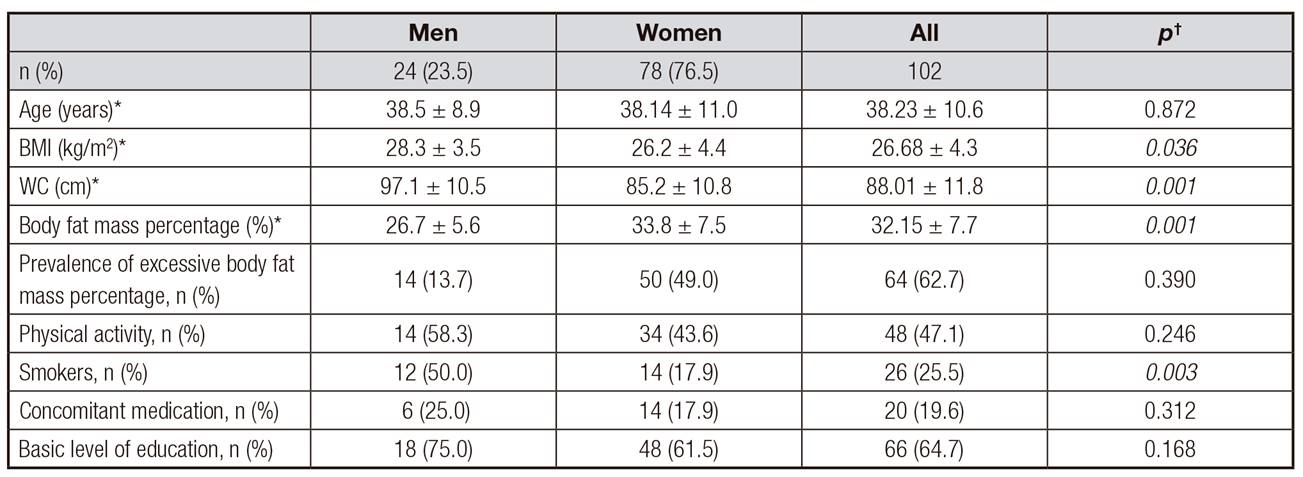
BMI: body mass index; WC: waist circumference. *Age, body mass index (BMI), waist circumference (WC) and body fat mass percentage are presented as mean ± standard deviation (SD). Categorical variables are presented as a percentage. †Student's t test was used for continuous variables and Chi-square, Fisher's test, for categorical variables.
DIETARY PATTERNS
Table 2 shows factor loadings for the three DP between participants. We extracted three distinct DP with factor loadings > 0.50: the first one was characterized by a high intake of fruits, vegetables, non-fat cereals, fish and shellfish, legumes and fats with protein, named healthy pattern; the second one, named risk pattern, was highly correlated with high-fat food, high-saturated fats, fast-foods, high-fat meals, sausages, and sweet-beverages; and the third one, named empty pattern, was highly correlated with alcohol and soft-drinks. These three DP explained 23.7%, 17.4% and 10.2% of the variance of food intake, respectively.
Average consumption of food groups, energy and nutrients is presented in Table 3. Participants in the healthy DP were those who consumed fewer cereals with fat, dairy products and alcoholic beverages, while those in the risk-DP had greater amounts of high fat meat. Adults in the empty-DP group had the highest intake of dairy products and alcohol (p < 0.05). Adults in the healthy-DP group had the lowest cholesterol consumption (p = 0.007) and the highest monounsaturated fats consumption, with a p-value close to statistical significance (p = 0.056). For the other components, while there were no significant differences between DP, although it was observed that adults in the healthy-DP presented lower energy consumption, those in the risk-DP ate more proteins and fats, and those in the empty-DP consumed higher amounts of carbohydrates, polyunsaturated, and saturated fats than adults in the other DP. In addition, it is notorious that with respect to the recommendations for healthy adults, average fiber intake was low in the three DP (< 30 g/day).
Table II Factor loadings for three dietary patterns among adults derived by principal component analysis*

Correlation values ≥ 0.50 are presented in bold style, for easy identification of the major food group intakes. Variance explained is expressed as a percentage. *Adjusted for energy intake.
Table III Intake of dominant food-groups, energy and nutrients for three dietary patterns derived by principal component analysis among healthy adults*

*All values are mean ± standard deviation, adjusted for energy intake except for the energy variable.
†p-values calculated with ANOVA test adjusted by energy intake.
