Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.98 no.2 Madrid feb. 2006
ORIGINAL PAPERS
Double-balloon enteroscopy: a descriptive study of 50 explorations
E. Pérez-Cuadrado, P. Más, H. Hallal, J. Shanabo, E. Muñoz, I. Ortega, A. López Martín, E. Torrella, A. López Higueras, A. Martín and F. Carballo
Unit of Small Bowel. Section of Digestive Diseases. Hospital General Universitario Morales Meseguer. Murcia, Spain
ABSTRACT
Aim: to evaluate the utility of double-balloon enteroscopy for small-bowel disease.
Design: a prospective study of 50 consecutive enteroscopies performed from December 2004 to July 2005 to analyze diagnoses and treatments.
Patients: 44 patients (33 had undergone a previous capsule endoscopy) with indications for obscure digestive hemorrhage, angiodysplasia, Peutz-Jeghers syndrome, ulcer, suspected Crohn's disease, tumors, and refractory celiac disease.
Results: we carried out enteroscopy studies in 44 patients by the oral route and, in 6 additional patients, by both the oral and anal routes. We reached the ileon with the oral route in all cases but one (jejunal stenosis), and in 4 cases out of 7 with the anal route, with an average duration of 73 minutes. We found angiodysplasia in 19 cases, as well as NSAID-related enteropathy, Crohn's disease, diverticulosis, and Waldenström's disease. We performed biopsies in 31% of cases with diagnoses of adenocarcinoma, lymphangiectasia secondary to tumor in celiac disease, and Whipple's disease. We treated 19 patients with angiodysplasia (1 to 20 synchronous lesions) with argon, and 4 patients with polyps using polipectomy (sporadic polyps or Peutz-Jeghers syndrome). A retained capsule in one patient with stenosis was removed.
Conclusions: double-balloon enteroscopy is a useful and effective technique in the diagnosis and treatment of small intestine diseases, thus complementing capsule endoscopy. More studies are needed to analyze its impact on the management of this condition.
Key words: Double-balloon enteroscopy. Occult gastrointestinal bleeding. Angiodysplasia.
Pérez-Cuadrado E, Más P, Hallal H, Shanabo J, Muñoz E, Ortega I, López Martín A, Torrella E, López Higueras A, Martín A, Carballo F. Double-balloon enteroscopy: a descriptive study of 50 explorations. Rev Esp Enferm Dig 2006; 98: 73-81.
Introduction
The small intestine is nowadays fully accessible with capsule endoscopy (1), a first-line, non-invasive diagnostic procedure that works better than small-bowel follow-through (2). This "wireless" device has opened an oral approach to the small intestine, with an explosion of knowledge about endoscopic lesions (3). Despite the high diagnostic effectiveness of capsule endoscopy (around 75%) (4), we need a pathological and/or therapeutic classification in most cases. Oral push enteroscopy (OPE) was a step forward in both ways (5), but it could not examine the whole small intestine despite the help of the overtube, which increased range with no significant increase in diagnosis yield. If capsule endoscopy reveals a lesion out of OPE's reach, this lesion may only be accessible by surgery and/or intraoperative enteroscopy (IOE), which is deemed the "gold standard" for small intestine. However, an effectiveness lower than expected has been shown in IOE in case of obscure gastrointestinal hemorrhage (OGH), with relapses in 40% of patients (6). Recently, Yamamoto et al. (7) have developed a fine enteroscope that can be fitted into an special, flexible overtube with a balloon with monitored pressure at its distal end. This double-balloon enteroscopy (DBE), by means of a smart push-pull mechanism, makes the SI fold like a telescope, so that it can be fully examined with an adequate channel for biopsy and therapy measures, thus being better than OPE.
There are no publications so far about DBE in our country.
