Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
The European Journal of Psychiatry
versión impresa ISSN 0213-6163
Eur. J. Psychiat. vol.23 no.3 Zaragoza jul./sep. 2009
Light-therapy applications for DSM-IV-TR disease entities
Mercedes Paino, Eduardo Fonseca-Pedrero, Manuel Bousoño, Serafín Lemos-Giráldez
Department of Psychology. University of Oviedo. Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), Ministry of Science and Innovation. SPAIN
This research has received funding from the Spanish Ministry of Science and Innovation (MICINN), the Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM) and the Fundación Universidad de Oviedo (FUO), Project references: PSI2008-06220/PSIC, PSI2008-03934, FUO-EM-101-08.
ABSTRACT
Background and Objectives: Recent decades have seen significant advances in the knowledge of pathogenesis of mood disorders, as well as of other conditions directly or indirectly related to such diseases. Such progress has led to the emergence of new treatments, such as bright light therapy, based on the discovery of the therapeutic effects of exposure to bright light with the so-called seasonal affective disorder (SAD), a DSM seasonal pattern specifier linked to major depression and bipolar disorder recurrent describing the course of illness during seasons. The goal of the present work is to review the potential clinical applications of phototherapy, including SAD, obsessive-compulsive disorder, bulimia, premenstrual syndrome, non seasonal major depression, sleep disorders, jet-lag, dementia, normal populations and in primary care.
Methods: A systematic review of the literature about this matter since the early Rosenthal,s group observations has been carried out.
Results: A considerable number of studies has been published about this therapeutic approach, pointing that not only depression but also other pathologies that may follow a seasonal pattern could benefit from phototherapy integrated with more standard treatments, as well as other disorders directly or indirectly related to mood, and even another conditions without a seasonal pattern.
Conclusions: The data about the different uses of this treatment neither confirm nor dismiss its efficacy, stating that the therapy should still be regarded as experimental. Future studies should continue investigating to draw reliable conclusions about the usefulness of bright light therapy on mood disorders and other conditions to provide an alternative to standard treatments almost exclusively based on psychoactive drugs.
Key words: Seasonal affective disorder (SAD); Light therapy; Phototherapy.
Seasonal affective disorder (SAD)
The therapeutic effects of exposure to bright light are by no means a phenomenon of recent discovery. As early as the 1920s, thanks primarily to the work of Kraepelin1, attention was drawn to the presence of certain depressive disorders which, in contrast to other affective disorders, would begin in a more or less regular way in the autumn/winter, with remission in the spring/summer. These initial observations led Rosenthal's2 team to define what was known as seasonal affective disorder (SAD) or seasonal depression, after demonstrating the antidepressant effect of exposure to bright light in this type of patient3,4. Thus, the condition would consist in recurrent depressive episodes occurring annually, tending this "winter" depression to be characterised by anergy, hypersomnia, hyperphagia, increased appetite, weight gain and compulsive consumption of carbohydrates5,6.
The first symptoms of SAD usually occur in adulthood, and the severity of the syndrome often increases with geographical latitude2,7; it is more common in women, and in the age range 35 to 508. However, SAD is not considered as a separate diagnostic category: the DSM-III-R9 refers to "specification of seasonal pattern" to apply to Bipolar disorders I and II and to Recurrent Major Depressive Disorder, the principal characteristic of this pattern being the onset and remission of major depressive episodes at certain times of the year.
Given the characteristics of SAD, the reduction in exposure to daylight has been hypothesised as its principal aetiological triggering factor, based on population surveys carried out from the 1990s onwards which explored changes in the prevalence of the disorder in relation to geographical latitude in countries such as the USA10, Japan11, Finland12 and Australia13, as well as in samples from polar expeditions14 and from military personnel and their families15.
Numerous alternative explanations of the pathogenic mechanisms of SAD have been proposed. The early theories receiving the most empirical support were those related to a psychophysical alteration in light sensitivity due to a retinal or hypothalamic deficit16. But the discovery that treatment with bright light improved depressive symptoms in such patients has led researchers to focus their attention on the circadian system and the regulatory role of melatonin in it for explaining not only the cause of the disorder but also the therapeutic mechanism of phototherapy17,18.
Light therapy
By the 1990s, the effectiveness of treatment with bright light for "winter depression" had been described in over 30 controlled studies, with more than 300 patients at 14 different research centres19; recent reviews have confirmed the success of this treatment20,21, due primarily to its rapid and well-tolerated antidepressant effect.
