Introduction
Vitamin D deficiency is a worldwide public health problem, since nearly 1000 million people have the condition (Holick, 2017) and it affects a considerable number of women during pregnancy and lactation (Sánchez, 2010). Previous studies have indicated that in the United States up to 50% of pregnant women may be deficient in vitamin D (Mulligan, Felton, Riek, & Bernal-Mizrachi, 2010), while in some European countries the figure is between 10% and 30% (Bodnar et al., 2007; (Holick, 2017; Johnson, Wagner, & Hulsey, 2011).
Vitamin D plays an important role in cell differentiation, immune response and fetal growth and development (Boullion, Verstuyf, Branisteanu, Waer, & Mathieu, 1995). Vitamin D deficiency (<50 nmol/L) has been related to problems in both the pregnant woman (pre-eclampsia and gestational diabetes) and the child (lower birth weight and lower head circumference at birth, small for gestational age, preterm birth, etc.) (Amegah, Klevor, & Wagner, 2017; Wei, Qi, Luo, & Fraser, 2013). In studies with animal models, changes in the morphology and physiology of the offspring's brain as a result of vitamin D deficiency during pregnancy have also been observed (Eyles, Brown, Mackay-Sim, McGrath, & Feron, 2003).
The results of a prospective cohort study (INMA) conducted in 4 populations in Spain (Sabadell, Valencia, Asturias and Gipuzkoa) indicate that vitamin D levels <50 nmol/L during pregnancy are associated with lower scores on the index of mental and motor development in children at 14 months (Morales et al., 2012). And recent research in Australia shows that 19.6% of children whose mothers were deficient in vitamin D had lower language development at 4 years of age (Gould et al., 2017). In the same study it was also observed that higher levels of vitamin D in the umbilical cord were associated with an increase in the child’s language level.
Nevertheless, current research into the effect of vitamin D deficiency during pregnancy is limited and there is not enough scientific evidence to confirm its effect on the child’s neurodevelopment. A recent systematic review evaluated the effect of maternal vitamin D deficiency on the development of different psychological alterations in the offspring. It covered 9 studies involving animals and 10 involving humans and included a wide range of age groups (from lactation to adulthood). One of the studies conducted on humans assessed the relationship between vitamin D deficiency and cognitive, motor and psychological disorders (hyperactivity, autism and depression) (Pet & Brouwer-Brolsma, 2016). However, the lack of homogeneity among the studies included in the review, with different ages and different diagnostic approaches, prevented the authors from coming to any definite conclusions, although they did suggest a possible relationship between maternal vitamin D deficiency and language deficits and the appearance of autistic spectrum disorders in the child.
Concentrating on the effect that vitamin D deficiency during pregnancy may have on neurodevelopment in childhood, our objective is to carry out a systematic review of the literature that focuses on this area. Our hypothesis is that maternal vitamin D deficiency could indeed have a negative impact on the child’s neurodevelopment.
Methods
Search strategy
The studies selected were identified via a systematic review of the scientific literature published in PubMed/MEDLINE, Scopus and Cochrane until January 2018. The search strategy was to follow these keywords: ("Vitamin D") Mesh (OR "Ergocalciferols") Mesh (OR "Cholecalciferol") Mesh (OR "Calcifediol") Mesh(OR "24, 25-Dihydroxyvitamin D 3") Mesh (OR "25-Hydroxyvitamin D 2") Mesh() AND (“pregnancy” OR “pregnant” OR gesta*) AND ("Infant, Newborn") Mesh (OR "Infant") Mesh (OR “neonates” OR “birth outcomes” OR "Pregnancy Outcome")Mesh() AND (“neurodevelopment” OR "Neurobehavioral Manifestations" OR "Neurodevelopmental Disorders" OR "Cognition" OR “cognitive function” OR “neuropsychological development” OR “motor” OR "Behavior" OR "Infant Behavior" OR "Mental Disorders" OR "Psychomotor Performance" OR “motor development” OR “mental development” OR “cognitive development” OR “infant development”). A manual search was also carried out for articles in the bibliographies of other studies. Comments and editorials were excluded, while systematic reviews and meta-analysis were used to cite some studies.