Methods
Material
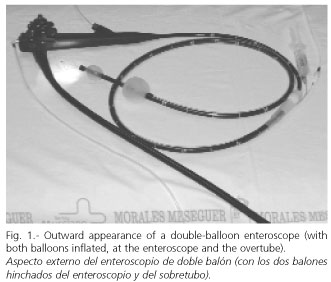
A videoenteroscope (EN-450. Fujinon. Japan) 2000 mm long with a 2.2 mm biopsy channel, and a flexible overtube (TS-12140 Fujinon. Japan) 1500 mm long with an inner wash channel (Fig. 1).
Both devices have balloons fitted in their distal end that are filled with air and connected by catheters to a manometer (PB-10. Fujinon. Japan) for pressure monitoring, which has an acoustic-visual security system in case of overpressure. A video processor with a magnification of 2:1 (EVE 400. Fujinon. Japan). Disposable ancillary material with a caliber lower than 2.2 mm and specifications similar to those of conventional endoscopy (biopsy forceps, polypectomy snares, injection needles, Dormia baskets). It is connected to an argon and coagulation unit (APC 300/ICC 200. Erbe. Germany).
Inclusion protocol
1. OGH with a diagnosis -by means of capsule endoscopy- of angiodysplasia, active bleeding, ulcer, polyp (sporadic or Peutz Jeghers) or tumor of the small intestine.
2. OGH with no etiological filiation after capsule endoscopy.
3. Celiac disease with a poor outcome and no significant findings during capsule endoscopy.
4. A procedure previous to DBE.
All patients signed an agreement and were informed about the technique and anesthesia. Preanesthetic examination: nothing to eat or drink for 12 hours. In case of rectal insertion, preparation with an oral cleansing solution (Fosfosoda®). Where appropriate, the patient was hemodynamically stabilized.
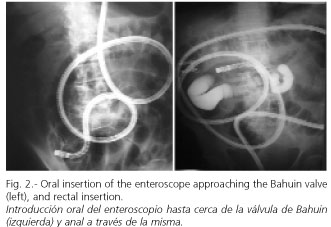
5. DBE technique: oral insertion with a mouth gag and/or rectal insertion (Fig. 2) in left lateral decubitus under deep sedation, moving forward the overtube and endoscope with alternative push-pull movements, with the help of the sequential inflation and deflation of their respective balloons, making the small intestine fold outside the overtube and endoscope.
-Oral DBE: theendoscope and overtube were inserted with deflated balloons approaching the jejunum, sucking the gastric cavity until they could not push forward. After the inflation of the overtube balloon, the insertion of the endoscope was carried out, and when it could not move forward, the inflation of the endoscope balloon and the deflation of the overtube balloon inserting the overtube later were carried out. These movements were alternatively repeated until no more could be inserted, and then both balloons were inflated (endoscope and overtube balloons) and then removed "en bloc" until they became resistant to pull or manometric overpressure. After this simultaneous pull, they stayed in the same place of the small intestine, so handles were rectified; after this, previous movements were repeated (8). After examining the small intestine, the endoscope and overtube balloons stayed half-inflated in order to avoid an abrupt movement of the enteroscope during withdrawal.
-Rectal DBE: the endoscope and overtube were inserted with deflated balloons through the colon in a way similar to that orally used until the Bahuin valve was reached, making the way through easier in prone decubitus. The small intestine was examined using movements similar to those carried out during oral insertion.
6. Lesion topography in small intestine: the jejunum was considered to be the two proximal fifths of the small intestine from the ligament of Treitz to the Bahuin valve, and the ileum the three distal fifths. Jejunum and ileum were divided into proximal, middle and distal in three equal parts. Radiological control and the instillation of a water-soluble contrast were occasionally carried out (Fig. 2).
7. Diagnostic procedures:
-Biopsy: it was carried out with forceps in order to obtain tissue samples for histological evaluation, polymerase chain reaction, electronic microscopy, etc.
