Introduction
The worldwide prevalence of dementia in 2015 was 46.8 million, with the expectancy of this number to reach 131.5 million by 2050.1 In 2011, for Spain, the lifetime risk of dementia in people aged over 65 was 14.1% for men and 19.7% for women.2 Alzheimer's disease is the leading cause of dementia, followed by vascular dementia. The incidence of Alzheimer's disease in the South of Europe (Greece, Italy and Spain) in 2015 was estimated at 8.97 per 1,000 person-years, with an increase with age: from 3.43 in people aged 65-74 years old to 35.74 per 1,000 person-years in people aged over 85.3 At the same time, there is an important expected rise in the population over 65 years old in Spain, from 18.7% in 2016, to 34.6% in 2066.4 Nonetheless, effective treatments for any type of cognitive impairment still seem illusive.5 A strategy that could delay by one year the start and progression of dementia would reduce the global incidence by 9.2 million in 2050.6 Therefore, there is a solid interest in preventive measures that will slow down the progress of decreasing cognitive function. Epidemiological studies seeking to determine the impact of risk factors in the development of dementia need a reliable, valid, and efficient method of evaluating cognitive function.
The Mini Mental State Examination (MMSE)7 is widely used as a screening tool to assess cognitive function in the clinical setting.8 However, face-to-face evaluations are time-consuming and costly, and their practicality for large epidemiological studies is limited. The Telephone Interview for Cognitive Status (TICS) is a brief test of cognitive evaluation administered over the phone, intended to be used in large-scale screening and epidemiological studies.9 A modified version of the TICS (TICS-m) was developed after the inception of the original version, eliminating items that were difficult to verify over the phone and adding a delayed recall item, improving sensitivity but not adding length to the questionnaire. TICS-m has shown an excellent sensitivity (85%) and specificity (83%) in differentiating Alzheimer's disease patients and cognitively normal subjects.10
While it is important to certify that the TICS-m correctly evaluates cognitive function compared to already used and validated cognitive function tests, such as the MMSE, its most interesting feature would be the applicable prediction of decline in cognitive function over the years. The TICS-m has been validated in other studies that confirm its usefulness in the setting of large epidemiological studies, and it has also been translated into several other languages.11-15 There is no other previous validation study for the Spanish version (STICS-m), although a previous study reported on the usefulness of the STICS-m.16 This study aims to validate the Spanish translation of the questionnaire (STICS-m), using the MMSE as a standard criterion of normal cognitive function. Additionally, it tries to assess the STICS-m's ability to predict dementia cases, evaluating its utility for epidemiological studies.
Method
Subjects
We approached volunteers recruited at primary care centers in Navarre, Spain, with no relevant hearing impairment, able to understand and speak Spanish, as part of the PREDIMED Plus study. The PREDIMED Plus study is an intervention trial that evaluates the effect of an intensive lifestyle program with caloric restriction on obesity, weight loss and related conditions such as neurodegenerative diseases. The sample consisted of men between 55-75 years old and women between 60-75 years old, overweight or obese. They underwent an in-person neurocognitive assessment battery by a trained nurse, including the MMSE. Normal cognitive function, as assessed by the complete neuropsychological evaluation, was a criterion for inclusion. The STICS-m was performed by a neurologist and completed on a subgroup of these subjects within a 2-month period since the baseline MMSE.
Additionally, participants from the “Seguimiento Universidad de Navarra” (SUN) study were recruited through detailed questionnaires, which included general information about health, food habits and educational level. The SUN study is an ongoing dynamic prospective cohort of Spain university graduates focused on lifestyle issues and their relationship to disease.17 For the SUN study, 22,564 participants were recruited up to March 2017. Out of these, 1,921 participants over the age of 55 years were invited to be evaluated with the STICS-m. A subsample of 1,063 subjects accepted, out of which 933 participants completed the baseline questionnaire and 892 after two years of follow up. The diagnosis of dementia was gathered through questionnaires and medical reports, when needed, during a median follow-up time of 6.5 years. ApoE status was determined through genotyping of DNA extracted from saliva samples previously collected with the Oragene-DNA (OG-500) kit from DNA Genotek.
Cognitive assessment
-
The Mini-Mental State Examination
The MMSE is the most widely used tool for initial evaluation of cognitive function in the clinical setting. The test includes five domains: orientation; language and comprehension; registration and recall (memory); attention/calculation and praxis. The maximum score is 30, with a score above 24 considered normal and below 21 practically always denoting cognitive deficiency.8 Each domain contributes almost equally to the total score14.