DIETARY PATTERNS, CENTRAL-OBESITY AND SERUM LIPID CONCENTRATIONS
Table 4 shows the data on obesity and overweight, central-obesity, body fat-mass percentage, total cholesterol, LDL-cholesterol, HDL-cholesterol, triacylglycerides, and atherogenic index according to DP. Since there were more women in the healthy pattern, it was expected that the highest body fat-mass percentage was observed in this dietary pattern (p < 0.05). Nonetheless, it should be noted that body fat mass percentage was the highest in women and men in the healthy pattern (p < 0.05). Also, it should be noted that the mean of body fat mass percentage was above the healthy limits among adults in the three DP. In addition, for a more complete analysis, a subsample of 24 women was extracted to analyze their distribution in the three dietary patterns based on the consumption of the characteristic food groups of each of them. As no statistically significant differences were found, we assume that sex does not determine the classification of participants in dietary patterns.
Table IV Association between obesity, central-obesity, body fat mass percentage, serum lipid concentrations and dietary patterns in healthy adults*
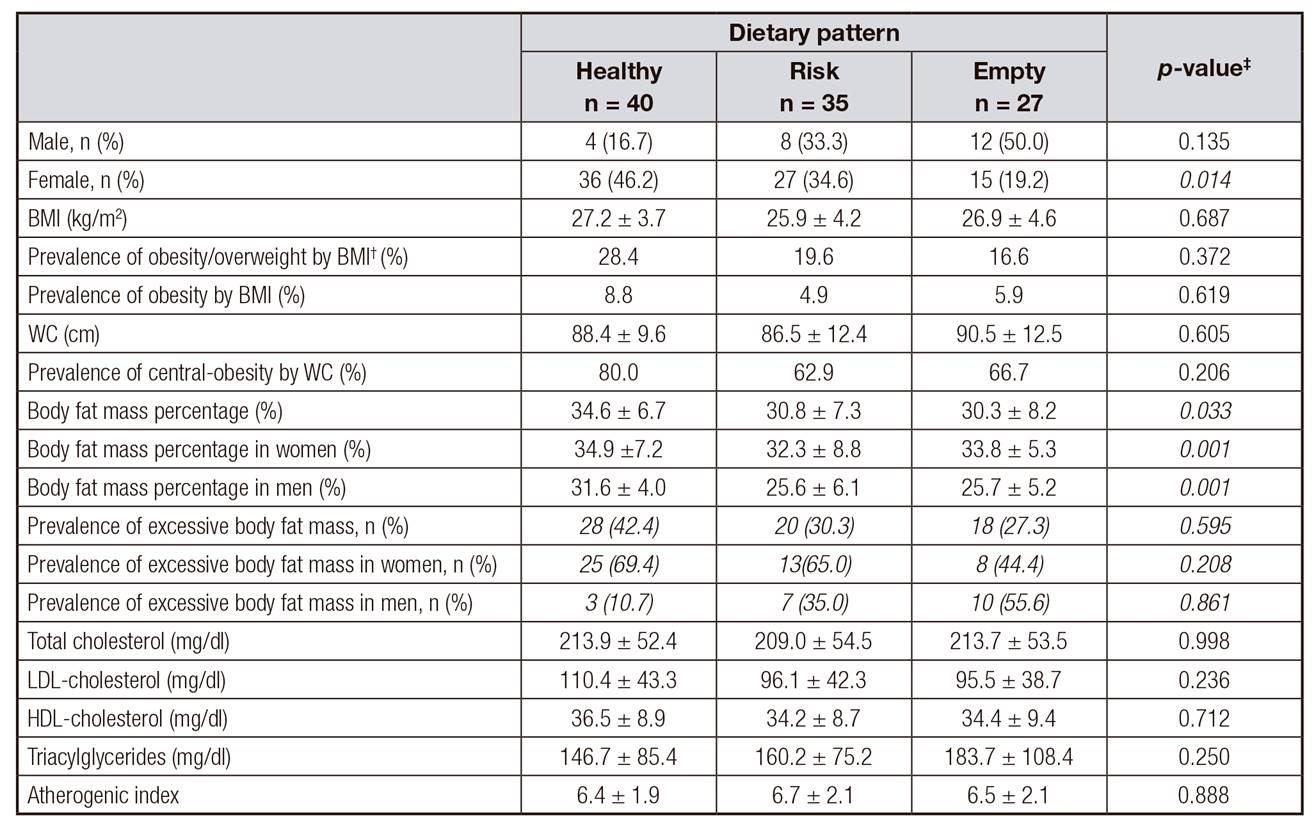
BMI: body mass index; WC: waist circumference.*All values are mean ± standard deviation. †According to BMI overweight and obesity in the same category. ‡p-value calculated with ANOVA test, adjusted by energy intake for continuous variables; Chi-square test for categorical variables. §≥ 32% for females, ≥ 25% for males.
