BACKGROUND
A balanced diet has been proved to improve people's current and future health (1,2). Correct dietary intakes become even more important during diseases and consequently during hospitalisations (3,4). The prevalence of patients at risk of malnutrition can reach up to 50 % in the hospital setting; these patients should be first identified and then treated (5,6).
When faced with a patient at risk of malnutrition, or malnourished, or who cannot adequately cover energy/protein needs, physicians should evaluate the best intake and, if necessary, introduce artificial nutrition (7,8).
Previous studies have found that invasive (enteral or parenteral) artificial nutritional therapies were not always indicated or correctly prescribed (5,9). This has a negative impact at the level of both increased iatrogenic complications and costs (10). Continued re-evaluation of the adequacy of invasive therapies is also supported by the global campaign Choose Wisely, even though there are no strong recommendations in this specific field (11).
In the literature, the few data available, with weak evidence, would seem to reveal a favourable impact of the introduction of a dedicated Clinical Nutrition and Dietetic Service on the use of artificial nutrition considering all services of a hospital (12).
In this study, we illustrate how nutritional therapy has changed within our hospital after the introduction of a dedicated Clinical Nutrition Team, as a point of reflection for new research in this regard.
METHODS
STUDY DESIGN AND PARTICIPANTS
The single-centre, retrospective, observational study took place at the Regional Hospital of Locarno, Switzerland. This public hospital is equipped with services for Intensive Care, Internal Medicine, General and Trauma Surgery, Gynaecology, Obstetrics, and Paediatrics.
The study descriptively describes the evolution of nutritional therapy from 2014 to 2019.
Since mid-2017, the hospital has been equipped with a Clinical Nutrition and Dietetic department supporting physicians in the management of patients with nutritional issues, including malnourished patients and patients forced to fast after surgery. This support is to be considered a non-binding consultation for clinicians, who remain in charge of patient care in full decision-making and therapeutic autonomy.
DATA SOURCE
The data reported, such as the total number of patients and the proportions of malnutrition diagnoses, were provided by the Finance and Controlling Service of the hospital. These data are regularly provided to the managers of the Clinical Nutrition and Dietetic Service to monitor their progress. The diagnosis of malnutrition is reported in the patient's exit letter, thus encoded at the end of the hospital stay, according to the SWISS-DRG rules (13). Data concerning the products used for artificial nutrition were provided by the hospital pharmacy. We report the volume of products used for enteral nutrition and the total number of bottles of oral nutritional supplements (ONS). Data on the amount of maltodextrin or protein powder used in the kitchen for the enrichment of the basic diet are not available.
NUTRITIONAL TEAM
In the years preceding the introduction of the Clinical Nutrition and Dietetic Service, the hospital had a dietary service composed of 2.7 units of dietitians, who were called in case of need by physicians.
From 01JUN2017 a real Clinical Nutrition and Dietetic Service was created, composed of a medical unit (a doctor) at the head of the team and dietitians. The aim was to improve the management of malnourished patients and improve nutritional counselling in general.
With the introduction of the Clinical Nutrition and Dietetic Service, the application of malnutrition screening tools improved by using the Nutritional Risk Screening (NRS-2002), a tool recognised by the European Society for Clinical Nutrition and Metabolism (ESPEN) (4,14). Before 2017 the NRS-2012 was carried out in paper format, while with the introduction of the Clinical Nutrition and Dietetic Service it was integrated into the computerised and semi-automated medical record. In contrast, the elaboration process remained unchanged: the first part is carried out by nurses, the second part by physicians.
In practice, the three questions and parameters (weight and height) measured and/or asked when not obtained by the screening tools were made mandatory and have become an integral part of the compulsory admission nursing history. With this device we were able to apply screening systematically in the first 24-48 hours to all patients who are hospitalized.
If any of the four items resulted pathological, a red alert would appear in the patient's diagnosis list. The patient's physician, by activating the alert message, could gain access to the second part of the screening procedure. If the score exceeded three points, the patient was deemed to be “at risk of malnutrition”, directly starting a request of consultation by the Clinical Nutrition and Dietetic Service.
In addition, the Clinical Nutrition and Dietetic Service provided training sessions for physicians and nurses, in addition to the usual bedside teaching during consultations.
RESULTS
The number of patients who were treated by the hospital remained more or less constant from 2014 to 2019: on average 7,544 pts/year (CI, 7,364-7,735) (Table I). The percentage of patients with a malnutrition diagnosis reported in the exit letter increased over the years from 1.6 % (117 patients) in 2014 to 9.2 % (703 patients) in 2019 (+ 501 %). The greatest increase occurred after 2017: + 2.35 % from 2015 to 2016, + 3.4 % in 2017, + 5.5 % in 2018, + 9.2 % in 2019, respectively. There was a net increase, in fact a doubling, in annual consultations starting from 2017, the year following the introduction of the Clinical Nutrition and Dietetic Service (from about 1,666/year in 2016 to 3,212/year in 2019) (Table I).