Inclusion and exclusion criteria
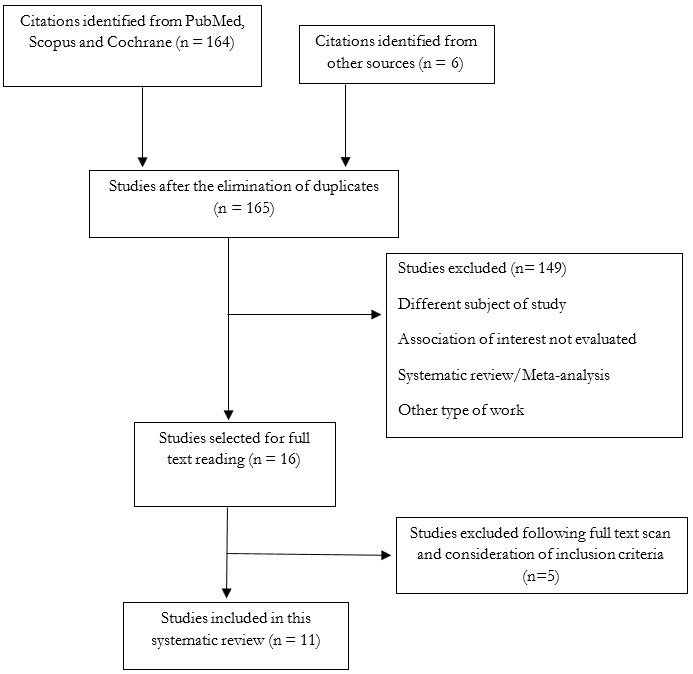
The studies were filtered by title and abstract and repeated publications were excluded (Figure 1). We explored studies that linked the maternal status of vitamin D with the neurodevelopment of the child. The inclusion criteria were as follows: a) Vitamin D concentrations measured in serum or plasma during pregnancy or in the umbilical cord at delivery, and b) infants, preschool and school children. The exclusion criteria were: a) pregnant women with chronic diseases, and b) adolescent women.
From each article selected we extracted the following information: author, year of publication, design of the study, geographical location, cut-off point for vitamin D, gestational age at the time the blood sample was taken, laboratory method used to measure vitamin D concentrations, age, domains assessed and neurodevelopmental assessment test.
Encoding of the variables and instrumentation
Two of the authors conducted their own independent literature searches of the different electronic databases and the degree of agreement was verified. The purpose of this was to analyze the reliability of the selection process.
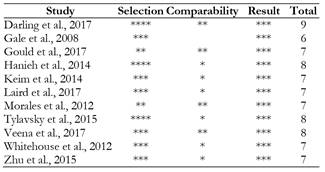
The quality of the observational studies was assessed using the Newcastle-Ottawa scale, as recommended by the Cochrane Non-Randomized Studies Methods Working Group. The score is based on three items: selection (maximum 4 stars), comparability (maximum 2 stars), and results (maximum 3 stars). Studies that scored between 7 and 9 were considered to be of high methodological quality, between 4 and 6 moderate, and less than 4 low (Wells et al., 2014).
Results
From the databases we identified 164 articles that fulfilled the inclusion criteria, from which 11 were finally selected. The articles reviewed were published between 2008 and 2017 and, although they varied as regards some of the characteristics relating to their methodology, they all examined the relationship between maternal vitamin D levels and neurodevelopment in children.