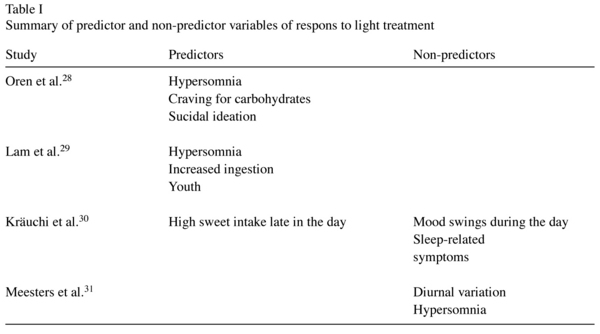
Numerous studies have used the Hamilton Depression Rating Scale-Seasonal Affective Disorders Version (HDRS-SAD)22 in an effort to identify possible predictors of response to treatment. The results of these studies indicate that non-responders to treatment with light for SAD displayed different clinical profiles when they were depressed6,23,24, with higher scores on the Hamilton scale and lower scores on the complementary atypical symptoms scale; the more severe the atypical symptoms of depression (i.e., hypersomnia, fatigability or carbohydrate craving) the more likely they were to respond to phototherapy, while greater severity of melancholic ("endogenous") symptoms (i.e., suicide, feelings of guilt, motor retardation, insomnia, anxiety, typical diurnal variation -morning worse- or despersonalization) predict a poor response. Other studies have identified specific symptoms as potential predictors of response to light therapy (see Table I), and a current research line attempts to relate personality variables and the response to phototherapy25-27.
Types of light
The original design for research on phototherapy with SAD used a system of full-spectrum fluorescent bulbs, giving off light containing all the wavelengths of sunlight from behind a plastic diffusing screen inside a rectangular box32. Since then, there has been speculation as to whether full-spectrum light is actually an essential requirement for the treatment of SAD33, leading to research on the efficacy of different light spectra34-36, including full-spectrum light with or without ultraviolet rays, cool-white light (i.e., fluorescent light with a substantial production of energy in the green and yellow wave bands, and a small quantity of ultraviolet emission), red light, green light and incandescent light (yellow waves with negligible ultraviolet emission). However, and in spite of considerable research efforts, the properties of the light spectrum most suitable for use in phototherapy for SAD have not yet been clearly identified, though it does seem to be clear that ultraviolet wavelengths are not necessary for the antidepressant effect in SAD, so that, given its potentially harmful effects, it should not be used in phototherapy for this disorder37.
Clinical applications of light therapy
In the early 1990s, Rosenthal's38 group set out to explore the extent to which seasonality might be a feature of other neuropsychiatric entities, and to study the effectiveness of light therapy for different disorders. From then on, a range of studies have focused on the seasonal pattern and light-therapy applications for diverse conditions:
a) Obsessive-compulsive disorder (OCD)
Initially, seasonal variation in the symptoms of 34 patients with OCD was explored38. Of these patients, who used a retrospective self-report scale measuring mood and behavioural changes, a considerable proportion with obsessive-compulsive disorder (53%) reported a marked seasonal variation in their symptoms. Furthermore, evidence that serotoninergic brain systems are altered in both OCD and SAD lends theoretical support to the use of light therapy for obsessive-compulsive disorder, and in practice a reduction in obsessive-compulsive symptoms through its use has indeed been demonstrated39.
b) Bulimia
There is growing evidence that some patients with bulimia nervosa display a marked seasonal pattern in mood and in symptoms related to ingestion40, estimating a prominent worsening of the mood and the symptoms related to ingestion in winter in a high percentage of these patients, percentages varying among the different studies from 10% to as much as 42%. Treatment with light has been shown to be effective and well tolerated in patients with SAD, achieving a rapid improvement of mood state and eating-disorder symptoms, as well as in patients with seasonal patterns of bulimia nervosa41,42, though in the case of these bulimic patients it is recommended that phototherapy be used in conjunction with other treatments of a pharmacological and/or psychological nature.
c) Premenstrual syndrome
Premenstrual syndrome is characterised by cyclical mood changes that correspond to the menstrual cycle43, and it has been shown how women with SAD frequently also present premenstrual syndrome44, as well as other common symptoms, such as over-sleeping, carbohydrate craving and lethargy2,43. Very recent studies with large samples of women with premenstrual syndrome, moreover, have reported a reduction in depressive symptoms and premenstrual tension as a result of light therapy45,46.