-
The Telephone Interview for cognitive status-modified
The STICS-m is a translation of the TICS-m in English, which is a modified version of the TICS.10 The TICS-m includes 12 items that evaluate four cognitive domains: orientation; registration, recent memory and delayed recall (memory); attention/calculation; semantic memory, comprehension and repetition (language). The maximum TICS-m score is 51. In contrast to the MMSE, TICS-m assigns a higher proportion of the total score to the memory component.14 Some investigators prefer to use the original cognitive test, without including the delayed-recall component, giving a total of 41 points.9 Moreover, no optimal cut-off score has been established, varying between 22 and 28 points.18
The STICS-m contains the following items, in parentheses we state the amount of points given for correctly answering all parts of each item: 1) full name (2 points); 2) date (5 points); 3) address (5 points); 4) counting backward (2 points); 5) 10-word list learning exercise (10 points); 6) serial sevens backward (5 points); 7) responsive naming (4 points); 8) repetition (2 points); 9) semantic memory (current Spanish President and King, 2 points); 10) finger tapping (2 points); 11) word opposites (2 points) and 12) delayed recall of the 10-word list in task 5 (10 points).
Statistical analysis
Baseline characteristics are reported as mean±standard deviation for quantitative traits and as percentage for qualitative characteristics.
From the data gathered from the PREDIMED Plus study, the distribution of both cognitive screening test scores was plotted with histograms. The consistency between the MMSE (by personal interview) and the STICS-m (by telephone) was evaluated with an intraclass correlation coefficient (ICC) of consistency, without item number 12 of the STICS-m. The correlation between cognitive tests was evaluated with a Spearman correlation coefficient (ρ, rho). As sensitivity analysis, an ICC was calculated using the STICS-m including item number 12. Furthermore, since the memory component is more prominent in the STICS-m than in the MMSE, we also calculated an ICC using the total scores of MMSE and STICS-m without the memory items (divided into recent and delayed recall). A comparison of each domain for the MMSE and the STICS-m was also performed, not including the praxis domain of the MMSE.
From the data of the SUN cohort, we described with boxplots baseline and 2-year changes in STICS-m scores separately among participants who remained free of dementia during follow-up and among participants who developed dementia during follow-up. Changes between scores at baseline and at the 2-year follow-up were compared between patients who did and who did not develop dementia with a Student's t-test. In addition, we calculated baseline and 2-year changes in the STICS-m score among participants who developed and did not develop subsequent dementia during follow-up adjusted for ApoE (dominant model), age at baseline STICS-m ascertainment and years of university education. We also used multivariate logistic regression models to assess the association between baseline STICS-m score or 2-year changes in STICS-m score and the subsequent risk of incident dementia, adjusting for ApoE (dominant model), age at baseline STICS-m ascertainment and years of university education.
All analyses were performed using STATA SE 13.0 software.
Ethics approval and consent to participate
To obtain informed consent of potential participants, we duly informed these potential candidates of their right to refuse to participate in the SUN study or to withdraw their consent to participate at any time without reprisal, according to the principles of the Declaration of Helsinki. Special attention was given to the specific information needs of individual potential candidates as well as to the methods used to deliver their information and the feedback that they may receive from the research team. After ensuring that the candidate had understood the information, we sought their potential freely-given informed consent, and their voluntary completion of the baseline questionnaire. Participants in the cognitive function subproject of the SUN cohort provided a specific written informed consent. Participants in the PREDIMED-Plus trial provide written informed consent before entering the trial. These methods were accepted by the Institutional Review Board of the University of Navarra (Comité de Ética de la Investigación, Universidad de Navarra) as to imply an appropriately-obtained informed consent.
Results
A total of 106 participants (56% men) were included in the analysis of consistency between MMSE and STICS-m from the PREDIMED Plus study. The age of the participants at recruitment was 65±5 years. The histograms with the distribution of scores for both the MMSE and STICS-m are shown in Figure 1. The mean MMSE score was 28.4±1.6 and the mean STICS-m score was 32.4±3.8. The ICC of consistency between the MMSE and the STICS-m was 0.31 (95% confidence interval [95%CI]: 0.13-0.48) without item 12 of the STICS-m and 0.24 (95%CI: 0.05-0.41) with this item. The Spearman correlation coefficient was 0.27 (p=0.0087), after eliminating nine participants with an improbable TICS score, when compared with the MMSE score. When eliminating all memory items from both cognitive tests (recent memory and delayed recall), the ICC of consistency between the MMSE and STICS-m increased slightly to ICC=0.33 (95%CI: 0.15-0.49). The ICC of consistency between the cognitive tests for each domain was: 0.15 (95%CI:−0.04-0.33) for orientation, 0.00 (95%CI:−0.19-0.19) for recent memory, 0.36 (95%CI: 0.18-0.52) for attention/calculation, 0.14 (95%CI:−0.05-0.32) for delayed recall, and 0.21 (95%CI: 0.02-0.39) for language.