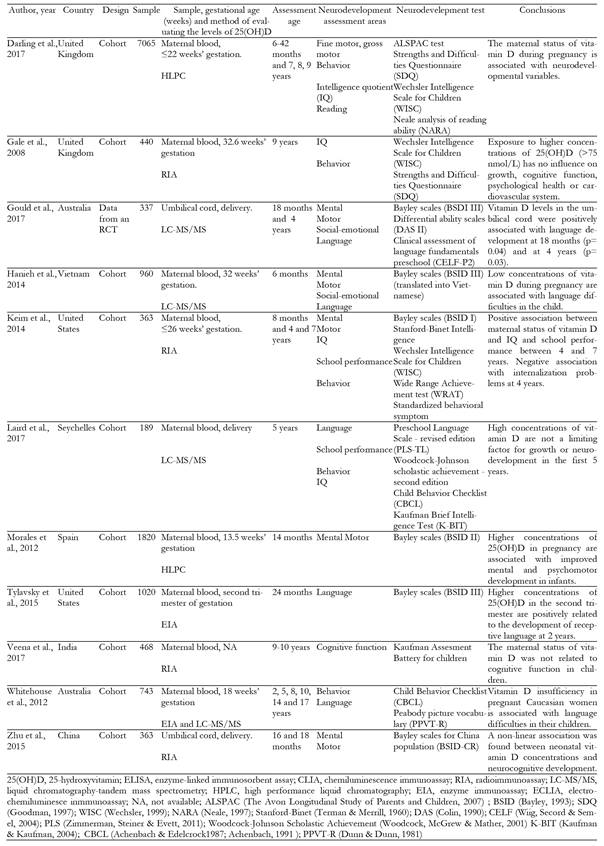
Table 1 presents the characteristics of the studies selected for this review. We included eight studies conducted in developed countries - two in the United States (Keim, Bodnar, & Klebanoff, 2014; Tylavsky et al., 2015), two in Australia (Gould et al., 2017; Whitehouse et al., 2012), two in the United Kingdom (Darling et al., 2017; Gale et al., 2008), one in Spain (Morales et al., 2012) and one in China (Zhu et al., 2015) - and three conducted in developing countries: Vietnam, India and the Republic of Seychelles (Hanieh et al., 2014; Laird et al., 2017; Veena et al., 2017).
There were ten observational cohort studies (Darling et al., 2017; Gale et al., 2008; Hanieh et al., 2014; Keim et al., 2014; Laird et al., 2017; Morales et al., 2012; Tylavsky et al., 2015; Veena et al., 2017; Whitehouse et al., 2012; Zhu et al., 2015), whereas only one study originating from a clinical trial was found (Gould et al., 2017).
In eight studies the neurodevelopment of the child was assessed during infancy and the preschool stage (Darling et al., 2017; Gould et al., 2017; Hanieh et al., 2014; Keim et al., 2014; Morales et al., 2012; Tylavsky et al., 2015; Whitehouse et al., 2012; Zhu et al., 2015), while in seven studies it was assessed during the school-age stage (Darling et al., 2017; Gale et al., 2008; Gould et al., 2017; Keim et al., 2014; Laird et al., 2017; Veena et al., 2017; Whitehouse et al., 2012)
Six studies assessed mental development (Gould et al., 2017; Hanieh et al., 2014; Keim et al., 2014; Morales et al., 2012; Veena et al., 2017; Zhu et al., 2015), six studies motor development (Darling et al., 2017; Gould et al., 2017; Hanieh et al., 2014; Keim et al., 2014; Morales et al., 2012; Zhu et al., 2015), two social-emotional development (Gould et al., 2017; Hanieh et al., 2014), five language development (Darling et al., 2017; Gould et al., 2017; Hanieh et al., 2014; Tylavsky et al., 2015; Whitehouse et al., 2012) and five IQ (Darling et al., 2017; Gale et al., 2008; Keim et al., 2014; Laird et al., 2017; Veena et al., 2017).
Quality evaluation
According to the score obtained in the Newcastle-Ottawa scale, ten observational studies were considered to be of high methodological quality, while only one was of moderate quality (Table 2).
Discussion
This systematic review comprises eleven cohort studies (ten of a high methodological quality and one moderate) that assess the impact of vitamin D levels during pregnancy on the neurodevelopment of the child. The results indicate that vitamin D levels <50 nmol/L during pregnancy have a negative effect on the child’s neurodevelopment, with language being one of the domains most affected.
Most of the studies (81%) were carried out in developed countries and 88% evaluated the effects of maternal vitamin D levels on neurodevelopment during lactation and the preschool stage.