d) Panic disorder
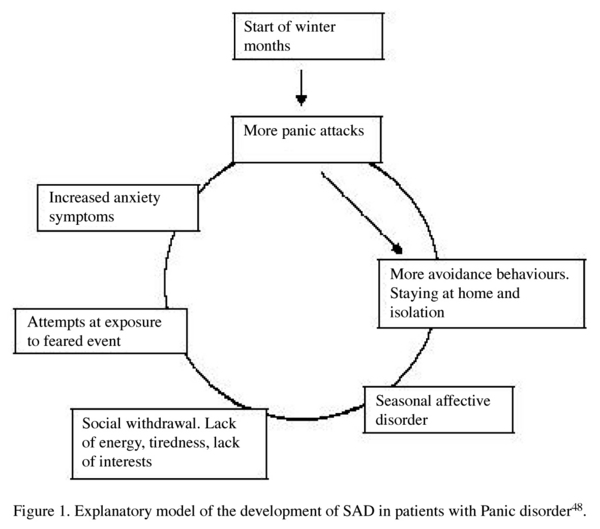
Panic disorder is characterised by episodes of acute anxiety with intense fear or distress and symptoms of physiological activation. Clinical assessments of patients with this disorder indicate the possibility of a seasonal pattern in a high percentage47,48, with a pronounced peak in their attacks during the winter months. An explanatory model has been proposed by Marriot and cols.48 for the development of SAD in patients with panic disorder (Figure 1) which hypothesises a common aetiology for the two disorders related to seasonality, so that light therapy could constitute an appropriate treatment for some of these patients.
e) Non-seasonal major depression
Although several investigators have regarded light therapy as a first-line treatment for seasonal affective disorder (SAD), the results of light therapy in nonseasonal major depressive disorder have been non-conclusive49. Nevertheless, it seems that major depressed patients can be predicative of beneficial outcome of subsequent light therapy, but since the patients use to be additionally treated with medication, an interaction of the two adjunctive therapies cannot be excluded. Recently accumulated evidence has demonstrated that bright-light therapy in combination with antidepressants is effective in patients with non-seasonal major depression50,51.
f) Sleep disorders
Exposure of the eyes to light of an appropriate intensity and duration and at a certain time of day can have substantial effects on the rhythm, duration and quality of sleep52. In patients suffering from SAD accompanied by hypersomnia or delayed sleep phase, normalisation of sleep can be achieved through light therapy, as well as a remission of or improvement in depressive symptoms53,54. Patients without SAD but who experience alterations in their sleep phases, such as initial or terminal insomnia when they try to sleep at normal times, maybe could also be treated with such methods55.
Research in this field has revealed differences between patients with SAD and normal controls in the architecture of sleep, the former displaying higher rapid eye movement (REM) density (though not a shorter latency) throughout the year and a reduction of delta sleep in winter during depressive phases56. Light therapy has yielded satisfactory results for stimulating delta sleep and the effectiveness of sleep, at the same time reducing the density of REM sleep.
g) Jet-lag
Jet-lag, or the syndrome resulting from rapid change of time zone, is a complaint affecting travellers and aircrew on long-haul flights from east to west and vice versa. This phenomenon involves a desynchronisation between the endogenous circadian system, which continues to be synchronised with the time markers of the point of departure, and the geo-social system of the point of arrival. Adjustment takes around 4 days, provoking for example, variations in cognitive and athletic performance, body temperature or alcohol metabolism. However, the main symptom being sleep alterations, because of that temporal asynchrony between a sudden change of the time of sleep (owing to the adjustment to the new local day-night cycle) and a progressive readaptation of the circadian system.
Early laboratory studies had not been sufficiently conclusive in support of the hypothesis that bright light could alleviate jet-lag57,58. Nevertheless, the most recent research has attempted to determine the relationship between light therapy and the effects of melatonin, using medication in this context for the treatment of jet-lag59,60. Several laboratory and field experiments with different doses of melatonin, have found that occasional short-term use of melatonin, taken close to the target bedtime at the destination (i.e., 10 pm to midnight), decreased jet-lag from flights crossing five or more time zones59,61,62. However, trials with just timed exposure to bright light (without melatonin) do not give enough support to it's efficacy for alleviating jet lag symptoms63,64.
h) Dementia
Early research in this area included that of Fontana Gasio's65 team in Switzerland, who studied for a period of three weeks the effects of certain light therapy conditions after sunset on the sleep cycles of elderly patients with dementia, finding a marked improvement in sleep quality and cognitive functions. Other studies have confirmed such results in patients with Alzheimer-type dementia66,67, highlighting the effect on sun-downing, the syndrome of confusion and agitation that occurs at dusk in this type of patient.
