Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Avances en Odontoestomatología
versión On-line ISSN 2340-3152versión impresa ISSN 0213-1285
Av Odontoestomatol vol.23 no.6 Madrid nov./dic. 2007
Ameloblastoma of the jaw and maxillary bone: clinical study and report of our experience
El ameloblastoma del hueso maxilar y mandibular: un estudio clínico basado en nuestra experiencia
Di Cosola M.*, Turco M.*, Bizzoca G.*, Tavoulari K.*, Capodiferro S.*, Escudero-Castaño N.**, Lo Muzio L.***
* Department of Dentistry and Surgery, University of Bari, Italy.
** Departament of Oral Medicine and Bucofacial Surgery, Complutense University of Madrid, Spain.
*** Department of Oral Pathology, University of Foggia, Italy.
Receibed: Febrero 2007.
Acepted for publication: Marzo 2007.
SUMMARY
In order to ameloblastoma´s cases series, benign tumour of epithelial origin, we will value the histological and radiographic common findings, its frequent symptomatology, and we will estimate the prevalence variation according to the age, gender, lesion localization, etc.
In the other hand, we will emphasize the principal risk factors and we will classify the different treatment according to its histology, clinic and type of lesion.
Key words: Solid-multicystic ameloblastoma, unicystic ameloblastoma.
Introduction
The ameloblastoma is a relatively rare dental tumor, described for the first time by Broca in 1868, and so denominated by Churchill in 1934.
According to Larsonn and Almeren (1), its incidence is 0,6 cases per million, while Shear and Singh (2) found an incidence of 0.31 cases per million in a white population of Witwatersrand in South Africa. Between 1975 and the beginning of the 80, the concept that the ameloblastoma exists in three different clinical/histopatological forms was accepted (3-4): solid-multicystical, unicystical and peripheral.
Reichart and Philipsen (5), in an analysis of the three previously mentioned entities, state that the average age of the patients with ameloblastoma is 36 years. Gardner critesizing such review( 6), calculated a 39 year-old average age for the solid multicystic ameloblastoma, 22 for that unicystic ameloblastma and of 51 years for the peripheral ameloblastoma. Equal incidences have been found in the two sexes by Reichart.
Material and methods
Ten cases (10) of ameloblastoma were identified in the department of Dentistry and Surgery of the University of Bari-Italy between 1990 and 2006. They were evaluated and classified clinically, histologically and radiographycally, based on the cytological criteria of Vickers and Gorlin (21) and World Health Organization (25) guide lines.
The clinical-pathological data was evaluated: age, sex, site and dimensions of the lesion, primary and secondary symptoms and radiographic aspects and characteristics. Furthermore the possible presence and entity of recurrence in relationship to the histological nature of the lesions was examined. The size of the tumor was measured from the panoramic radiograph and the greater mesio-distal and apico-occlusal diameters were recorded.
We also considered the type of treatment, results in relationship to the hystological, clinical and pathological criteria of the various types of lesion, with a follow-up ranging from 1 to 15 years.
Results
Frequency
10 cases of ameloblastoma were identified during this study. According to the hystological classification (25) we found: 8 solid-multicystic, 2 unicystic.
Age and gender: The average age of all the patients, during the diagnosis, was 39.6 years. The male/female relationship calculated for the whole group was 1,3:1, for the solid ameloblastomas 1,4:1 and 1,25:1for the unicisticis ameloblastomas.
All the patients were of Caucasian race and of Italian nationality.
Site distribution
9 cases were located in the jaw and 1 in the upper maxilla. The ratio between the upper maxilla and jaw was 9:1. In 7 cases the ameloblastoma was located in the posterior third of the maxillary bones, including the area of the molar teeth and the structures distal to them. In 3 cases the tumor was found in the anterior and /or middle part of the maxillary bones, therefore the region in front of the first molar.
Analysing the three histological types separately we found that 7 of the 8 cases of solid ameloblastoma were located in the jaw, 1 of these in the posterior third, and 1 in the upper maxilla. All the unicystic ameloblastomas (2) were located in the posterior third of the jaw.
Size of tumor
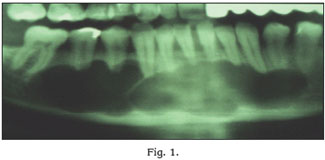
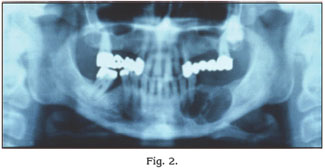
In all patients the mesio-distal dimensions were greater than 2,5 cm (Figs. 1-2-3).