Vitamin D status during pregnancy
The prevalence of pregnant women with vitamin D deficiency (<50 nmol/L) in the studies reviewed ranged between 19% and 49% depending on the characteristics of the population. In a recent study conducted in the US, pregnant women had an average vitamin D concentration below the limits considered sufficient (45 nmol/L) (Keim et al., 2014), while in another study the prevalence of vitamin D deficiency was 42% (Tylavsky et al., 2015). Two studies conducted in the United Kingdom found a similar prevalence of vitamin D deficiency in pregnant women, one being 41% (Darling et al., 2017) and the other 47% (Gale et al., 2008). In Spain this deficit was much lower at 19% (Morales et al., 2012), while in Australia it ranged between 42% (Gould et al., 2017) and 25% (Whitehouse et al., 2012). In Asia the highest prevalence of insufficiency was between 60% and 62% (Hanieh et al., 2014; Veena et al., 2017). Also noteworthy was the high prevalence of children with vitamin D deficiency (78%) in China (Zhu et al., 2015), this value correlating with maternal concentrations (Maghbooli et al., 2007; Markestad, Aksnes, Ulstein, & Aarskog, 1984). Moderate exposure to the sun is the main source of vitamin D for humans (Rodríguez-Dehli et al., 2015). The season, latitude, weather, use of sunscreen, skin color and clothes all have an influence on the amount of ultraviolet rays that penetrate the skin, and thus on the synthesis of vitamin D (Holick, 2004). Dietary intake of vitamin D can also affect vitamin D levels, but there are very few foods that contain this nutrient. Geographical location, the time of blood extraction, skin color and the low intake of foods with vitamin D are possibly the factors most related to the high prevalence of vitamin D deficiency found in the studies.
Currently there is no consensus on adequate or inadequate levels of vitamin D in the general population and even less as regards during pregnancy and in the child stage. In 2010 the US Institute of Medicine defined vitamin D deficiency as being levels of 25 (OH) D <30 nmol/L (12 ng/mL), insufficiency as between 30 and 50 nmol/L (12 to 20 ng/mL) and sufficient levels as ≥50 nmol/L (≥ 20 ng/mL) (Institute of Medicine, 2010). The American Society of Endocrinology, however, defined deficiency as being levels of 25 (OH) D <50 nmol/L (20 ng/mL), insufficiency as between 52.5 and 72.5 nmol/L (21-29 ng/mL) and optimal or adequate levels as >75 nmol/L (>30 ng/mL) (Holick et al., 2011). Regardless of the proposed cut-off points, it has been observed that vitamin D levels <50 nmol/L during pregnancy are associated with an increased risk of pre-eclampsia (Wei et al., 2013), gestational diabetes (Wei et al., 2013), being small for gestational age (Santamaria et al., 2018; Wei et al., 2013) and preterm infants (Qin, Lu, Yang, Xu, & Luo, 2016; Wei et al., 2013), while levels of 25 (OH) D <30 nmol/L are associated with low birthweight (Santamaria et al., 2018).
Not all the studies in this systematic review define vitamin D deficiency at the same cut-off point. The studies carried out in Spain (Morales et al., 2012), the United States (Keim et al., 2014; Tylavsky et al., 2015), the United Kingdom (Darling et al., 2017), Australia (Gould). et al., 2017), China (Zhu et al., 2015) and India (Veena et al., 2017) used the same definition of vitamin D deficiency as the American Society of Endocrinology (<50 nmol/L), while those carried out in Vietnam (Hanieh et al., 2014), the Republic of Seychelles (Laird et al., 2017), the United Kingdom (Gale et al., 2008) and Australia (Whitehouse et al., 2012) used the cut-off point proposed by the Institute of Medicine. In some studies, the two cut-off points (<30 and <50 nmol/L) were used, and in both cases a negative impact on the child’s neurodevelopment was observed.
Association of vitamin D status with cognitive and motor development
At 6 months Hanieh et al. (2014) found no association between vitamin D levels and the mental, motor and social-emotional domains, although lower scores in language were observed. Using the same test, Keim et al. (2014) found no relationship between vitamin D levels during pregnancy and neurodevelopment at 8 months.
The observational studies included suggest that having levels of 25 (OH) D <50 nmol/L in pregnancy has a negative effect on the mental and motor development of children between 14 and 30 months. In a prospective cohort study conducted in 4 populations of Spain (Sabadell, Valencia, Asturias, and Gipuzkoa) it was observed that the children of women with vitamin D levels <50 nmol/L were disadvantaged in the score for mental and motor development at 14 months compared to the children of women with levels >75 nmol/L (Morales et al., 2012). In the study conducted in China it was found that children at 18 months with umbilical cord vitamin D levels <21 nmol/L were 7.06 points lower in the mental domain and 8.04 points lower in the motor domain compared to children with levels >40 nmol/L (Zhu et al., 2015). Both of these studies assessed neurodevelopment through the BSID II test. In the United Kingdom, Darling et al. (2017) found that deficient levels of vitamin D (<50 nmol/L) increase the risk of difficulties in gross motor development at 18 and 30 months and in fine motor development at 30 months. Unlike previous research, this study assessed motor development using the ALSPAC preschool questionnaires.