-Indian-ink staining: in case of finding SI lesions subject to surgery or bleeding relapse after DBE therapeutics. Besides, after oral insertion, the most distal area was examined aiming at finding it in case of later instructions of rectal insertion, so that a complete examination of the SI was guaranteed.
-Chromoendoscopy: magnification (2:1). It was used to allow a better examination of the villous standard en cases of patchy atrophy, in an easy way using water or indigo carmine dye as instilled through a catheter.
8. Therapeutic procedures:
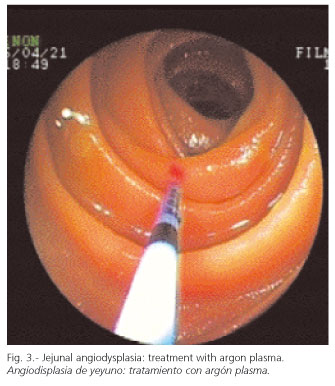
-Disposable argon catheters were used in cases of angiodysplasia, with a maximum flow of 0.5 L/m, 40 W, and tangential impact on the lesion (Fig. 3).
-Polyps were removed by means of diathermy snares, and foreign bodies were removed using a Dormia basket.
9. Statistical study: In the descriptive study, quantitative variables have been expressed as average plus/less standard deviation (a ± SD) values, and qualitative variables as total percentage. The statistical program used was SPSS, version 9.0.1, by SPSS Inc.
Results
Sample characteristics
From December 2004 to July 2005, 44 patients, 23 men and 21 women with an average age of 57.7 ± 19 years, were consecutively included, and a total of 50 examinations using DBE were performed. Six patients underwent DBE both rectally and orally.
The indication for DBE was OGH in 32 cases, with a previous diagnosis by capsule endoscopy in 18 and without it in 14 cases -suspicion of Crohn's disease (n: 4), Peutz Jegher's syndrome (n: 3), tumor (n: 3), and refractory celiac disease (one case); 33 patients (75%) had a previous capsule endoscopy performed. CE diagnoses included: in 22 patients (50%) angiodysplasia, 3 suspected cases of Crohn's disease, two stenosis, two polyps, and two ulcers. Oral insertion (n: 44) always led to reach the distal-middle ileum (one case close to Bahuin) except for one tumor and one jejunal stenosis. The rectum was reached in one case of complementary insertion by jejunostomy. Rectal insertion (n: 6) reached the proximal ileum (the middle part in 3 cases, and the distal part in one case). The way through the Bahuin valve was found difficult in one case, and in another case the examination was given up in the sigmoid colon after having some complications. Mean duration for the oral and rectal DBE was 73.2 ± 25.7 (25-165) and 73.1 ± 27.0 (10-100) minutes, respectively.
Diagnostic-therapeutic DBE
-Angiodysplasia. In the 19 patients suffering from angiodysplasia an average of 5.05 ± 5.61 (1-20) lesions were found, which were all treated using argon with no complications. The most complex vascular lesions were tattoos (Fig. 4).
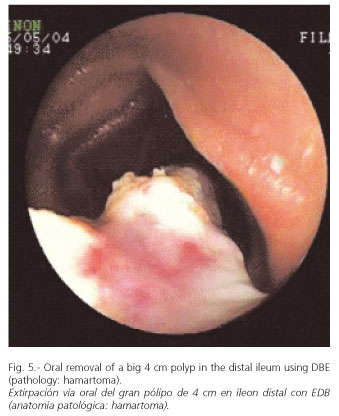
-Peutz Jeghers. In two patients who underwent previous laparotomies for small intestine obstruction (1 to 6 surgical resections) DBE confirmed the findings of capsule endoscopy, and big ileal polyps of 3.5 and 2 cm in size were removed (Fig. 5). In another case, capsule endoscopy detected 6 polyps, while with DBE 15 polyps bigger than 1 cm were found and removed with no complications (hamartomas).
-Jejunal diverticula. In two patients jejunal diverticula were found, which had remained unnoticed to capsule endoscopy.
