Introduction
Rare diseases (RDs) are diseases that affect a small number of people, with a prevalence of less than or equal to 1 person per 2,000. These are characterized by being chronic, progressive, with high morbi-mortality and a high degree of disability (Federación Argentina de Enfermedades Poco Frecuentes [FADEPOF], 2018).
When detected in childhood, the family of the person with RD plays a fundamental role (Cardinali et al., 2019). The moment of diagnosis can be a traumatic experience, causing alterations at the emotional, behavioral, and psychopathological levels (López, 2019). Likewise, there are constant worries, feelings of uncertainty, and the need to anticipate limitations or losses that the child may experience (Zaher, 2012).
In turn, the family, and whoever assumes the role of primary caregiver, modifies their daily routine and learns to live with the disease (Zaher, 2012). The primary caregiver usually has a significant burden, affecting their well-being and quality of life (Tramonti et al., 2019). Due to the complexity involved for a family living with an RD and the lack of systematic reviews on this issue, this study aimed to review the scientific evidence on family functioning in families who have a child with an RD.
Method
Design
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed to conduct the systematic review (Page et al., 2021).
Search Strategies
The search was conducted in May 2022 in the Pubmed and EBSCO databases, and in the Google Scholar search engine. The search strategy used, both in Spanish and English, was: ("family functioning" OR "family dynamics" OR "parenting styles" OR "parental styles" OR "parents") AND ("rare diseases" OR "neuromuscular diseases" OR "inborn errors of metabolism" OR "lysosomal diseases" OR "congenital malformations" OR "congenital anomalies" OR "mucopolysaccharidosis" OR "spinal muscular atrophy" OR "Duchenne muscular dystrophy"). A filter was applied with respect to year of publication (2012-2022) and language (Spanish and English) in the databases that allow it.
Study Selection and Eligibility Criteria
Only empirical articles published in Spanish or English, published between 2012 and 2022 that addressed the population of families of children with a diagnosis that could be classified as RD were included. Once the search was completed, we proceeded to read the title to filter out any documents that were not relevant to the topic; then, we read the abstract of the remaining articles and applied the inclusion criteria, until we reached the final sample of the review. Finally, we proceeded to a critical reading of the documents, with the aim of extracting data on the RD populations studied, the instruments used, and the main results found.
Results
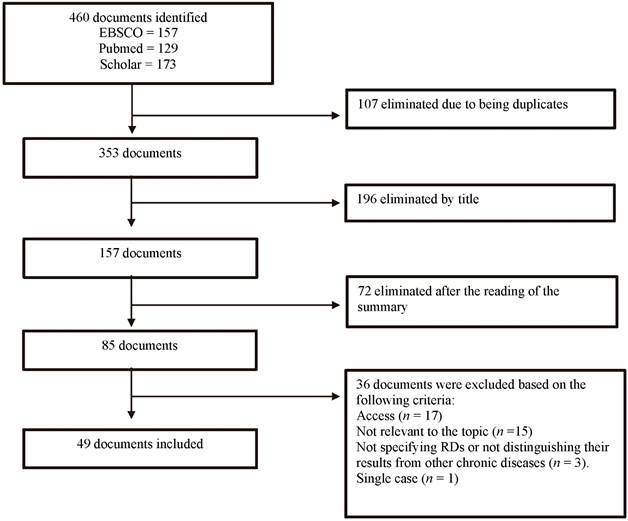
Initially 460 articles were found from which 49 research articles on family functioning in families with a child with an RD were selected (Figure 1). The description of the 49 selected studies, including the country in which they were conducted, the study sample, and the instruments used are shown in Table 1.