Cognitive development was assessed through IQ. In the United Kingdom, Gale et al. (2008) were the first to evaluate the association between maternal vitamin D levels and the child's IQ. This study found no association between vitamin D levels during pregnancy and IQ. However, this may have been due to the fact that the cohort in this study was small (178 mothers and children) and the results were not adjusted for confounding variables. Also in the UK, a recent study with a cohort of 7065 mothers and children found a significant association between vitamin D levels <50 nmol/L during pregnancy and verbal intelligence assessed at 8 years (OR 1.19 95% CI 1.02 to 1.39, p= 0.03). In the United States a positive association was found between maternal vitamin D levels and IQ, reading and spelling at ages 4 and 7 years, and arithmetic performance at 7 years (Keim et al., 2014). However, in this same age range a study conducted in India and another in the Republic of Seychelles found no association (Laird et al., 2017; Veena et al., 2017), and indeed the Indian study used a wider battery of neuropsychological tests. In the Republic of Seychelles study, the lack of association could be due to the fact that most of the women had sufficient levels of vitamin D.
The biological mechanisms in which a deficiency of vitamin D can affect the development of the brain are currently unknown. However, vitamin D regulates 3% of known human genes (Mizwicki & Norman, 2009), and therefore deficient levels could affect the expression process of genes that code for proteins that control motor and cognitive function. In a recent systematic review of animal models, it was observed that genetic expression (of genes that code for proteins involved in synaptic plasticity) is affected in the offspring of mothers exposed to a deficiency of vitamin D (Pet & Brouwer-Brolsma, 2016). In addition, a change in 1,25 dihydroxyvitamin D3 can play a part in motor development through the dopaminergic pathway. Experimental models in rats suggest that vitamin D plays an important role in dopaminergic systems (Pet & Brouwer-Brolsma, 2016).
Motor and executive function development (frontal parts of the brain) is related to the process of myelination (Rosselli, 1997, Rosselli 2003). Vitamin D, as a neuroactive steroid, plays an essential role in myelination, which is important for brain connectivity (Wang et al., 2016). The process of myelination begins three months after conception, although few areas of the brain are myelinated at birth. A deficiency of vitamin D during pregnancy could probably interfere with the beginning of this process and make maturing more difficult at later ages. This is a complex process and one that could also be affected by deficiencies of other nutrients during pregnancy.
Only two studies found a relationship between vitamin D levels during pregnancy and IQ. One possible explanation could be the origin of the studies included in the present review. Those that showed no relationship were carried out in developing countries, where deficiencies of micronutrients rarely occur in isolation. In most undernourished populations, several nutrient deficiencies (iron, folate, copper, zinc, vitamin A, B12, etc.) that affect brain development are also likely to be present, and so it is difficult to determine which nutrient is responsible for the particular effects studied. Another possible mechanism that is believed to influence the delay of certain cognitive abilities is intrauterine growth retardation, e.g. a lower cephalic circumference at birth. Several studies have shown that children of mothers with deficient levels of vitamin D (<30 nmol/L) have a lower cephalic circumference compared with children of mothers with higher levels (Eckhardt et al., 2015; Morley et al., 2006).
Association of vitamin D status with language development
Hanieh et al. (2014) found a lower score on the language scale (BSID III) in children at the beginning of language development (6-month-old infants) when their mothers had vitamin D levels <37.5 nmol/L during pregnancy. In the United States, Tylavsky et al. (2015) assessed language development at 2 years (BSID II) and observed that the children of mothers with vitamin D levels <50 nmol/L had lower scores in receptive and expressive language compared to those with levels >75 nmol/L. In the study conducted in Australia in 2012, it was observed that the children of women with vitamin D levels <37 nmol/L had up to twice the risk of being categorized as having severe language difficulties compared to the children of women with levels >75 nmol/L (OR 2.04 95% CI 1.14 to 3.68), although after adjusting for confounding variables the increase in risk was similar for both groups (OR 1.92 95% CI 1.01 to 3.62) (Whitehouse et al., 2012). A recent study in the same country found that an increase of 10 nmol/L in vitamin D levels in the umbilical cord is associated with an increase of 0.6 points in the language scale at 18 months as assessed by BSID III, and an increase of 0.67 points at 4 years as assessed by CELF-P2 (Gould et al., 2017).