-Polyps. One patient diagnosed as having an ulcer by capsule endoscopy had actually an ulcered polyp, which was removed.
-Diffuse lymphangiectasia. One patient suffering from refractory celiac disease developed a secondary diffuse lymphangiectasia close to one celiac tumor (adenocarcinoma) detected by capsule endoscopy.
-Whipple's disease. In one case of segmentary spontaneous bleeding during capsule endoscopy in several sections, DBE ruled out associated conditions and allowed to obtain histological material for polymerase chain reaction and EM (Fig. 6), which confirmed the disease.
-Ulcers. One case with Waldenström's disease and OGH had multiple ulcers. Two cases of ulcers caused by NSAIDs were also found.
-Tumors. Biopsies by DBE of a neoplastic-looking jejunal stenosis known to capsule endoscopy found an adenocarcinoma. DBE allowed to successfully removing the capsule held in said stenosis.
-Others. Biopsies in two patients were carried out with stenosis due to Crohn's disease with contraindicated capsule endoscopy, excluding a malignancy. Malignancy was also excluded in two cases of celiac disease, and other findings of lower clinical significance such as enteritis, isolated lymphangiectasia, xanthoma, micropolyps, etc., were documented. Biopsies were performed in a total of 14 patients (31.8%).
Complications
1. Technical complications: a balloon came out the enteroscope into the intestinal lumen, and was then removed using the Dormia basket.
2. Anesthetic complications: in one patient with endotracheal intubation, abdominal relaxation pushed the cannula, causing a selective intubation of the right main bronchus with desaturation.
3. Endoscopic complications: one patient with OGH and rectal insertion was found to have a marked perforation at 20 cm from the rectum due to serum adhesions around the torsion of a necrotic epiploic appendix that had not been previously diagnosed. The immediate operation showed an extraluminal lesion in that loop. As the preparation of the colon for DBE was good, a simple suture was carried out and the patient was discharged after 3 days.
Discussion
The small intestine is nowadays fully accessible for a pathological and/or therapeutic diagnosis using DBE, either orally or rectally, if necessary. This technique has been shown to be better than OPE in terms of length of small intestine explored (8).
One of the contraindications of capsule endoscopy is the known stenosis of the small intestine, but in cases where this is not suspected, capsules may be held within. DBE allows the pathological classification of stenosis and capsule removal, as was the case in one of our patients, the first one with OGH, who had a jejunal adenocarcinoma.
Capsule endoscopy and DBE have been shown in our study to be complementary techniques; the fairly harmlessness and non-invasivity of capsule endoscopy rendered it a first-line study for diagnosis, and DBE was carried out in cases requiring a histological diagnosis or endoscopic therapy. Capsule endoscopy can lead the way (orally or rectally) for DBE.
In OGH, capsule endoscopy has previously shown a high diagnostic effectiveness related to the early carrying out of the technique in connection with the time of the bleeding episode (4). In cases with no clear diagnosis by capsule endoscopy (as when visualizing bleeding in the small intestine with no detectable pathology), DBE has the advantage of allowing the washing and aspirating of blood remnants, which makes diagnosis and treatment easy.
As for angiodysplasia, the most frequently found lesion in our study, the number of lesions found by DBE has always been the same or higher than the one found by capsule endoscopy in all cases, which is obviously due to the insufflations, mobility, possibility of mucus washing, and higher number of pictures taken per second of DBE, with the disadvantage of causing alterations because of instrumental friction, which requires assessment and treatment at insertion (not at removal). The usefulness of DBE would be a reduction of transfusion requirements by treating as many lesions as possible, which would directly affect OPE (9). Another difficulty of these "evanescent" lesions is that they tend to be multiple (some synchronic lesions may go unnoticed) and may also develop metachronically; therefore, follow-up using capsule endoscopy seems an obvious option, and should new findings arrive then DBE would be carried out again.