In a more recent long-term, doubled-blind, placebo-controlled study with elderly residents of group care facilities, Riemersma-van der Lek et al.68 had concluded that light has a modest benefit in improving some cognitive and noncognitive symptoms of dementia, recommending it only in combination with light to counteract the adverse effect of melatonin on mood. This work is along the lines of a recent Cochrane review on light and dementia69, who concluded that there is insufficient evidence of efficacy of bright light therapy in managing sleep, behaviour, mood, and cognitive disturbances associated with dementia.
i) Normal population
Seasonal changes in mood and behaviour are frequent among the general population, mainly affecting women of reproductive age. Given the antidepressant and energising effects of light therapy in patients with SAD, research has tried to determine whether other sectors of the population could benefit from phototherapy, especially those presenting so-called subsyndromal SAD, a milder form of the disorder whose sufferers do not fulfil the criteria for the diagnosis of SAD per se. People presenting this seasonal subsyndrome have been found to respond favourably to treatment with bright light, especially in conditions of long exposure70,71. Likewise, research has shown the utility of exposure to bright light during the winter months for relieving stress and improving vitality in healthy people72.
j) Applications in primary care
Between 10 and 15% of primary care patients in industrialised countries express some complaint about certain behavioural alterations and low mood state during the winter months, year on year. In spite of these percentages, just 0.2% of all patients and 3% of depressed patients who consult their GP are diagnosed with SAD. Attempts to assess the efficacy of light therapy in primary care patients have yielded positive results, and this could point the way to a treatment alternative for SAD patients seeking help in the primary care context73.
Conclusions
The significant progress in the area of mood disorders and other pathologies in recent decades, including advances in diagnostic, pathogenetic and epidemiological knowledge, has been accompanied by the emergence of new treatments, among them that of light therapy. The goal of the present work was to review the potential clinical applications of phototherapy for different defined disease entities on the DSM-IV-TR, as well its possible use with normal populations and in primary care. Although treatment with light therapy is well established since the very first studies on its application to SAD, it must be heeded for recent conclusions of the Swedish Council on Technology Assessment in Health Care's (SBU) report on light therapy for depression74; they declare that, although a considerable number of studies has been published about the use of this treatment for SAD, it's efficacy can be neither confirmed nor dismissed, stating that the therapy should still be regarded as experimental, because of the lack of significant difference between placebo and light therapy with regard to the number of patients who improve bay at least 50%. In keeping with this point of view, the present overview of the results obtained from different studies indicates that the effectiveness of this treatment for the revised conditions still remains unconfirmed, because of the lack of satisfactory controlled studies.
Nevertheless, it has been pointed that not only depression but also other pathologies may follow a seasonal pattern, and therefore could benefit from phototherapy, primarily as an approach integrated with more standard treatments. In fact, many potential areas of application of this therapy have to do with disorders directly or indirectly related to mood. Apart from anything else, it's common knowledge that another conditions without a seasonal pattern, could still be helped with this treatment.
Likewise, seasonal changes in mood and behaviour are common in the general population, and light therapy also might constitute an effective treatment, in spite of some people have reported mild (no substantial) side-effects75-77 usually temporary and generally remedied by reducing exposure time, including: headaches, ocular tension, eye irritation or disturbing sensations of visual glare, mild hypomania and irritability, sleep disturbances in patients that use light at dusk, overactive state, jumpiness, jitteriness or feeling "wired", and also slight nausea.
On the other hand, and despite the potential utility of this therapy, we should not overlook the possible interaction of mood with activities that the person may do during the seasons with more light and where there is more exposure to sunlight, with the resulting synergic effect between light and more reinforcing lifestyles. Furthermore, no satisfactory controlled studies have been published on the subject, reflecting the great need to conduct these studies with enough participants to draw reliable conclusions about the efficacy of bright light therapy on mood disorders and other conditions.
In this line of new treatments it is also relevant to mention the research being carried out on Behavioural Activation Therapy for depression, which has concluded that this therapy produces results equivalent to those of psychoactive drugs in patients with severe depression78. The findings of this and other recent studies have reopened the debate on the effectiveness and wisdom of the use of psychoactive drugs in the treatment of some psychological disorders, such as depression79,80, indirectly calling into question the models of mental illness and intervention customarily used by health services in dealing with this type of problem.