Even when differences were not statistically significant (p > 0.05), it is interesting to observe that according to BMI and WC, obesity/overweight, obesity, central obesity, the highest average HDL-cholesterol and lowest atherogenic index were more prevalent in adults in the healthy-DP group, but all participants had elevated averages of total cholesterol, triacylglyderides and low HDL-cholesterol concentrations.
Table V Odds ratios (OR) and 95% confidence intervals (95% CI) of the association between dietary patterns, obesity, abdominal obesity and elevated serum lipid concentrations in 102 healthy adults
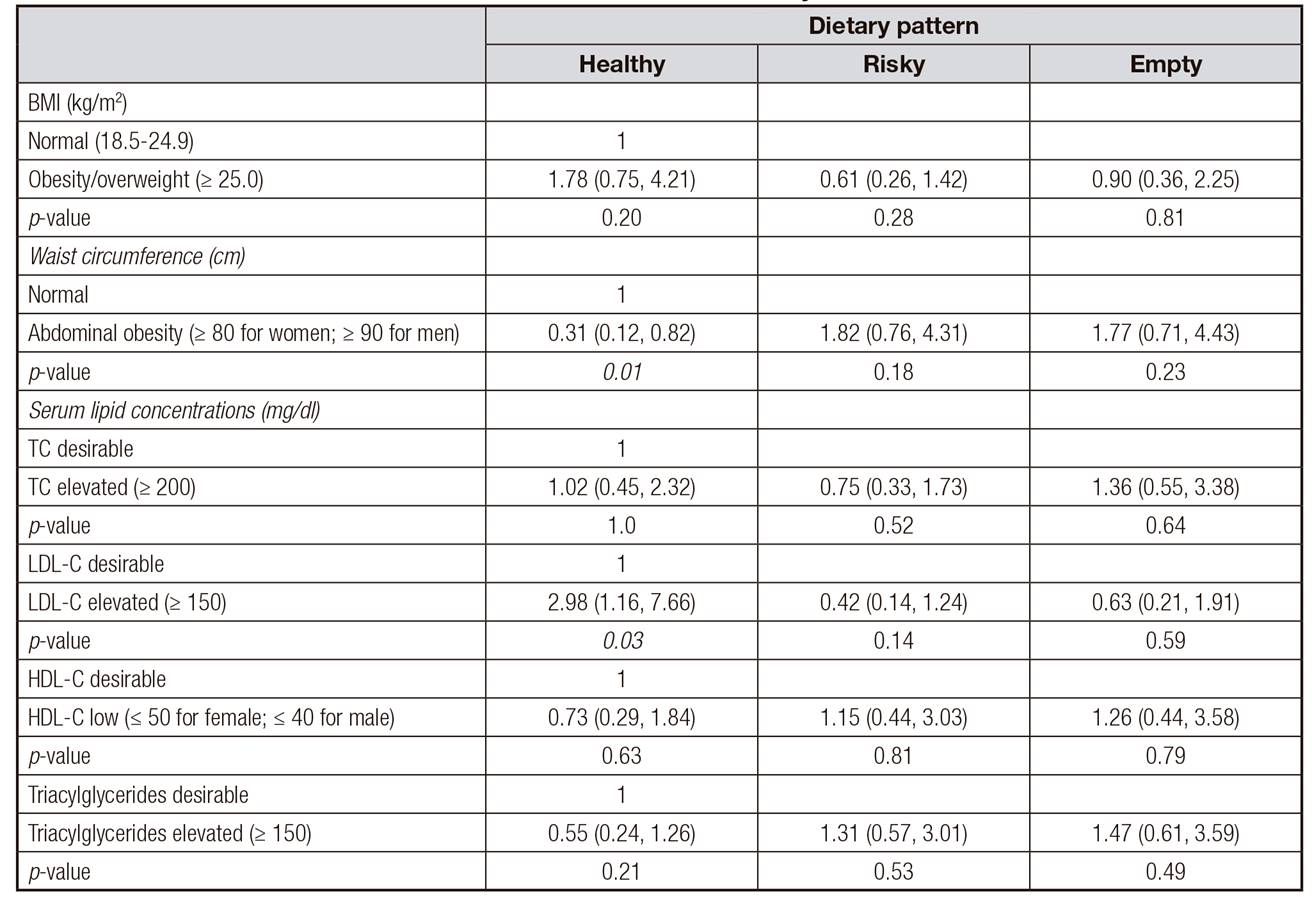
BMI: body mass index; TC: total cholesterol; LDL: low density lipoproteins; VLDL: very low density lipoproteins; HDL: high density lipoproteins; TG: triglycerides.
