Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.98 no.3 Madrid mar. 2006
PICTURES IN DIGESTIVE PATHOLOGY
Hemobilia
D. Vañó, J. García-Cano1, C. J. Gómez-Ruiz1 and G. Arranz
Department of Internal Medicine. 1Department of Gastroenterology. Hospital Virgen de la Luz. Cuenca, Spain
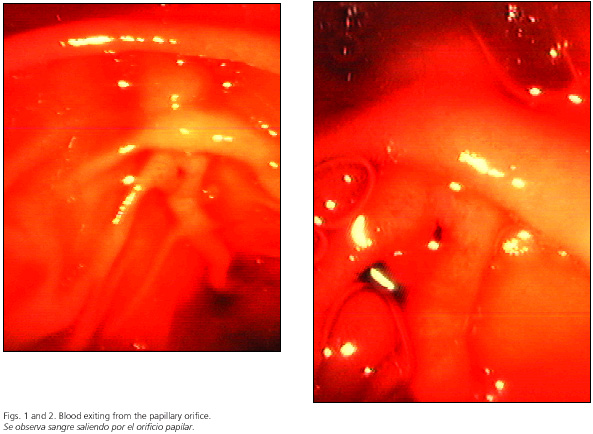
A 74-year-old woman was admitted because of dark stools in the last four days. She suffered from atrial fibrillation, had two heart valves implanted (mitral and aortic), and was under anticoagulant therapy with acenocumarol. The most remarkable laboratory findings were hemoglobin 9.2 g/dl, hematocrit 26.8%, mean corpuscular volume 94.2 fl, and blood urea 80 mg/dl. Prothrombin time was 28% and INR 2.65. An esophago-gastro-duodenoscopy was performed. Blood was observed in the second duodenal portion, perhaps in the papillary area, although no definite source was found. The routine forward-view gastroscope was exchanged for a side-view duodenoscope. Blood was seen oozing out the papilla (Figs. 1 and 2). Conservative measures were taken using blood transfusions and venous fluid supply. Magnetic resonance cholangiopancreatography and abdominal magnetic resonance angiography revealed only cholecystolithiasis and no vascular abnormalities. The patient did well without rebleeding, and she was discharged.
Hemorrhage through the papilla of Vater may have three sources: the bile-duct system (hemobilia), the pancreatic duct (hemosuccus or wirsungorrhage) (1), and the papilla itself (for instance, in ampullary tumors). Diagnosis is difficult because routine forward-view gastroscopes cannot properly see the papilla. If a papillary source is suspected endoscopy should be performed with duodenoscopes as used for ERCP. If vascular interventional radiology is available a celiac axis angiography should be performed, which can be both diagnostic and therapeutic. In contrast, as in the case reported here, a magnetic resonance angiography allows to rule out vascular abnormalities, and a wait-and-see policy can be undertaken. Hemobilia has been reported to occur in patients having gallbladder pathology (2) and on anticoagulant therapy (3). Our patient had both risk factors.
References
1. García-Cano Lizcano J, Morillas Ariño J, Navarro S, Pérez Vigara G, Parera A, Pérez Sola A. Wirsungorrhage. 21st meeting of the Spanish Society of Gastrointestinal Endoscopy. Barcelona, November 1999.
2. De Quinta Frutos R, Moles Morenilla L, Docobo Durantez F, Soto Pradas JA, Iriarte Calvo J, Vázquez Medina A. Hemobilia secondary to chronic cholecystitis. Rev Esp Enferm Dig 2004; 96: 221-5.
3. Hong JW, Han YS, Lee JH, Kim NH, Lim KW, Joung YH, et al. A case of non-traumatic hemobilia due to warfarin therapy [in Korean, abstract in English]. Korean J Gastroenterol 2004; 44: 292-5.











 texto en
texto en