Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO  Similares en Google
Similares en Google
Compartir
Archivos de la Sociedad Española de Oftalmología
versión impresa ISSN 0365-6691
Arch Soc Esp Oftalmol vol.80 no.3 mar. 2005
EDITORIAL
DRY EYE - IS THIS A DISEASE OR A NATURAL CONSEQUENCE OF AGING?
OJO SECO: ¿ENFERMEDAD O CONSECUENCIA NATURAL DE LA EDAD?
MICHAEL E. STERN, Ph.D1
The prototypical dry eye patient is a peri- or post-menopausal woman or middle aged man who presents at the ophthalmologists or optometrists office complaining of chronic ocular surface pain and foreign body sensation. Due to the persistence of symptoms and lack of satisfaction with suggested therapies, these patients tend to see several ophthalmic professionals in search of help. The typical response these patients have heard from their doctor is: «you're getting older and your lacrimal glands are not working as well as they have in the past. This is very common and you are just going to have to live with it, however you should try artificial tears to see if they help». This is unsatisfactory to both the patient and physician. To the patient, this disease has a significant negative impact on their quality of life.
As the population ages, the financial realities and medical necessities have forced the research community to place emphasis on diseases that impact this demographic group. It is no longer suitable to view diseases such as Dry Eye, which have age as a risk factor, as a «normal» part of the aging process. In 1989 when I first started to focus on this area, the first understanding we came to was that this is in fact, a disease. It is not «a normal part of aging» -it has an associated pathology from which specific therapeutic targets can be elucidated.
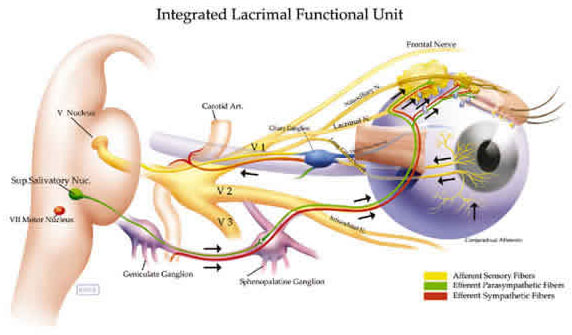
Since 1989, there have been several important findings from several excellent laboratories which have supported the «Unified Theory» paper which was published in 1998. In this paper we discussed the secretion of tears through the Lacrimal Functional Unit (LFU) consisting of the ocular surface (cornea, conjunctiva), the main and accessory (Wolfring and Krause) lacrimal glands and the interconnecting enervation (Stern et al., 1998). Proper functioning of the LFU is required to secrete tears of normal composition which helps to maintain a normal homeostatic environment for the epithelia of the ocular surface.
It is now known that there are two major factors in helping to maintain the tissues and function of the LFU. The first is the presence of circulating androgens. David Sullivan at the Schepens Eye Research Institute demonstrated that androgens help to maintain an «anti-inflammatory umbrella» over the tissues of the LFU (Sullivan and Edwards, 1997; Rocha et al., 1998; Sullivan et al., 2002). Androgens are «steroid-like» hormones which have anti-inflammatory properties. As we age, or with specific pathologies, the systemic levels of androgens decrease. This is especially critical in women who have lower levels of androgens in the normal state.
The second factor involved in protecting the LFU is the immune system. Immunovigilant T-cells migrate through the lacrimal glands in search of problems such as inflammation. In the normal individual, these cells will undergo apoptosis (programmed cell death) while leaving the glands enroute to local lymph nodes. In the inflamed eye, the epithelial cells of the lacrimal glands and ocular surface are capable of expressing antigens on their surface which will bind to the lymphocytes and prevent apoptosis and cause them to activate and secrete a profile of cytokines which will result in the tissue inflammation seen in Dry Eye.
An individual whose androgen levels decrease below a threshold level, such as the post-menopausal woman or man who is taking anti-androgen drugs as therapeutics for androgen problems, become susceptible to Dry Eye. If this individual, who cannot inhibit inflammation normally, is placed in an adverse environment with low humidity, wind or has allergies or an ocular surface viral infection, this results in increased neural traffic throughout the LFU. Inflammation at the neural-epithelial junction in the lacrimal glands results in antigen presentation to the epithelial cell surface. This is noticed by the trafficking lymphocytes (T-cells) which bind to the epithelial cells and become activated. They abort their normal apoptosis program and become activated, secreting multiple cytokines which serve to inflame the tissue and recruit additional T-cells.