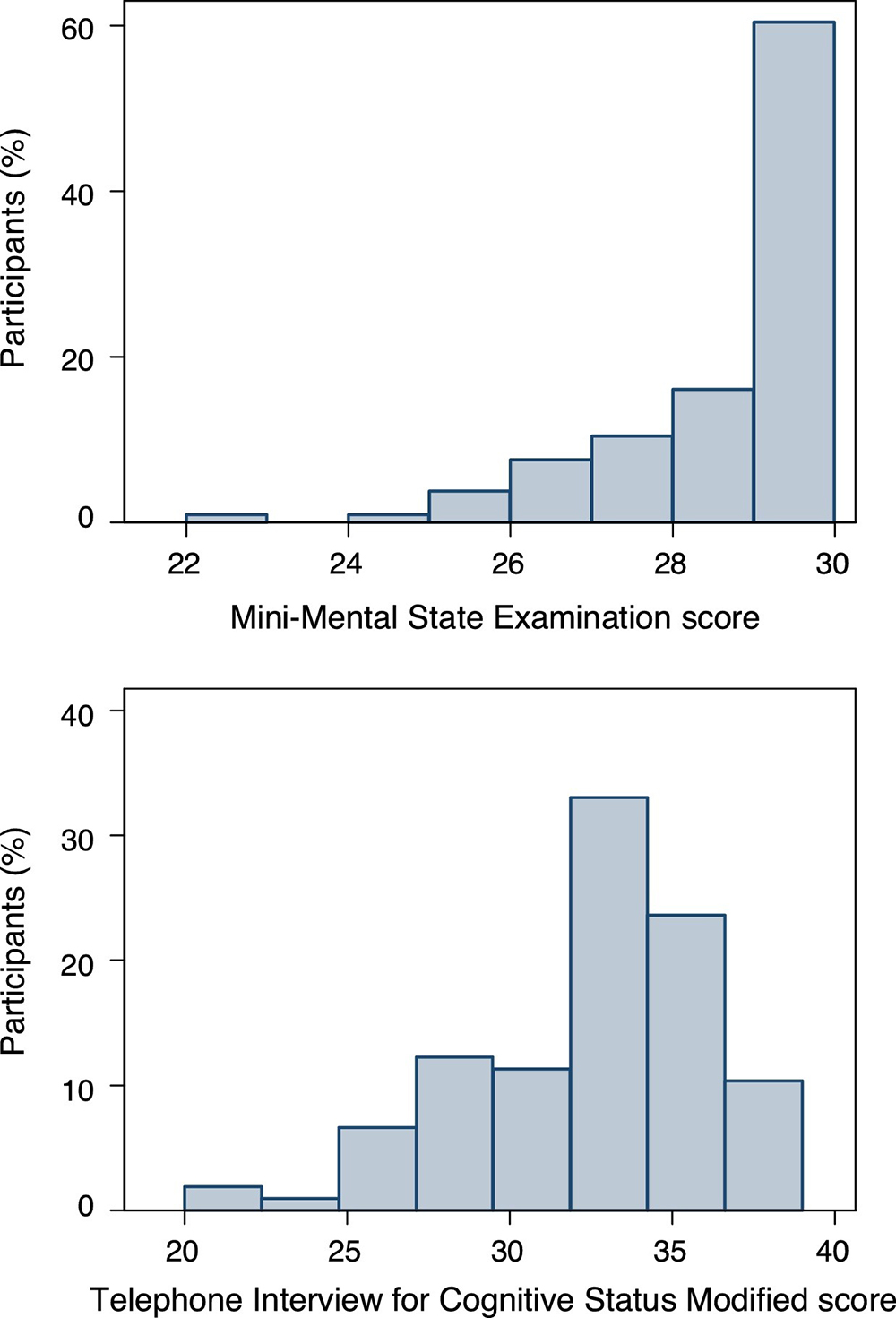
Figure 1 Distribution of scores of Mini Mental State Examination and modified Spanish Telephone Interview for Cognitive Status among PREDIMED Plus participants.