Table 1. Description of the Studies Included in the Systematic Review
| Citation | Country | RD | Sample | Instrument |
|---|---|---|---|---|
| Baiocco et al., 2017 | Italy | Duchenne Muscular Dystrophy | 23 mothers and 16 fathers of children (6-14 years old) | Family Adaptability and Cohesion Evaluation Scales interview |
| Baumbusch et al., 2019 | Canada | Rare Diseases | 15 mothers and 1 father of persons (up to 20 years old) | Semi-structured interview |
| Boettcher et al., 2020 | Germany | RD with mechanical ventilation | 75 families of children (under 21 years) | The Ulm Quality of Life Inventory for Parents, The Brief Symptom Inventory, The Coping Health Inventory for Parents, The Oslo-Social Support Scale, The Family Assessment Measure |
| Boettcher et al., 2021 | Germany | Congenital surgical diseases | 107 mothers and 97 fathers of children | The Family Assessment Measure, The Oslo-Social Support Scale, Impact on Family Scale |
| Brenner et al., 2016 | Canada | Congenital malformations | 1,675 families with parents together with children with and without congenital malformations | Quebec Longitudinal Study of Child Development |
| Campos et al., 2021 | Argentina | Phenylketonuria | 30 children aged 8 and 11 years with diagnosis and control group | Children's Coping Questionnaire, Scale Perception of the Relationship with Parents |
| Currie & Szabo, 2019a | Canada | RD | 15 parents under 15 years of age | Semi-structured interviews |
| Currie & Szabo, 2019b | Canada | RD | 11 mothers, 4 fathers of children under 11 years of age | Semi-structured interviews |
| Currie & Szabo, 2020 | Canada | RD | 11 mothers, 4 fathers of children under 11 years of age | Semi-structured interviews |
| Fonseca et al., 2012 | Portugal | Congenital anomalies | 44 couples parents of children with anomalies, 46 couples parents of healthy children | Brief Symptom Inventory 18, Maternal Confidence Questionnaire |
| Golfenshtein et al., 2017 | United States | Congenital heart disease | 129 parents of children with congenital heart disease and parents of healthy children | Parenting stress index-long form |
| Gramer et al., 2013 | Germany | Metabolic disorders | 189 parents | Questionnaire |
| Grant et al., 2012 | United Kingdom | Mucopolysaccharidosis type III | 16 mothers and 7 fathers of children with MPS III; 20 mothers and 3 fathers of children with intellectual disabilities | The Resilience Scale for Adults, Brief COPE |
| Hjorth et al., 2021 | Sweden and Denmark | Spinal Muscular Atrophy type 1 and 2 | 95 parents of children | Interview |
| Ho et al., 2021 | China | Neuromuscular diseases | 21 fathers and 59 mothers of children (up to 18 years of age) | PedsQL™Family Impact Module, Parental Stress Scale |
| Holm et al., 2021 | Denmark, Spain, Poland, Italy | Congenital anomalies | 43 mothers, 15 fathers and 2 child caregivers | Interviews and focus groups |
| Johnson et al., 2018 | United Kingdom | Dysmelia | 11 mothers and 9 fathers of children up to 5 years of age | Semi-structured interview |
| Khair & Pelentsov, 2019 | United Kingdom | Hemorrhagic disorder | 99 fathers and 132 mothers of children from 0 to 17 years of age | Parental Needs Scale for Rare Diseases |
| Lamb et al., 2016 | United States | Rett syndrome | 400 primary caregivers | Efficacy component of the Parenting Skills of Competence Scale, Ways of coping Checklist revised, Family Assessment Measure III, Psychological Adaptation Scale |
| Liang et al., 2019 | China | Duchenne muscular dystrophy | 13 families with 15 children (2-18 years old) and 15 unaffected families | PedsQLFIM - PedsQL |
| Long et al., 2021 | Australia | Diagnosed mitochondrial respiratory chain disorder | 14 patients, 12 parents (3 of them also have a diagnosis) | Focus groups |
| Magliano et al., 2014 | Italy | Duchenne and Becker muscular dystrophies | 336 parents of patients with DMD (246) and BMD (90) | Family Problems Questionnaire |
| Miodrag & Peters, 2015 | United States | Angelman Syndrome | 124 parents of individuals (0 to 27 years old) with Angelman Syndrome (99 with deletion I and II, 11 with IC defects, 14 UPD) | Parenting Stress Index |
| Needham et al., 2013 | United States | Mucopolysaccharidosis type II | 74 caregivers and 21 patients | PedsQL FIM, supplemental questionnaire |