Finally, the results pointed out with the new therapies, notably light therapy, lead inevitably to a reappraisal of current approaches to the treatment of disorders involving mood alterations. Given that today the equipment necessary for applying phototherapy can be bought or rented from many medical suppliers, such findings should encourage clinicians to make greater efforts to recognise the types of symptoms and of patients who might benefit from this relatively new form of treatment, and to ensure that it is offered and applied in an appropriate way.
References
1. Kraepelin E. Manic depressive insanity and paranoia. Edinburgh: Livingstone; 1921. [ Links ]
2. Rosenthal NE, Sack DA, Gillin JC, Lewy AJ, Goodwin FK, Davenport Y, et al. Seasonal Affective Disorder: A description of the syndrome and preliminary findings with light therapy. Arch Gen Psychiatry 1984; 41: 72-80. [ Links ]
3. Byrne B, Brainard GC. Seasonal Affective Disorder and Light Therapy. Sleep Med Clin 2008; 3: 307-315. [ Links ]
4. Eagles JM. Light therapy and seasonal affective disorder. Psychiatry 2009; 8: 125-129. [ Links ]
5. Lewy AJ, Wehr TA, Goodwin FK, Newsome DA, Markey SP. Light suppresses melatonin secretion in humans. Science 1980; 210: 1267. [ Links ]
6. Stinson D, Thompson C. Clinical experience with phototherapy. J Affect Disord 1990; 18: 129-135. [ Links ]
7. Agumadu CO, Yousufi SM, Malik IS, Nguyen MC, Jackson MA, Soleymani K, et al. Seasonal variation in mood in African American college students in the Washington, D.C., metropolitan area. Am J Psychiatry 2004; 161(6): 1084-1089. [ Links ]
8. Matías J, Manzano JM, Santalla JL, Carrasco JL, Llorca G, Ledesma A. Trastorno afectivo estacional y terapia lumínica. Actas Luso Esp Neurol Psiquiatr Cienc Afines 1996; 24(4): 204-208. [ Links ]
9. APA. Diagnostic and statistical manual of mental disorders (3rd ed. revised) (DSM-III-R). Washington, DC: American Psychiatric Association; 1987. [ Links ]
10. Rosen LN, Targum SD, Terman M, Bryant MJ, Hoffman H, Kasper SF, et al. Prevalence of seasonal affective disorder at four latitudes. Psychiatry Res 1990; 31: 131-144. [ Links ]
11. Takahashi K, Asano Y, Kohsaka M, Okawa M, Sasaki M, Honda Y, et al. Multi-center study of seasonal affective disorders in Japan: A preliminary report. J Affect Disord 1991; 21: 57-65. [ Links ]
12. Partonen T, Partinen M. Light treatment for seasonal affective disorder: Theoretical considerations and clinical implications. Acta Psychiatr Scand 1994; 377: 41-45. [ Links ]
13. Murria G. How common is seasonal affective disorder in temperate Australia? A comparison of BDI and SPAQ estimates. J Affect Disord 2004; 81: 23-28. [ Links ]
14. Palinkas LA, Suedfeld P. Psychological effects of polar expeditions. Lancet, 2008; 371: 153-163. [ Links ]
15. Rosen LN, Moghadam LZ. Patterns of seasonal change in mood and behavior: An example from a study of military wives. Mil Med 1991; 156: 228-230. [ Links ]
16. Reme C, Terman M, Wirz-Justice A. Are deficient retinal photoreceptor renewal mechanisms involved int the pathogenesis of winter depression? Arch Gen Psychiatry 1990; 47: 878-879. [ Links ]
17. Desan PH, Oren DA. Is seasonal affective disorder a disorder of circadian rhythms? CNS Spectr 2001; 6(6): 487-494, 499-501. [ Links ]
18. McClung CA. Circadian genes, rhythms and the biology of mood disorders. Pharmacol Ther 2007; 114: 222-232. [ Links ]
19. Terman M, Terman JS, Wuitkin FM, McGrath PJ, Stewart JW, Rafferty B. Light therapy for seasonal affective disorder. A review of efficacy. Neuropsychopharmacology 1989; 2: 1-22. [ Links ]
20. Golden RN, Gaynes BN, Ekstrom RD, Hamer RM, Jacobsen FM, Suppes T, et al. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry 2005; 162(4): 656-662. [ Links ]