Symptoms
The symptoms were recorded in all cases: in 8 patients the main symptom was a non aching swelling of the maxillary bones, 2 were accompanied by pain. In 4 cases the increase of volume of the lesion was described up until the hospitalisation; in 1 case pain was the only symptom. In 2 patients rhizolisi was observed. Paraesthesia was observed only in 1 case as a secondary symptom. In 2 cases we found the non aching ulceration of the overlying oral mucosa (Fig. 4). In 4 cases the discovery of the lesion was chance, after performing an x-ray for other medical purposes. The average time between the debut to the diagnosis was 9,7 months.
Radiographic findings
The radiographic aspect in 8 cases was multilocular and in 2 cases unilocular. In the case of maxillary ameloblastoma the opacity of the maxillary sinus was observed.
Histological findings
The histological diagnosis and the classification based on the actual criteria (25) allowed us to indentify 8 solid-multicistic amelobblastomas. The solid follicolar ameloblastoma were 4 (50%), the plessiforme 2 (25%), the acantomatosis 1 (12,5%) and the mixed 1 (12,5%). The 2 cases of unicystic ameloblastoma were recognised and classified based on the Ackerman classification into: 1 type III (50%) and 1 type II (50%).
Treatments and recurrence
The cases have been divided into 3 groups based on the clinical entity ( multicystical or unicystical) and the treatment received (conservative or radical):
— Group 1: multicystic ameloblastoma with conservative therapy, (cases from 1 to 6).
— Group 2: multicystic ameloblastoma with radical therapy, (cases from 7 to 8).
— Group 3: unicystic ameloblastoma with conservative therapy (cases from 9 to 10).
Conservative surgical therapy included enucleation, curettage, electrocautery, excision and stitching. Radical surgery also includes marginal resection, segmental or total resection of the mandible with wide margins.
The analysis of the first group (6 patients) showed 3 cases of recurrences. The average time between the treatment and the recurrences was 3,5 years (range 4 months-10 years).
2 of the 3 recurrences were treated again with conservative therapy.
In one case the treatment of the recurrence consisted in the resection of the jaw without continuity of the inferior edge and a bone autograft, which has not recurred.
In the second group of solid ameloblastomas the 2 patients were treated with radical surgery.
In this group the only case of recurrence was observed after 5 years, in spite of the resection of the jaw with solution of continuity of the inferior edge the recurrence was diagnosed and treated with a surgical extension of the borders.
The third group with unicystic ameloblastomas, is composed of 2 patients with an initial conservative treatment.
The unicystic ameloblastomas recurred in average after 3.5 years.
There was one recurrence in this group. It was possible to reconstruct the following therapeutic history: first treated with conservative therapy, recurred for the second time and a jaw resection with solution of continuity of the inferior edge was necessary but successful.
Clinical and histological factors of risk for recurrence
The first group (cases 1-6) had 3 recurrences out of a total of 6 with dimensions greater than 2 cm at the moment hospitalisation and 1 recurrences had dimensions inferior than 2 cm at the time of hospitalisation. In the second group (cases 7-8), 1 lesion out of 2 had dimensions greater than 3 cm at the hospitalisation.
In the group of the unicystic ameloblastomas (cases 9-10) the only recurrences had with dimensions greater than 3 cm at hospitalisation were observed. By each the location, in the first group we have noticed only 3 recurrences out of a total of 6 with location in the anterior and middle third of the maxillary bones, while the remainder 3 lesions were located in the posterior third recurred. In the second group there was only one lesion located in the posterior third.
In the group of the unicystic ameloblastoma, we found one recurrence located in the posterior part of the jaw.
Discussion
The ameloblastoma is statistically more frequent in the molar region and branch of the jaw, while in the maxilla it is more often found in the molar region, even if in some cases the maxillary cavity is interested.
The 80% of these cases were solid-multicystical and the remaining 20% unicystic. This data differ from Reicharts studies (5), which estimates 51% the incidence of the solid-multicystical lesion and the 49% for the unicystic. Such discrepancy can only be determined by the small amount of patients considered in our study. From the analysis of our cases an agreement emerged with Kramer and Regezi et, to the (11), we found no correlation among clinical symptoms, biological behavior and histological subtype. According to Reichart (5) the most common histological type is the follicolar lesion 50% compared to 33,9% proposed by literature.