| Neumann et al., 2021 | United States | Short bowel syndrome | 13 mothers and 4 fathers of children (0 to 19 years old) | Family Management Measure |
| Obeidat et al., 2021 | Jordan | Duchenne muscular dystrophy | 20 parents (10 pairs) of children (average age 14 years) | Interview |
| Ortega, 2020 | Argentina | Duchenne muscular dystrophy | 4 mothers, 2 fathers, and 2 other relatives of children | Family Cohesion and Adaptability Assessment Scale, MOS Social Support Scale. |
| Ortega et al., 2022 | Argentina | Neuromuscular diseases | 35 families of children (1 to 18 years) | Psychological Adaptation Scale and Adult Self-Report Questionnaire, The Adult Self Report |
| Pangalila et al., 2012 | Netherlands | Duchenne muscular dystrophy | 80 parents of 57 adults | EuroQOL, Utrecht Coping List, General Self-efficacy Scale |
| Pasquini et al., 2021 | United States | Leukodystrophies and spinal muscular atrophy | 15 parents, 4 with children with metachromatic leukodystrophy, 10 with children with SMA and 1 with two children with SMA. | Semi-structured interviews |
| Pfeiffer et al., 2021 | United States and Spain | Achondroplasia | 14 mothers, 1 father of children under 2 years of age | Focus groups and interviews |
| Picci et al., 2015 | Italy | RD | 30 mothers and 25 fathers of children under 18 years of age with RDs and 30 mothers and 26 fathers of children under 18 years of age with chronic illnesses | The Satisfaction With Life Scale, The Profile of Mood States, The Coping Orientation to Problem Experienced, The Hamilton Rating Scale for Depression, The Hamilton Rating Scale for Anxiety |
| Porter et al., 2020 | United States | Mucopolysaccharidosis type III | 19 mothers and 6 fathers of individuals from 4 to 36 years of age | Focus groups and questionnaire |
| Qian et al., 2015 | United States | Spinal Muscular Atrophy | 21 patients, 64 parents, 11 specialized clinicians | Focus groups |
| Ragusa et al., 2020 | Italy | Prader Willi Syndrome | 21 children and adolescents with Prader-Willi syndrome, 34 adults and 138 caregivers | Written interviews |
| Rozensztrauch et al., 2019 | Poland | Esophageal atresia | 73 parents of children (aged 1 month to 18 years) who had esophageal atresia surgery | PedsQL™ Family Impact Module |
| Saetrang et al., 2018 | Norway | Duchenne muscular dystrophy | 12 families of children (from 7 to 17 years old) | Interviews |
| Sjöberg et al., 2020 | Sweden | Upper and/or lower limb impairment | 12 mothers and 5 fathers of children (average age 5.9 years) | Semi-structured interviews |
| Somanadhan & Larkin, 2016 | Ireland | Mucopolysaccharidosis | 8 parents of individuals (0-24 years) | In-depth interviews |
| Somanadhan et al., 2021 | Ireland | Mucopolysaccharidosis | 8 parents of individuals (0-24 years) | In-depth interviews |
| Sulmonte et al., 2020 | United States | Duchenne Muscular Dystrophy | 10 parents of children with DMD who also have other unaffected children ages 8 to 17 years old | Interviews |
| Trawicka et al., 2019 | Poland | Marfan syndrome and juvenile idiopathic rheumatoid arthritis | 25 adolescents with Marfan syndrome, 29 with JIA, 20 without chronic disease | Family Assessment Scale, Child Behavior Checklist, Youth Self-Report |
| Turan et al., 2019 | Turkey | Duchenne and Becker Muscular Dystrophy | 28 children and adolescents with DBMD and 50 healthy control group. 8.11 mean age of patients | Kiddie-Sads-Present and Lifetime, the Beck Depression Scale, State-Trait Anxiety Inventory, Parental Attitude Research Instrument, the Child Behavior Checklist, Family Assessment Device |
| Vitale, 2016 | United States | Prader Willi Syndrome | 15 mothers and 5 fathers of children (2 to 17 years old) | Interviews |
| Von Gontard et al., 2012 | Germany | Spinal muscular atrophy | 96 children and adolescents with SMA aged 6 to 18 years and 59 controls | Questionnaire on Resources and Stress, Family Crisis Orientated Personal Evaluation Scale, the F-SOZU questionnaires |
| Waldboth et al., 2021 | Switzerland | Neuromuscular diseases | 10 young people (14-30 years old) with ENM and 21 family members | Interviews |