21. Rastad C, Ulfberg J, Lindberg P. Light room therapy effective in mild forms of seasonal affective disorder-A randomised controlled study. J Affect Disord 2008; 108: 291-296. [ Links ]
22. Williams JBW, Link MJ, Rosenthal NE, Amira L, Terman M. Structured interview guide for the Hamilton Depression Rating Scale, Seasonal Affective Disorders Version (SIGH-SAD), revised ed. New York: New York State Psychiatric Institute; 1994. [ Links ]
23. Nagayama H, Sasaki M, Ichii S, Hanada K, Okawa M, Ohta T, et al. Atypical depressive symptoms possibly predict responsiveness. J Affect Disord 1991; 23: 185-189. [ Links ]
24. Terman M, Amira L, Terman JS, Ross DC. Predictors of response and nonresponse to light treatment for winter depression. Am J Psychiatry 1996; 153(11): 1423-1429. [ Links ]
25. Goel N, Terman M, Terman JS. Dimensions of temperament and bright light response in seasonal affective disorder. Psychiatry Res 2003; 119(1-2): 89-97. [ Links ]
26. Haffmans J, Koppelaar V, Hoencamp E. Comorbidity and personality in patients with Seasonal Affective Disorder. J Affect Disord 2008; 107: S117. [ Links ]
27. Maeno N, Kusunoki K, Kitajima T, Iwata N, Ono Y, Hashimoto S, et al. Personality of seasonal affective disorder analyzed by Tri-dimensional Personality Questionnaire. J Affect Disord 2005; 85: 267-273. [ Links ]
28. Oren DA, Jacobsen FM, Wehr TA, Cameron CL, Rosenthal NE. Predictors of response to phototherapy in seasonal affective disorder. Compr Psychiatry 1992; 33: 111-114. [ Links ]
29. Lam RW, Goldner EM, Solyom L, Remick RA. A controlled study of light therapy for bulimia nervosa. Am J Psychiatry 1994; 151(5): 744-750. [ Links ]
30. Kräuchi K, Wirz-Justice A, Graw P. High sweet intake late in the day predicts a rapid and persistent response to light therapy in winter depression. Psychiatry Res 1993; 46: 107-117. [ Links ]
31. Meesters Y, Jansen JHC, Lambers PA, Bouhuys AL, Beersma DGM, Van den Hoofdakker RH. Morning and evening light treatment of seasonal affective disorder: response, relapse, and prediction. J Affect Disord 1993; 28: 165-177. [ Links ]
32. Rosenthal NE, Sack DA, Skwerer RG, Jacobsen FM, Wehr TA. Phototherapy for seasonal affective disorder. In: Rosenthal NE, editor. Seasonal affective disorders and phototherapy. New York: The Guildford Press; 1989. p. 273-295. [ Links ]
33. Bielski RJ, Mayor J, Rice J. Phototherapy with broad spectrum white fluorescent light: a comparative study. Psychiatry Res 1992; 43: 167-175. [ Links ]
34. Brainard GC, Sherry D, Skwerer RG, Kelly WK, Rosenthal NE. Effects of different wavelengths in seasonal affective disorder. J Affect Disord 1990; 20: 209-216. [ Links ]
35. Lam RW, Buchanan A, Clark CM, Remick RA. Ultraviolet versus non-ultraviolet light therapy for seasonal affective disorder. J Clin Psychiatry 1991; 52: 213-216. [ Links ]
36. Oren DA, Brainard GC, Johnston SH, Joseph-Vanderpool JR, Sorek E, Rosenthal NE. Treatment of seasonal affective disorder with green light and red light. Am J Psychiatry 1991; 148: 509-511. [ Links ]
37. Lee TMC, Chan CCH, Paterson GJ, Janzen HL, Blashko CA. Spectral properties of phototherapy for seasonal affective disorder: a meta-analysis. Acta Psychiatr Scand 1997; 96: 117-121. [ Links ]
38. Yoney TH, Pigott TA, L'Heureux F, Rosenthal NE. Seasonal variation in obsessive-compulsive disorder: preliminary experience with light treatment. Am J Psychiatry 1991; 148(12): 1727-1729. [ Links ]
39. Brinkhuijsen M, Koenegracht F, Meesters Y. Symptoms of seasonal affective disorder and of obsessive-compulsive disorder reduced by light therapy. J Affect Disord 2003; 74(3): 307-308. [ Links ]
40. Lam RW, Solyom L, Tompkins A. Seasonal mood symptoms in bulimia nervosa and seasonal affective disorder. Compr Psychiatry 1991; 32: 552-555. [ Links ]