Finally, ordinal logistic regression is shown in Table 5. Participants in the healthy-DP group were more likely to have lower risk for central obesity according to WC criteria (OR = 0.31, CI = 0.12, 0.82), p = 0.017. Interestingly, participants in the healthy-DP group also had the highest risk for elevated LDL-cholesterol (OR = 2.98, CI = 1.16, 7.66), p = 0.030. No significant association was found between risky and empty DP with obesity or overweight by BMI, central-obesity by WC or serum lipid abnormalities.
DISCUSSION
In this study in Mexican healthy adults, three major DP were identified and their association with central obesity and serum lipid concentrations was investigated. With the use of PCA, we applied a complex epidemiological method recently used in Mexico. Clearly these three DP characterize the diet of young urban adults, describing a large variety of fresh, industrialized and traditional foods as habitual diet. It is interesting that with no differences between the three DP, consumption of dairy products is an important feature in this population, which may indicate that it is a habit derived from decades of dairy consumption, possibly due to a high availability of milk in childhood.
The first dietary pattern, which we considered as healthier because it included consumption of nuts, vegetables, fruits, cereals without fats, fish and the lowest intake of high fat meat and dairy, was associated with a low intake of cholesterol and a high intake of monounsaturated fats. The risk-DP and the empty-DP were considered as unhealthy because they had high amounts of non-recommended foods like high-fat cereals and meats, fast-foods, alcohol and sugars.
Adults from the healthy-DP group were more likely to eat less fats and to drink less alcoholic beverages, possibly in concordance with a healthier behavior. Furthermore, this healthy DP was also associated with a lower risk for central obesity in adults, although adults in this healthy-DP presented higher body fat mass. In our study, adults with higher body fat mass percentage were more likely to eat healthier, while no significant association was found regarding risk or empty DP and prevalence of obesity. This probably could be because when adults perceive they have overweight or obesity, they improve their diet; in other words, selection of healthier foods and, as a consequence, a healthier diet is perhaps the product of overweight or obesity.
Analyzing the overall diet components and combined nutrients resulted in a better way to examine dietary effects on health outcomes and a good interpretation of possible risk factors in the future. It is very important to remember that participants in this study were healthy young adults, and the importance of the dietary analysis is related to the promotion of modification of risk factors for metabolic conditions 22.
Another important finding in our results was the low consumption of fiber in all participants; even in participants of the healthy-DP group, who presented higher consumption of vegetables and fruits, the intake of dietary fiber does not cover recommendations for a healthy population 23. However, we agree with the evidence that promotes the study of all the components of the diet, rather than one of its components, particularly with respect to fruits and vegetables consumption 24. In this study, it must be noted that PCA is one of the best techniques for the extraction of dietary patterns in nutritional epidemiology 25.
With respect to the transcendence of chronic diseases related to diet, some studies mention that the nutritional epidemiological transition leads to chronic diseases as the growing epidemic obesity in Latin America 26,27. From the perspective of public health, obesity represents the most important challenge. In Mexico, the total cost of overweight and obesity and their indirect costs are estimated to reach 150.860 billion pesos (8.122 billion dollars) for 2017 28.
The imbalance in the diet is crucial to the development of obesity, especially the high consumption of fats and sugars, comprised in the risky-DP group in our study, which is similar to previous findings 29,30,31,32.
Likewise, associations between high consumption of risky or empty foods with metabolic disorders such as hypercholesterolemia and hypertriacylgliceridemia had been described previously 33,34, and similarly with our results, despite not having found significant associations, abnormal concentrations of total cholesterol and triacylglycerides were observed in apparently healthy subjects. In this regard, McNaughton et al. have reported that a high intake of white bread, chips, sugar in hot-beverages, hamburgers and soft drinks and a low intake of vegetables are associated with an increase in serum total-cholesterol, triacylglycerides and low concentration of HDL-cholesterol 35. These are conditions that, unless they are modified, could lead to the development of obesity as well 34,36,37.
On the other hand, we found in this study a healthy-DP integrated with food groups such as fruits and vegetables considered a prudent or healthy-DP as in other studies, which have been linked to the prevention of chronic diseases such as obesity, diabetes, hypertension and cancer 34,38,39,40. These could be used for the assessment of diet quality in future studies, or in interventions to modify risk factors such as diet.
CONCLUSIONS
In this sample of Mexican adults, three DP were identified: a healthy-DP, a risk-DP and an empty-DP. The healthy-DP was associated with a low risk of central obesity. Our results confirm that higher intakes of vegetables, fruit, lean protein, nuts and lower intakes of dairy and alcohol are likely beneficial for the prevention of central obesity, but not for desirable lipid concentrations.