| Yamaguchi & Suzuki, 2014 | Japan | Duchenne muscular dystrophy | 18 parents with children aged 15 to 30 with NMD | Semi-structured interviews |
| Yang et al., 2016 | Taiwan | Spinal muscular atrophy type I and II | 19 parents with children with SMA | Interviews |
| Zengin et al., 2020 | Turkey | Mucopolysaccharidosis | 8 parents with children (n=10) with a mean age of 8.8 | Semi-structured interviews |
From the review of these articles, the results were organized into the following themes: impact of the diagnosis (N=18); role of the primary caregiver (N=8); family functioning (N=20); impact on the emotional sphere (N=7); effects on marital and social life (N=8); coping strategies (N=3); and family and the health care system (N=7). The results for each theme will be presented below.
Impact of the Diagnosis
The articles reviewed on the impact of the diagnosis allow us to establish that the diagnosis, the communication, and the moment of detection of an RD are prominent influencing factors. Regarding communication, parents often point out the lack of time and sensitivity on the part of physicians, which generates a negative experience of that moment (Qian et al., 2015). When they receive an early diagnosis, parents generally have greater tools to accept it; they have some emotional readiness and greater organization (Johnson et al., 2018; Qian et al., 2015)
Receiving a diagnosis of an RD has an emotional impact on parents. Ambivalence about treatment decisions and consequently feelings of anxiety and uncertainty arise (Sjöberg et al., 2020). Then, thanks to knowledge and adequacy in their role as caregivers, parents gain confidence in their management of the disease, becoming experts and feeling able to teach and educate others (Khair & Pelentsov, 2019; Somanadhan et al., 2021). Parental coping can be improved by increasing intra- and extrafamilial resources and decreasing perceived family stress in mothers (Boettcher et al., 2021).
Upon diagnosis, parents report experiencing a change in status from being parents of a healthy child to parents of a child with an RD. Parents highlight the uncertainty regarding the future and express the emotional and painful struggle they go through when dealing with a progressive and fatal condition (Boettcher et al., 2020; Somanadhan et al., 2016; Somanadhan et al., 2021). In some cases, parents face the challenge of a premature death, where the desire to see their child grow up transformed into the fear of death (Obeidat et al., 2021; Qian et al., 2015; Yang et al., 2016).
Parents cite constant concern about their child's future, emotional and physical health, social well-being, and ability to function independently (Holm et al., 2021; Pfeiffer et al., 2021). Furthermore, parents have the responsibility to find trained caregivers and obtain the necessary adaptations, monitor their child to avoid complications, advocate for their children, and educate others about the disease. This responsibility can be overwhelming, and it can lead to parental hypersensitivity and hypervigilance (Long et al., 2021; Pfeiffer et al., 2021).
Role of the Primary Caregiver
Regarding the caregiver role, it is mothers who usually adopt the primary caregiver role, while fathers provide secondary care. Thus, while mothers are responsible for meeting the child's basic needs, fathers assist mothers and take care of activities that require strength (Obeidat et al., 2021).
Primary caregivers report fatigue, stress, social isolation, and insomnia (Obeidat et al., 2021). In turn, an impact on the work environment appears, which can be experienced as a loss of power and the feeling of not being able to be away from home and enjoy one’s time (Baumbusch et al., 2019; Obeidat et al., 2021; Pfeiffer et al., 2021; Ragusa et al., 2020).
In addition to the impact on labor, there is the financial expense involved in accessing medications, benefits, and services (Gramer et al., 2013; Khair & Pelentsov, 2019). Because of this, there are families who receive some financial assistance from the government, or unpaid support from family or friends. Other families report unmet needs, and some of them are unaware of the possibility of receiving government support or do not qualify for it (Jones et al., 2018).