41. Braun DL, Sunday SR, Fornari VM, Halmi KA. Bright light therapy decreases winter binge frequency in women with bulimia nervosa: A double-blind, placebo-controlled study. Compr Psychiatry 1999; 40(6): 442-448. [ Links ]
42. Lam RW, Lee SK, Tam EM, Grewal A, Yatham LN. An open trial of light therapy for women with seasonal affective disorder and comorbid bulimia nervosa. J Clin Psychiatry 2001; 62(3): 164-168. [ Links ]
43. Dalton K. The Premenstrual Syndrome. Springfield: Charles C. Thomas; 1964. [ Links ]
44. Praschak-Rieder N, Willeit M, Neumeister A, Hilger E, Stastny J, Thierry N, et al. Prevalence of premenstrual dysphoric disorder in female patients with seasonal affective disorder. J Affect Disord 2001; 63: 239-242. [ Links ]
45. Haffmans J, Richmond A, Landman F, Blom M. The effects of light therapy and cognitive behavioral therapy in premenstrual dysphoric disorder (PMDD). J Affect Disord 2008; 107: S86. [ Links ]
46. Krasnik C, Montori VM, Guyatt GH, Heels-Ansdell D, W. BJ, Group ftMUSS. The effect of bright light therapy on depression associated with premenstrual dysphoric disorder. Am J Obstet Gynecol 2005; 193: 658-661. [ Links ]
47. Kanofsky JD, Sandyk R, Kaplan S, Yaryura-Tobias JA. Seasonal panic disorder responsive to light therapy. Lancet 1991; 337(8749): 1103-1104. [ Links ]
48. Marriot PF, Greenwood KM, Armstrong SM. Seasonality in panic disorder. J Affect Disord 1994; 31: 75-80. [ Links ]
49. Fritzsche M, Heller R, Hill H, Kick H. Sleep deprivation as a predictor of response to light therapy in major depression. J Affect Disord 2001; 62(3): 207-215. [ Links ]
50. Even C, Schröder CM, Friedman S, Rouillon F. Efficacy of light therapy in nonseasonal depression: a systematic review. J Affect Disord 2008; 108(1-2): 11-23. [ Links ]
51. Martiny K. Adjunctive bright light in non-seasonal major depression. Acta Psychiatr Scand Suppl 2004; 425: 7-28. [ Links ]
52. Björkstén K S, Bjerregaard P, Kripke DF. Suicides in the midnight sun-a study of seasonality in suicides in West Greenland. Psychiatry Res 2005; 133(2-3): 205-213. [ Links ]
53. Murray G, Michalak EE, Levitt AJ, Levitan RD, Enns MW, Morehouse R, et al. O sweet spot where art thou? Light treatment of Seasonal Affective Disorder and the circadian time of sleep. J Affect Disord 2006; 90: 227-231. [ Links ]
54. Postolache TT, Oren DA. Circadian phase shifting, alerting, and antidepressant effects of bright light treatment. Clin Sport Med 2005; 24(2): 381-413. [ Links ]
55. Gammack JK. Light Therapy for Insomnia in Older Adults. Clin Geriatr Med 2008; 24: 139-149. [ Links ]
56. Skwerer RG, Jacobsen FM, Kelly WK, Sack DA, Tamarkin L, Gaist PA, et al. Neurobiology of seasonal affective disorder and phototherapy. J Biol Rhythms 1988; 3(2): 135-154. [ Links ]
57. Chesson AL, Littner M, Davila D, Anderson WM, Grigg-Damberger M, Hartse K, et al. Practice parameters for the use of light therapy in the treatment of sleep disorders. Standards of Practice Committee, American Academy of Sleep Medicine. Sleep 1999; 22(5): 641-660. [ Links ]
58. Samel A, Wegmann HM. Bright light: A countermeasure for jet lag? Chronobiol Int 1997; 14(2): 173-183. [ Links ]
59. Lathrop NJ, Lentz M. Melatonin, light therapy, and jet lag. Air Med J 2001; 20(5): 30-34. [ Links ]
60. Skene DJ, Arendt J. Circadian rhythm sleep disorders in the blind and their treatment with melatonin. Sleep Med 2007; 8: 651-655. [ Links ]
61. Herxheimer A, Petrie KJ. Melatonin for the prevention and treatment of jet lag (Cochrane Review). Cochrane Database Syst Rev 2002; 2: CD001520. DOI: 10.1002/14651858. CD001520. [ Links ]
62. Parry BL. Jet lag: minimizing it's effects with critically timed bright light and melatonin administration. J Mol Microbiol Biotechnol 2002; 4(5): 463-466. [ Links ]