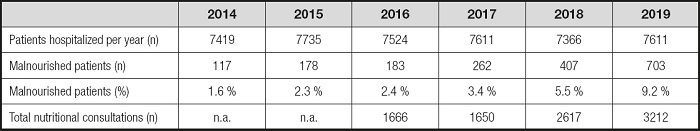
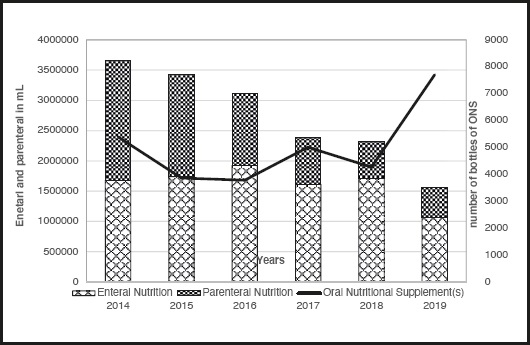
Table II shows the details about the artificial nutrition used. The amount of total parenteral and enteral artificial nutrition used decreased steadily from 3,660,250 ml in 2014 to 1,560,750 ml in 2019 (- 57 %) (Table II and Figs. 1 and 2).
Table II. Consumption of artificial nutrition.
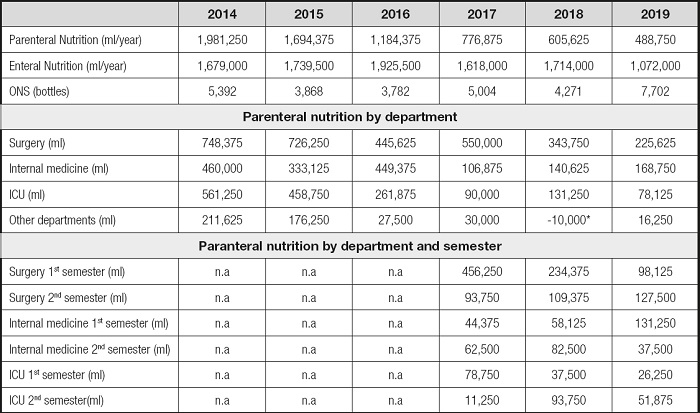
ONS: oral nutritional supplement(s); n.a: not available; ICU: intensive care unit.
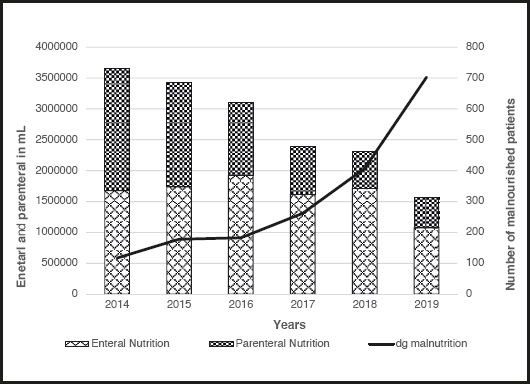
Figure 2. Evolution of artificial nutrition (parenteral and enteral) over the years in relation to the number of malnourished patients.
The volume of parenteral nutrition used steadily decreased from a maximum of 1,981,250 ml in 2014 to a minimum of 488,750 ml in 2019 (- 75 %). The reduction started already in 2015, but since 2017 there was a net decrease in the prescription of parenteral nutrition in the Internal Medicine and Intensive Care departments. In Internal Medicine, the average annual utilisation dopped by 44 % after the introduction of the Clinical Nutrition and Dietetic Service. For Intensive Care, we observed a 75.5 % decline. The same trend was observed also in other departments (gynaecology, haemodialysis).
The Surgery Department had a steady reduction over the years. However, the largest drop started from the second half of 2017, where it changed from 456,250 ml to 93,750 ml (Table II and Fig. 3).
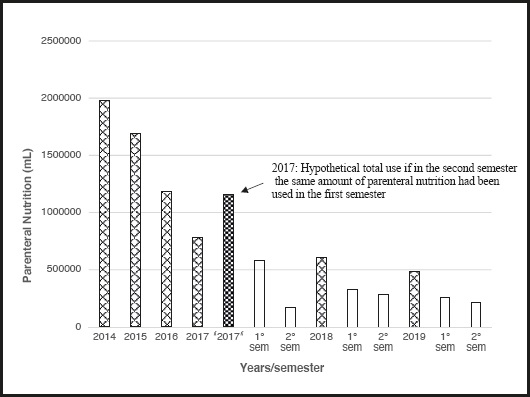
Figure 3. Evolution of parenteral nutrition over the years, divided by semester after 2017 (introduction of the Clinical Nutrition and Dietetic Service mid-2017).