Family Functioning
Studies that described family functioning seem to indicate that it is affected by the symptoms of the disease, the care needs, and the impact created from receiving a diagnosis (Currie & Szabo, 2019a; Turan et al., 2019). The presence of an RD affects the family on an emotional level, sometimes there is also an impact on the social, cognitive, and communication domains (Rozensztrauch et al., 2019). Often parents face difficulties in expressing their emotional and psychological problems in the family (Obeidat et al., 2021).
Some families report positive changes in terms of family dynamics: strengthening of family bonds, perspective taking, and focus on the present and the positive, enjoyment of small victories, modification of personal values, and an improvement in their ability to perform challenging tasks and handle difficult situations (Neumann et al., 2021; Obeidat et al., 2021; Pfeiffer et al., 2021).
Regarding family functioning, studies revealed that families exhibit good levels of family cohesion-i.e., being connected or semi-connected-(Ortega, 2020) and that adolescents perceive their families as cohesive and flexible (Trawicka et al., 2019). It has been shown that dysfunctional functioning, with greater disconnection and poorer communication and family satisfaction correlates with behavioral problems in adolescents (Trawicka et al., 2019).
Single caregiver assignment and the child's level of disability have been found to be associated with lower levels of family functioning (Brenner et al., 2016; Liang et al., 2019; Needham et al., 2013). In contrast, better scores were obtained when the diagnosis was received by the firstborn (Brenner et al., 2016). In turn, parental self-efficacy, problem-focused coping, and emotion-focused coping correlate positively with family functioning (Lamb et al., 2016).
Family functioning and well-being are threatened due to recurrent stress and the constant risk of mental disorders (Vitale, 2016; Waldboth et al., 2021). An important period is the transition to adulthood, where lack of information can make it difficult to maintain good family functioning and well-being (Yamaguchi & Suzuki, 2014). Regarding siblings, relationships were found to include arguments and teasing, however, also learning CPR, and medication management (Sulmonte et al., 2020).
Family functioning may be the most important predictor of quality of life and mental health (Boettcher et al., 2020). The following were found as resources that promote psychological health: maintaining employment, being active, going to church, attending therapy, having the support of family, friends, and patient family groups (Needham et al., 2013). Many parents advise focusing on the healthy aspects and not just being focused on care and treatment (Hjorth et al., 2021; Holm et al., 2021).
Impact on the Emotional Sphere
At the emotional level, the findings indicate similar levels of depression upon diagnosis of an RD, compared to the diagnosis of chronic diseases. High levels of anxiety and the appearance of fear, insomnia, and depressive mood were found (Picci et al., 2015). In turn, it was concluded that stress levels vary according to the child's RD or disability, and this decreases levels of quality of life (Liang et al., 2019; Miodrag & Peters, 2015; Needham et al., 2013).
One study concluded that the main object of concern is the frequent sense of loss, the feeling of inadequacy to handle the situation, and the conviction that the whole family is influenced by the patient's condition (Magliano et al., 2014).
Effects on Marital and Social Life
After the onset of a diagnosis, marital relationships can become strained (Somanadhan et al., 2016). Lack of personal or social time, constant stress, both financial and related to finding qualified personnel were identified as marital stressors (Grant et al., 2012). Many parents recommend planning couple time to decrease stress in their relationship (Vitale, 2016).
The social sphere is another area of compromise. Extrafamilial relationships can be difficult to sustain (Ragusa et al., 2020). There is evidence of social limitation, experiencing stigma, or being ignored (Pfeiffer et al., 2021; Zengin et al., 2020), and the need to be available to their children all the time (Obeidat et al., 2021). The impact on vacations or other activities, which must be limited or adapted, is mentioned (Pfeiffer et al., 2021). Nevertheless, families mention that, over time, they become more adaptive (Obeidat et al., 2021). On the other hand, families receive support from other family members and friends and also develop friendships with patient families, often through organizations (Pfeiffer et al., 2021).