In order to assess the association between STICS-m and incident dementia, 933 participants (71% men) from the SUN project were evaluated with the STICS-m questionnaire at recruitment. One participant was excluded because of an implausible STICS-m score. Nineteen patients reported a diagnosis of dementia during a median follow-up time of 6.5 years. At the time of the first cognitive evaluation mean age was 67±6 years and the mean years of university education 5.3±1.8 years. The mean STICS-m scores at baseline in patients without dementia was 34.0±2.4 and 32.7±3.6 for patients with dementia. For participants with STICS-m evaluation after 2-years of follow-up (n=892), mean baseline age was 67±6 years. The mean STICS-m scores in patients without dementia was 34.3±2.4 and 31.5±4.6 for patients with dementia. The mean change for subjects without dementia was 0.30±2.6 and−1.8±3.5 for subjects with dementia. Figure 2 shows the distribution of the baseline and 2-year change in the STICS-m score separately for participants who developed and did not develop dementia. The unadjusted change in the STICS-m score between those who did and who did not develop dementia was statistically significant (p=0.001). Mean changes in the STICS-m score adjusted for age, year of university education and ApoE genotype (dominant model) were 0.30 (95%CI: 0.11-0.46) for participants who did not develop dementia and−1.66 (95%CI:−2.94 to−0.38) for participants who did develop dementia (p=0.011).

Figure 2 Baseline and 2-year changes in the modified Spanish Telephone Interview for Cognitive Status (STICS-m) SUN Project. Distributions are shown separately for participants who developed and did not develop dementia during a median follow-up of 6.5 years.
In the logistic regression model, the adjusted odds ratio (OR) for the development of dementia for each additional point in the baseline STICS-m score was 0.85 (95%CI: 0.72-1.02; p=0.084), adjusted for age at baseline STICS-m ascertainment, years of university education and ApoE genotype (dominant model). The OR for the development of dementia for each additional point in the 2-year STICS-m score was 0.74 (95%CI: 0.63-0.89; p=0.001). When we considered the 2-year change in the STICS-m score as exposure, the OR for the development of dementia was 0.79 (95%CI: 0.67-0.93; p=0.006).
Discussion
In the present study, we observed a weak consistency between the MMSE and the STICS-m score among participants who underwent both tests. Using data from the SUN project, adjusted mean 2-year changes in score demonstrated a maintenance of scores in patients without dementia and a decrease of almost 2 points in patients who subsequently developed dementia. The logistic regression model showed that for each additional point in the STICS-m score at year 2 of follow-up and in the 2-year change in score, the risk of developing dementia decreased by 26% and 21%, respectively. Therefore, despite the low ICC with the MMSE, the STICS-m appears to correctly differentiate people with a higher probability of developing dementia in longitudinal studies.
Previous validation papers have reported moderate to high correlation between the STICS-m and the MMSE with the use of Pearson (r) or Spearman (ρ) correlation coefficients. In our study, ρ=0.27 (p=0.0087). The original TICS was reported to have a r=0.94 (p<0.0001), which was evaluated on a population of mainly Alzheimer's disease patients.9A validation of the German TICS-m showed a ρ=0.48 (95%CI: 0.36-0.58) in a population study of people aged 70 years or older.19 A third study, with a sample of relatively high functioning adults, found a ρ=0.57 (p>0.001).14 Nonetheless, none of the aforementioned studies reported the ICC. The ICC of consistency is probably a better measure of agreement between diagnostic tests, since the correlation coefficients only measure association, while the ICC is an expression of the cognitive test's ability to persistently orientate subjects as either cognitively normal or impaired.20
The low correlation between the MMSE and the STICS-m is probably due to the population of our study, combined with the characteristics of the cognitive tests. The PREDIMED Plus sample, in which the both MMSE and STICS-m were performed, consisted of cognitively normal adults, which is confirmed by the high mean scores in both the MMSE and the STICS-m. The MMSE can be less sensitive to cognitive changes in high functioning individuals, a phenomenon known as the ceiling effect.21 This, combined with the sparser distribution of the STICS-m scores in comparison to the MMSE, as represented by the histograms and standard deviations, might have accounted for the low ICC. Furthermore, the memory and registration component of the TICS-m accounted for 20 out of the 51 points (vs. 6 out of 28 on the MMSE), which may enhance the sensitivity of this test to detect early cognitive dysfunction,22 but increase the differences between cognitive tests.14 Therefore, the low correlation can be partly justified by the fact that the MMSE does not identify well early memory deficits while the TICS-m has a more thorough memory evaluation. For this reason, we eliminated item 12 for our analysis, which allows for a better comparison between memory domains (10 out of 41 points in the STICS-m vs. 6 out of 28 in the MMSE).