On the other hand, some hereditary diseases such as Peutz Jeghers syndrome require a mapping by capsule endoscopy, which has been proved to be better than barium examinations in a study by Bordas et al. (10) where capsule endoscopy showed the number, size and location of polyps. After capsule endoscopy, a therapeutic DBE can be carried out, and following the resection of polyps capsule endoscopy (less invasive) can be used to control metachronic lesions before they become serious by blocking the lumen and folding the affected loop, which is important in patients with several previous laparotomies. That way, DBE has allowed in our study the removal of big-sized and multiple polyps, in one case with 6 previous laparotomies (Fig. 5), and the removal of 15 polyps in the same lesion in another patient.
Inflammatory intestinal disease has several difficulty levels in the small intestine. Crohn's disease can only affect the small intestine or even only the jejunum, and OPE has limited usefulness (11). On the other hand, indeterminate colitis where lesions in the small intestine are found by capsule endoscopy requires a DBE with biopsy collection for its diagnosis.
It seems only obvious that IOE requiring laparotomy and IOE having a limited examination area of the small intestine will give way to this new technique, as DBE has been shown in our study to be an easy, safe, and effective technique for the treatment of bleeding lesions, and for the performance of biopsies in areas not accessible to other techniques; it has been seen to even offer a new macroscopic diagnosis after capsule endoscopy. We think that DBE is a basic tool in many cases after a first-line non-invasive study of the small intestine with capsule endoscopy, and this endoscopic technique can be designated the diagnostic and therapeutic "gold standard" in the small intestine.
References
1. Iddan G, Meron G, Glukhovsky A, Swain P. Wireless capsule endoscopy. Nature 2000; 405 (6785): 417. [ Links ]
2. Costamagna G, Shah SK, Riccioni ME, Foschia F, Mutignani M, Perri V, et al. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology 2002; 123 (4): 999-1005. [ Links ]
3. Pérez-Cuadrado E. Acceso oral al intestino delgado. Rev Esp Enferm Dig 2002; 94 (7): 423-6. [ Links ]
4. Pennazio M. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: report of 100 consecutive cases. Gastroenterology 2004, 126: 643-53. [ Links ]
5. Pérez-Cuadrado E. Videoenteroscopia oral: estudio prospectivo de 30 casos. Rev Esp Enferm Dig 1996; 88: 9-15. [ Links ]
6. Ress AM, Benacci JC, Sarr MG. Efficacy of intraoperative enteroscopy in diagnosis and prevention of recurrent, occult gastrointestinal bleeding. Am J Surg 1992; 163: 94-8. [ Links ]
7. Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc 2001; 53: 216-20. [ Links ]
8. May A, Nachbar L, Shneider M, Neuman M, Ell C. Push-and-pull enteroscopy using the double-balloon technique: method os assessing depth os insertion and training of the enteroscopy technique using the erlangen endo-trainer. Endoscopy 2005; 37 (1): 66-70. [ Links ]
9. Pérez-Cuadrado E, Molina E, Lamas D. Diagnostic and therapeutic efficacy in a push enteroscopy series. Endoscopy 2000; 32 (Supl. 1) (E 58). [ Links ]
10. Mata A, Llach J, Castells A, Rovira JM, Pellise M, Gines A, et al. A prospective trial comparing wireless capsule endoscopy and barium contrast series for small-bowel surveillance in hereditary GI polyposis syndromes. Gastrointest Endosc 2005; 61: 721-5. [ Links ]
11. Pérez-Cuadrado E, Macenlle R, Iglesias J. Usefulness of oral video push enteroscopy in Crohn's disease. Endoscopy 1997; 29: 745-7. [ Links ]
![]() Correspondencia:
Correspondencia:
Enrique Pérez-Cuadrado.
C/ Delfos, 19.
30007 Murcia.
e-mail: eperezcuadradom@meditex.es
Recibido: 04-03-05.
Aceptado: 08-08-05.











 texto en
texto en