Enteral nutrition consumption tended to rise in the two-year period 2014-2016, then fluctuated and finally collapsed in 2019. Between 2014 and 2019, we observed a reduction in enteral nutrition by 36 % (from 1,679,000 ml to 1,072,000 ml). The use of ONS remained more or less constant until 2018, when there was a sudden increase (+ 80 %) (Table II).
DISCUSSION
Over the years, we witnessed the introduction of a Clinical Nutrition and Dietetic Service in many hospitals, to help manage the problems related to nutrition. In certain countries, the creation of Clinical Nutrition and Dietetic Services is imposed by the legislation (15). This is because its efficacy and usefulness are increasingly supported by the literature, although data are often limited to specific departments and do not consider the whole hospital reality (16). As malnutrition is a very frequent problem in hospitalized patients and is associated with an increase in morbidity-mortality, its recognition and treatment are essential (7). The updated systematic review and meta-analysis of Gomes F et al. clearly demonstrates that the treatment of these patients improves their prognosis (17).
Our analysis demonstrates that with the introduction of the Clinical Nutrition and Dietetic Service the number of patients identified as being malnourished increased significantly. The integration of the nutritional risk screening in the computerised medical record certainly helped improve the process of screening. This certainly played a role, but it is not the only one, since we observed some differences between services, with the largest improved in the identification of malnourished patients in the Internal Medicine service. Since the screening tool was the same in all services, the hypothesis is that internists has first integrated the importance and usefulness of recognising and taking care of the patient at risk of malnutrition, after the various trainings in this regard, as compared to surgeons and physicians of other specialities. We must note that unfortunately there is still a “long and winding road” to go until malnutrition is identified in every inpatient. The increase in the number of patients recognised as having a nutritional problem led to a net increase in the consultations performed.
The impact of the Clinical Nutrition and Dietetic Service on the use of artificial nutrition is not well understood and described in the literature. Previous studies have focused on assessing the appropriateness of prescriptions for artificial nutrition, mainly parenteral nutrition, with prescription inadequacy up to a rate of 37 % of cases (5,18). Other studies have focused on the potential for economic savings achieved by both reducing the use of artificial nutrition and reducing the morbidity of patients at risk of malnutrition with an appropriate treatment (5,19,20).
In our retrospective analysis, we observed a decrease in parenteral nutrition over the years (Fig. 1), a decrease that occurred indistinctly in all services. The decline in Internal Medicine and Intensive Care Unit was clearly accentuated starting from 2017, the year of introduction of the Clinical Nutrition and Dietetic Service.
We can only speculate that the decline in parenteral use is the result of a more individualised patient care and optimisation in the use of less invasive nutritional strategies (enrichment of the basic diet, ONS, enteral nutrition). Indeed, in 2019, that is, after 1.5 years from the introduction of the Clinical Nutrition and Dietetic Service, we observed a net decrease in invasive nutrition in favour of ONS. These are pre-packaged industrial oral supplements that the Nutritional Team often propose to accompany individualised diet regimens: supplementation of the regimen chosen for the patient's profile, adapted to the desired consistency and directly integrated in the kitchen with maltodextrin and/or proteins. The 2020 year analysis would have definitely been useful and would have allowed, 3 years after the introduction of the Clinical Nutrition Service, to confirm the trend detected. Unfortunately, with the arrival of the COVID-19 pandemic, the Hospital of Locarno has become a COVID centre and therefore the data are no longer comparable, as the patient case series has completely changed (21).
The net increase in consultations was achieved with an only modest increase in human resources (physician employed at 50 %). Therefore, even from a financial perspective, the Clinical Nutrition Service allows direct financial savings with less product purchase and indirect savings, as demonstrated in previous studies, reducing both iatrogenic complications related to invasive artificial nutrition and lowering the costs generated by the correct treatment of malnourished patients, who present fewer complications (5,17,18). Furthermore, the investment for the creation of the Clinical Nutrition Service is often relatively modest, as in most hospitals dietitians are already staff members and should only be re-inserted into a multidisciplinary clinical unit. Integration which, as our case teaches, can take place without conflicts.
Last but not least, indirectly, the improvement in the report in the outgoing letter of the malnutrition diagnosis can translate into increased hospital repayment for hospitalization.
We are aware of the weakness inherent to the retrospective study design: we cannot indeed not demonstrate that the observed changes traduce in improved patient care/prognosis.
We also recognise that other factors occurred in the long time lapse of six years may have influenced the reported results. In order to increase the authoritativeness of the results, we would need future study protocols with strong clinical endpoints, such as morbidity and mortality, endpoint with impact on DRG.
By supporting the Choose Wisely campaign, in light of the possibility of decreasing invasive nutrition without apparently negative repercussions, we hope that other physicians will join the campaign of continued revaluation of inappropriate or potentially harmful medical practices.