According to Shaw and Katsikas (26) none of their cases followed chemio- or radiotherapy, which are only indicated in case of remaining tumor tissue after lesion resection or as a palliative therapy. In case of upper maxillar lesions radical resection is advised, due to the spongy osteoarchitecture of the maxilla which facilitates the diffusion of the tumor to the sinus ethmoidalis, pterygoidea fossa, temporal fossa and base of skull (21,25). In our study we had only one case of ameloblastoma located in the upper maxilla, it were treated with conservative surgery. Recurrences were encountered in the patients, that were over 65 years old, for whom this type of treatment was chosen because of the limited life span left; but for the young patients the literature suggest a conservative approach in pediatric patients.
Considering the fact that the conservative treatment of the maxillar bones offers local recurrence in100% of the cases and a 60% of mortality rate (26-28-32), it is important that the patients with this pathology have a life long follow-up with the help of computer tomography (CT) and magnetic resonance tomography (MRT). The therapy of the ameloblastoma is surgical, but it has not been established yet which is the most suitable operation. The decision to use a radical or conservative approach depends on various factors: 1) the dimensions and the location of the lesion, 2) the growth rate and the relationship with the nearby structures, 3) the histological type, 4) the clinical characteristics, in the recurrences, 5) the general conditions of health and the age of the patient (14). Among this series of factors the histological aspect has a decisive role: the solid multicystic ameloblastoma and the unicystic-intramural ameloblastomas, subtype III of Ackerman, need radical treatment, with the resection of 1-2 cm of healthy bone (12-15-17), although not all the authors have found high rates of recurrence after the conservative treatment of such forms (5). On the contrary the unicystic intraluminal ameloblastoma rarely recurrers after conservative therapy, only 10 % according to Leider (15), Eversole (16), Gardner (17) and 13,7% according to Reichart (5). Therefore a conservative aproach it is advisable in the case of a non invasive and non proliferating cyst wall. The location of the lesion seems to be an important risk factor for the recurrence of the ameloblastoma in fact the most frequent recurrence were located in the third posterior of the jaw.
Conclusion
We think that the product of our experience, is useful for an efficient programming of treatment, taking in consideration numerous variables of this pathology and the indications found in literature.
We believe that for the diagnostic phase the instrumental examinations (X-RAY, CT or MRT) are essential; while intralesional byopsies are inefficient because they don t offer a whole vision of the tumor and could lead to diagnostic error. Therefore we think that it is advisable, considering: the site and extention, of the lesion, age and general conditions of the patient, to remove the lesion in a conservative manner in a first surgical step and according to the histolgical aspect evaluate a possible radical resection.
References
1. Larsson A Ê, Almeren H. Ameloblastoma of the jaws. An analysis of a consecutive series of all cases reported to the Swedish Cancer Registry during 1958-1971. Acta Pathologica et Microbiologica Scandinavica (A) 1978;86:337-49. [ Links ]
2. Shear M, Singh S. Age-standardized incidence rates of ameloblastoma and dentigerous cyst on the Witwatersrand, South Africa. Community Dentistry and Oral Epidemiology 1978; 6:195-9. [ Links ]
3. Gardner DG, PecË sak AMJ. The treatment of ameloblastoma based on pathologic and anatomic principles. Cancer 1980; 46:2514-9. [ Links ]
4. Robinson L, Martinez MG. Unicystic ameloblastoma: a prognostically distinct entity. Cancer 1977;40:2278-85. [ Links ]
5. Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological prole of 3677 cases. Oral Oncology, European Journal of Cancer 1995; 31B:86-99. [ Links ]
6. Critique of the 1995 review by Reichart et al.$ of the biologic erole of 3677 ameloblastomas D.G. Gardner Oral Oncology 1999;35:443-9. [ Links ]