The data from the SUN study suggests the practical utility of the STICS-m for epidemiological studies. While these cognitive tests are frequently used to classify subjects as cognitively normal or impaired according to score, we used the STICS-m as a quantitative variable to predict the development of dementia. While not statistically significant in this sample, a higher baseline STICS-m score appears to predict a lower probability of developing dementia. The multivariate logistic regression model indicates that each additional point in 2-year change in STICS-m score decreased the risk of developing dementia by 21%. Therefore, even as the correlation with the MMSE is weak, the STICS-m score appears to be a suitable tool to detect change in cognitive function over the years. A review of telephone-administered screening tests for dementia diagnosis states that it is more clinically relevant that a screening method indicates correctly whether an individual is likely to have dementia, rather than correlate well to another brief screening measure.23
There are other advantages of using the STICS-m over the MMSE or other in-person cognitive tests in large epidemiological studies. The TICS-m is a more efficient tool and has been shown to reduce selection bias, as it allows recruiting people over larger areas, and enables follow-up. Even as the use of telephone screening methods are not entirely homogenous,24 the advantages of using telephone interviews may outweigh their methodological limitations.25 The STICS-m can also be performed in visually-impaired populations and participants may find a cognitive telephone interview less threatening than in-clinic assessments, leading to lower dropouts and more complete data collection.14
Some strengths and limitations in our study deserve to be mentioned. A potential limitation in this work is the lack of comparison of the STICS-m to a neuropsychological or clinical evaluation of the participants in the two samples. In the PREDIMED Plus sample, this would have allowed to compare the STICS-m to a more suitable gold standard of dementia diagnosis, rather than the MMSE, and calculate measures of sensitivity and specificity. Another possibility could have been correlating the memory component of the neuropsychological tests to the STICS-m. Furthermore, the first sample (undergoing both MMSE and STICS-m) was only evaluated with STICS-m at one point in time and no data on ApoE status were available. In the SUN project, no MMSE was performed, although a similar correlation as seen in this study would have probably been found since this population of university graduates can be described as high-functioning. Another limitation is that the number of patients that developed dementia in this cohort was low. However, despite the low number of dementia cases, the change in STICS-m over 2-year follow-up when comparing patients with and without dementia was statistically significant. Since the high-functioning and high-level of education profiles of both samples might explain the low correlation between cognitive tests, further investigations with the STICS-m in samples with different characteristics are warranted.
Within the strengths of our study is the performance of the telephone questionnaire by a single neurologist for the first sample, which demonstrates both quality and consistency in the cognitive evaluation. Another positive aspect of our study is the long-term follow up of the SUN project, as few validation papers observe the change or stability in TICS over a long period of time. Furthermore, the information gathered for the SUN cohort, although self-reported, has been determined to be reliable by a series of studies that established the reproducibility of the questionnaires and some self-referred diagnosis, such as hypertension, depression and metabolic syndrome.26-28
Conclusion
In summary, the STICS-m can be regarded as a useful tool in the epidemiological setting. Previous validation studies in multiple languages ascertain its value as a screening tool for dementia diagnosis and this study confirms its -albeit low- correlation to in-person cognitive assessment, while also providing evidence of its ability to predict cognitive decline.
What is known about the topic?
The modified Telephone Interview for Cognitive Status (TICS-m) is a screening tool for cognitive function that has advantages over face-to-face evaluation, especially in the context of epidemiological studies. The TICS-m has been validated in several languages, demonstrating it has diagnostic validity (good sensitivity and specificity) and concurrent validity, in comparison to other cognitive tests widely used in the clinical setting, like the Mini-Mental State Examination. In large epidemiological studies, it allows the evaluation of cognitive function at a larger scale, in order to establish potential associations between risk factors and cognitive decline, essential to implement primary prevention measures against dementia. Hitherto, there has not been a validation study of the Spanish version of TICS-m.
What does this study add to the literature?
Even though we have found a low consistency between the results of the Mini-Mental State Examination and the Spanish version of modified Telephone Interview for Cognitive Status (STICS-m), the score of the questionnaire seems able to predict a greater risk of developing dementia. Therefore, the questionnaire allows the study of the relationship between cognitive function and lifestyle factors. The STICS-m has been used in the “Seguimiento de Universidad de Navarra” cohort of Spanish university graduates, which has gathered information on lifestyles. The study of the relationship between cognitive function and exercise, dietary patterns and cardiovascular risk factors in this cohort can expand current knowledge on potential preventive measures against cognitive decline, in a context where this disease will be more and more prevalent as the population ages.