Coping Strategies Used by These Families
In terms of coping strategies used by parents, a predominance is found in emotion-focused mechanisms, trust in God, and life after death (Zengin et al., 2020), and less attention is paid to long-term goals and future planning (Grant et al., 2012). One study concluded that while parents of children with RD turned mostly to religion, parents of children with other chronic conditions focused on active planning, seeking instrumental social support, and positive reinterpretation (Picci et al., 2015).
Health System
The care required by the disease must be included in the family dynamics. In some cases, routines are developed to successfully manage medical care (Neumann et al., 2021). There is a need for other children to achieve independence quickly to assume a supportive role (Porter et al., 2020).
Family dynamics may be affected by spending periods of time in the hospital. Additionally, while the home experience feels like a space of comfort and safety (Somanadhan et al., 2016), for those receiving extra help, a loss of boundaries within private spheres may be experienced (Currie & Szabo, 2019b).
Difficulties were encountered with social security in accessing the necessary services, and, consequently, the need for constant exchanges with social security representatives was also found (Pasquini et al., 2021). Likewise, the lack of coordination among health professionals contributes to the delay in access to benefits. The effort involved in the constant struggle with the social work is a burden for parents, and they experience it as exhausting (Baumbusch et al., 2019; Currie & Szabo, 2019a, 2019b).
Discussion
The aim of the present study was to review the literature related to the coexistence of a family with a diagnosis of RD. The existing literature revealed that family functioning is modified after the diagnosis of an RD in a family member. Due to the presence of the disease and because of its manifestation, it is necessary to reorganize roles, functions, and family routine, necessitating adaptation and emotional adjustment (Baumbusch et al., 2019; Currie & Szabo, 2019a; Neumann et al., 2021; Obeidat et al., 2021; Pfeiffer et al., 2021).
The results of this review showed a negative impact on marital life; lack of personal time, constant stress, and financial stress appeared as stressors (Grant et al., 2012). On the other hand, families mentioned a change in the way of coping with situations (Neumann et al., 2021; Obeidat et al., 2021; Pfeiffer et al., 2021; Porteous et al., 2021). In turn, regarding navigating the health system, some parents mentioned difficulties in accessing health services and in generating coordination between professionals, spending long periods of time in the hospital, and encountering health personnel at home (Currie & Szabo, 2019b; Somanadhan et al., 2016).
Family functioning can play a key role in the psychological health of caregivers. Parents need to be provided with the right information and treated with empathy. It is essential that health professionals make interventions in pursuit of the family's needs and capabilities (Boettcher et al., 2020; Saetrang et al., 2018; Sjöberg et al., 2020; Turan et al., 2019).
In this sense, based on the conclusions of this review, it is recommended that psychologists or health professionals who assist family members of people with rare diseases attend to the stressors present after diagnosis and encourage adaptive coping strategies. At the same time, it is suggested to work in an interdisciplinary manner with other treating professionals to facilitate families navigating the health care system. Addressing family risk aspects would be a way of working towards a better quality of life, both for the diagnosed person and his/her family.
This paper shows that most of the studies included were carried out in the United States, Germany, and other European countries. Only two Ibero-American studies were identified that explored this topic-in Argentina and Spain. This limitation indicates the need to promote research on family aspects in the Ibero-American population. Regarding the diseases studied, a limitation arose because the studies found were based on particular diseases or groups of diseases, demonstrating the scarcity of studies that address these issues in RDs as a heterogeneous set of diseases.
From the search focused on family functioning, a great variety of topics related to the family life of people with RDs emerged. Thus, the fundamental role played by the family in the treatment of children with RDs and the complexity of carrying out a family-centered approach is evident. Interdisciplinary work with the family should be considered and the family's resources, including family functioning, should be taken into account.
Based on this work and the scarcity of information in the Latin America region, it is considered relevant and necessary to investigate the family functioning of families with children with RDs in the Argentine population. At the same time, in view of the importance of the moment of communication of the diagnosis, it is proposed to carry out a psychoeducational communication model that accompanies the genetic counseling process, evaluating its impact on family functioning.