In short, there are many studies that seem to observe a negative impact on language development in children whose mothers had low levels of vitamin D during pregnancy. The development of language depends on the affective and intellectual relationships of the child, and the learning processes and the maturing of the anatomo-functional structure. Deficient vitamin D exposure in the uterus may affect development of the perisylvian structures responsible for language (Binder et al., 1997), which are those affected in children with language development difficulties (Webster et al 2004, Whitehouse et al., 2008). In animal models it has been observed that a deficiency of vitamin D during pregnancy can affect the morphology and physiology of the brain (Pet & Brouwer-Brolsma, 2016). In addition, a study in mice showed a reduction in volume of the lateral ventricle of the brain and the expression of genes involved in neuronal survival, such as the brain-derived neurotrophic factor (BDNF), the transforming growth factor β1 (Tgf- β1) and the Foxp2 protein (Forkhead box protein P2). People with a single functional copy of the transcription factor encoded by this gene have other difficulties in language (learning and control of speech movements) (Gaceta Médica, 2014).
It is known that perisylvian structures including the temporal plane, the triangular portion and the inferior frontal gyrus of the brain develop during the second and third trimesters of pregnancy (Quarello, Stirnemann, Ville, & Guibaud, 2008). However, not all studies that assess language development measure vitamin D levels during this period. Two of those reviewed measure vitamin D during the second trimester (Tylavsky et al., 2015, Whitehouse et al., 2012), one during the third trimester (Hanieh et al., 2014) and one during delivery via the umbilical cord (Gould et al., 2017). It may be that studies that measure vitamin D during the third trimester or at the end of the pregnancy do not reflect vitamin D levels in the early stages of pregnancy.
Association of vitamin D status with behavior
In studies that assessed behavior and its relationship with vitamin D levels during pregnancy, no association was found. In the United States, Keim et al. (2014) found that the children of mothers with the highest levels of vitamin D have a lower risk of internalization problems at 4 years. Although no consistent results have been observed regarding the relationship between vitamin D deficiency during pregnancy and behavior, it has been seen that low levels of vitamin D can affect the production of serotonin. Vitamin D is known to activate transcription of the gene that synthesizes serotonin in the brain (tryptophan hydroxylase 2) and affects the production of serotonin in peripheral tissues (Patrick & Ames, 2014). However, it is difficult to determine whether a deficiency during pregnancy can affect behavior or the risk of psychopathology during early stages due to the wide variety of factors that explain a child's behavior (genetic factors, prenatal environment, family, social and other environments, individual and environmental factors).
Strengths and limitations
A wide search strategy was followed for studies on the relationship between vitamin D status during pregnancy and neurodevelopment in children. No restrictions regarding the year of publication were made during the inclusion process, and therefore this systematic review gathers together all the information published to date on the subject of study. In order to control the risk of bias and ensure the results were reliable, the methodological quality of each study was evaluated. However, the different methodologies used in this type of study - such as the laboratory method to quantify vitamin D, different cut-off points for vitamin D, the trimester of pregnancy and time of year in which maternal blood was extracted, the different ages at which psychological assessments were carried out and the different batteries of neuropsychological tests applied - may influence whether or not consistent results are obtained and thus become a limitation.
It is well known that vitamin D concentrations are lower in spring and in winter and also that blood extraction in a particular semester does not reflect the state of vitamin D during the entire pregnancy. Also, in the various studies included in this review, different neurodevelopmental domains have been evaluated at different stages (lactation, preschool and school), and this makes it difficult to interpret the results. It is suggested that studies should be conducted to control for these factors in order to obtain a clearer view of the impact of maternal vitamin D deficiency on the child's neurodevelopment.
Conclusions
Although research into how vitamin D status during pregnancy affects children’s neurodevelopment is still scarce, the results of this review suggest that low levels of vitamin D have a negative impact on neurodevelopment during the infancy, preschool and school stages, mainly as regards the development of language. The children of mothers with higher levels of vitamin D have better scores in different neurodevelopmental tests. Nevertheless, these results should be interpreted with caution since they are based on evidence from observational studies with possible confounding factors. Suggested areas for future research (trial studies) include understanding how the maternal deficit of vitamin D can affect the child’s brain development and the ideal cut-off point for vitamin D during pregnancy so as to avoid a negative effect on brain development.











 texto en
texto en