7. Khan MA: Ameloblastoma in young persons: A clinicopathologic analysis and etiologic investigation. Oral Surg Oral Med Oral Pathol 1984; 67:706. [ Links ]
8. Eversole LR, Leider AS, Strub D. Radiographic characteristics of cystogenic ameloblastoma. Oral Sug Oral Med Oral Pathol 1984;57:572-7. [ Links ]
9. Gardner DG: Plexiform unicystic ameloblastoma: A diagnostic problem in dentigenous cysts. Cancer 1981; 47:1358. [ Links ]
10. Struthers P, Shear M: Root resorption by Ameloblastomas and cysts of the jaws. Int J Oral Surg 5:128, 1976. [ Links ]
11. 258 Kramer IR. Ameloblastoma: a clinicopathological appraisal. Br J Oral Surg 1963;1:13-28. [ Links ]
12. Regezi JA, Kerr DA, Courtney RM. Odontogenic tumors: analysis of 706 cases. J Oral Surg 1978;36:771-8. [ Links ]
13. Ackerman GL, Altini M, Shear M: The unicystic ameloblastoma: A clincopathological study of 57 cases. J Oral Pathol 1988;17:541. [ Links ]
14. HP Philipsen A, PA Reichart BH. Nikai CT. Takata CY. Kudo. Review Peripheral ameloblastoma: biological role based on 160 cases from the literature. Oral Oncology 2001; 37:17-27. [ Links ]
15. Ueno S, Nakamura S, Mushimoto K, Shirasu R. A clinicopathologic study of ameloblastoma. Journal Oral Maxillofacial Surgery 1986;44:361-5. [ Links ]
16. Waldron CA, El-Mofty SK. A histopathologic study of 116 ameloblastomas with special reference to the desmoplastic variant. Oral Surgery Oral Medicine Oral Pathology 1987;63:441-7. [ Links ]
17. Rick G, Howell F, Pindborg J. The peripheral Ameloblastoma: a clinicopathologic study of 18 cases. Journal Oral Pathology 1985;14:85. [ Links ]
18. Niccoli-Filho W, Gomes da MGME, Raldi FV, Seraidarian PI. Peripheral ameloblastoma. Journal Nihon University School of Dentistry 1997;39:34-7. [ Links ]
19. Buchner A, Sciubby JJ. Peripheral epithelial odontogenic tumors: a review. Oral Surgery Oral Medicine Oral Pathology 1987;63:688-97. [ Links ]
20. Nauta JM, Panders AK, Schoots CJF, Vermey A, Roodenburg JLN. Peripheral ameloblastoma. A case report and review of the literature. International Journal Oral Maxillofacial Surgery 1992;21:40-4. [ Links ]
21. Vickers RA, Gorlin RJ. Ameloblastoma: delineation of early istopatologic features of neoplasia. Cancer 1970;3, 699-710. [ Links ]
22. Kramer IRH, Pindborg JJ, Shear M. Histological typing of odontogenic tumours. 2nd ed. Berlin: Springer-Verlag; 1992. [ Links ]
23. Leider AS, Eversole LR, Barkin ME. Cystic ameloblastoma. A clinopathologic analysis. Oral Sug Oral Med Oral Pathol 1985;60:624-30. [ Links ]
24. Eversole LR, Leider AS, Strub D. Radiographic characteristics of cystogenic ameloblastoma. Oral Sug Oral Med Oral Pathol 1984;57:572-7. [ Links ]
25. Eggert JH, Steinhauser EW. Besonderheiten der Oberkiefer-Ameloblastome Beobachtungen an 12 Fallen. Fortschr Kiefer Gesichtschir 1986;31:101-4. [ Links ]
26. Shaw HJ, Katsikas DK. Ameloblastoma of the maxilla. A clinical study with four cases. J Laryngol Otol. 1973;87:873-84. [ Links ]
27. Eichhorn T, Glanz H, Kleinsasser O. Ameloblastome des Oberkiefers. Bericht uber 6 Falle und Literaturzusammenstellung. HNO 1982;30: 1-8. [ Links ]
28. Batsakis JG, Mclatchey KD. Ameloblastoma of the maxilla and paripheral ameloblastomas. Am Otol Rhinol Laryngol 1983;92:532-4. [ Links ]
29. Pilz G, Nitzschke M. Uber die Spatrezidivierung der Ameloblastome. Stomatol DDR 1979;29: 107-11. [ Links ]
30. Sandler KA, Novo RM, Rudner BE. A study of ameloblastoma- age, sex, location statistics. NY State Dent J 1983; 49: 682-4. [ Links ]
31. Young DR, Robinson M, Ameloblastoma in children: report of a case. Oral Sug Oral Med Oral Pathol 1962;15: 1155-62. [ Links ]
32. Sehdev MK, Huvos AG, Strong EW, Gerold FP, Willis GW. Proceedings: Ameloblastoma of maxilla and mandible. Cancer 1974; 33: 324-33. [ Links ]
33. Menakanit W. Ameloblastoma of the jaw: a 10 year analysis (1966-1975). J med Assoc Thai 1979; 62: 6-9. [ Links ]
34. Gardner DG. A pathologysts approach to the treatment of ameloblastoma. J Oral Maxillofac Surg 1984; 43:161-6. [ Links ]
35. Philipsen HP, Reichart PA. Revision of the 1992 edition of the WHO histological typing of odontogenic tumors. A suggestion. J Oral Pathol Med 2002;31:253-8. [ Links ]











 texto en
texto en