This «ramping up» of the inflammation within the ocular surface results in the secretion of an «inflammatory soup» onto the ocular surface which then becomes inflamed. Cytokines secreted by the conjunctival epithelial cells serve to recruit T-cells into the conjunctiva as well resulting in a chronic inflammation at both ends of the LFU. It is this ocular surface inflammation and the inability to maintain a normal homeostatic environment on the ocular surface which results in the syndrome known as Dry Eye (Pflugfelder, Beuerman and Stern, 2004).
Symptomatically, this certainly fits the definition of a chronic pain syndrome. Although symptoms may vary during the day, the patients are in constant pain and are relegated to thinking about their eyes all day which makes many otherwise routine daily tasks more difficult. A large percentage of these patients become clinically depressed and require systemic anti-depressive therapy.
With the advent of the Unified Theory, the goals of therapy changed dramatically from simply trying to keep the ocular surface wet to re-establishing the patient's ability to secrete normal tears and maintain a normal ocular surface environment. To achieve this, one must first eliminate the inflammation within the LFU. Current therapies include 1) topical cyclosporin A which is used to inhibit T-cell activation and allow the inflammation to decrease with the population of activated T-cells and 2) pulse dosing with topical steroids to eliminate the secretion of inflammatory mediators and the population of activated T-cells. Additionally, therapies which induce the secretion of mucin are being tested in clinical trials.
As a clinician, one must internalize a new understanding of the clinical picture of inflammation. This has been traditionally thought to be a red eye at the slit-lamp. In many cases ocular surface's have been shown to be highly infiltrated with CD4 positive T-cells while still looking «white» under examination. Patients with Sjogren's syndrome tend to have white ocular surfaces. Inflammation should be understood to be a cellular process resulting in the secretion of pro-inflammatory cytokines. The key sign to look for in patients is chronicity. If an individual spends the day working with their computer and they need a few drops of artificial tears to soothe their eyes - this is not a chronic disease. However, if a patient is using Artificial Tears four times or more per day, every day, then they most likely have a chronic inflammatory process. It has been previously shown that this type of inflammation can induce abnormal apoptosis (programmed cell death) in the all important cells of the ocular surface and lacrimal glands (Gao et al., 1998; Brignole et al., 2000). It is important that treatment be initiated to reverse the course of this inflammation before the patient becomes much worse.
The lessons that medical research have provided us as scientists and clinicians over the past fifteen years are that many diseases have age as a risk factor. This does not however indicate that we should attribute these diseases as a fact of age and allow them to proceed. The pathology of each disease needs to be thoroughly researched in order to develop effective therapeutics to restore and maintain good quality of life. We have made a good start for individuals with Dry Eye, elucidating the inflammatory nature of this syndrome, however the future will hold more targeted therapeutics.
1 Senior Research Investigator. Allergan, Inc.
E-mail: stern_michal@allergan.com
REFERENCES
1. Brignole F, Pisella PJ, Goldschild M, De Saint Jean M, Goguel A, Baudouin C. Flow cytometric analysis of inflammatory markers in conjunctival epithelial cells of patients with dry eyes. Invest Ophthalmol Vis Sci 2000; 41: 1356-1363.
2. Gao J, Schwalb TA, Addeo JV, Ghosn CR, Stern ME. The role of apoptosis in the pathogenesis of canine keratoconjunctivitis sicca: the effect of topical Cyclosporin A therapy. Cornea 1998; 17: 654-663.
3. Pflugfelder SC, Beuerman RW, Stern ME. In: Dry Eye and Ocular Surface Disorders. New York: Marcel Dekker, Inc; 2004.
4. Rocha EM, Wickham LA, Huang Z, Toda I, Gao J, da Silveira LA, Sullivan DA. Presence and testosterone influence on the levels of anti- and pro-inflammatory cytokines in lacrimal tissues of a mouse model of Sjogren's syndrome. Adv Exp Med Biol 1998; 438: 485-491.
5. Stern ME, Beuerman RW, Fox RI, Gao J, Mircheff AK, Pflugfelder SC. The pathology of dry eye: the interaction between the ocular surface and lacrimal glands. Cornea 1998; 17: 584-589.
6. Sullivan DA, Edwards JA. Androgen stimulation of lacrimal gland function in mouse models of Sjogren's syndrome. J Steroid Biochem Mol Biol 1997; 60: 237-245.
7. Sullivan DA, Sullivan BD, Evans JE, Schirra F, Yamagami H, Liu M et al. Androgen deficiency, meibomian gland dysfunction, and evaporative dry eye. Ann N Y Acad Sci 2002; 966: 211-222.











 texto en
texto en 