63. Boulos Z, Macchi MM, Stürchler MP, Stewart KT, Brainard GC, Suhner A, Wallace G, Steffen R. Light visor treatment for jet lag after westward travel across six time zones. Aviat Space Environ Med 2002; 73(10): 953-963. [ Links ]
64. Lahti T, Terttunen J, Leppämäki S, Lönnqvist J, Partonen T. Field trial of timed bright light exposure for jet lag among airline cabin crew. Int J Circumpolar Health 2007; 66(4): 365-369. [ Links ]
65. Fontana Gasio P, Krauchi K, Cajochen C, Someren E, Amrhein I, Pache M, et al. Dawn-dusk simulation light therapy for disturbed circadian rest-activity cycles in demented elderly. Exp Gerontol 2003; 38(1-2): 207-216. [ Links ]
66. Asayama K, Yamadera H, Ito T, Suzuki H, Kudo Y, Endo S. Double blind study of melatonin effects on the sleep-wake rhythm, cognitive and non-cognitive functions in Alzheimer type dementia. J Nippon Med Sch 2003; 70(4): 334-341. [ Links ]
67. Wu YH, Swaab DF. Disturbance and strategies for reactivation of the circadian rhythm system in aging and Alzheimer's disease. Sleep Med 2007; 8: 623-636. [ Links ]
68. Riemersma-van der Lek RF, Swaab DF, Twisk J, Hol EM, Hoogendijk WJG, Van Someren EJW. Effect of Bright Light and Melatonin on Cognitive and Noncognitive Function in Elderly Residents of Group Care Facilities: A Randomized Controlled Trial. JAMA2008;299(22):2642-2655. [ Links ]
69. Forbes D, Morgan DG, Bangma J, Peacock S, Adamson J. Light Therapy for Managing Sleep, Behaiour, and Mood Disturbances in Dementia (Cochrane Review). Cochrane Database Syst Rev 2004; 2: CD003946.DOI: 10.1002/14651858.CD003946.pub2. [ Links ]
70. Kasper S, Rogers SL, Yancey A, Schulz PM, Skwerer, RG, Rosenthal NE. Phototherapy in individuals with and without subsyndromal seasonal affective disorder. Arch Gen Psychiatry 1989; 46(9): 837-844. [ Links ]
71. Levitt AJ, Lam RW, Levitan R. A comparison of open treatment of seasonal major and minor depression with light therapy. J Affect Disord 2002; 71(1-3): 243-248. [ Links ]
72. Partonen T, Lönnqvist J. Bright light improves vitality and alleviates distress in healthy people. J Affect Disord 2000; 57: 55-61. [ Links ]
73. Remick RA. Diagnosis and management of depression in primary care: a clinical update and review. Can Med Assoc J 2002; 167(11): 1253-1260. [ Links ]
74. Mårtensson B, Ekselius L, Pettersson A. Treatment of depression with light therapy. A systematic literature review. SBU summary and conclusions. Lakartidningen 2008; 105(28-29): 2024-2025. [ Links ]
75. Campbell SS. Bright light treatment of sleep maintenance insomnia and behavioral disturbance. In: Lam RW, editor. Seasonal Affective Disorder and Beyond: light treatment for SAD and non-SAD conditions. Washington, DC, American Psychiatric Pub; 1998. p. 289-304. [ Links ]
76. Labbate LA, Lafer B, Thibault A, Sachs GS. Side effects induced by bright light treatment for seasonal affective disorder. J Clin Psychiatry 1994; 55(5): 189-191. [ Links ]
77. Lewitt AJ, Joffe RT, Moul DE, Lam, RW, Teicher, MH, Lebegue B, et al. Side effects of light therapy in seasonal affective disorder. Am J Psychiatry 1993; 50(4); 650-652. [ Links ]
78. Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol 2006; 74: 658-670. [ Links ]
79. Khan A, Warner HA, Brown WA. Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials. Arch Gen Psychiatry 2000; 57: 311-317. [ Links ]
80. Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: A metaanalysis of data submitted to the Food and Drug Administration. PLoS Med 2008; 5: 260-268. [ Links ]
![]() Correspondence:
Correspondence:
Mercedes Paino Piñeiro
Facultad de Psicología
Plaza Feijoo, s/n
Oviedo 33003, Spain
Tel.: +34-985-10-41-74
Fax: +34-985-10-41-44
E-mail: mpaino@uniovi.es
Received 5 December 2008
Revised 16 May 2009
Accepted 8 June 2009