Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 no.6 Madrid jun. 2014
LETTERS TO THE EDITOR
Pancreaticopleural fistula: An unusual cause of persistent pleural effusion
Fístula pancreaticopleural: una causa poco frecuente de derrame pleural masivo recidivante
Key words: Pancreaticopleural fistula. Pleuropancreatic fistula. Pleural efusion. Chronic pancreatitis.
Palabras clave: Fístula pleuropancreática. Fístula pancreaticopleural. Derrame pleural. Pancreatitis crónica.
Dear Editor,
There are multiple causes of persistent pleural effusion. Pancreaticopleural fistula (PFF) is one of them. This is a rare entity that only occurs occasionally in differential diagnoses due to the fact that it is an extremely rare consequence of chronic pancreatitis in adults. We report the case of persistent pleural effusion resulting from a pancreaticopleural fistula in a patient with chronic pancreatitis.
Case report
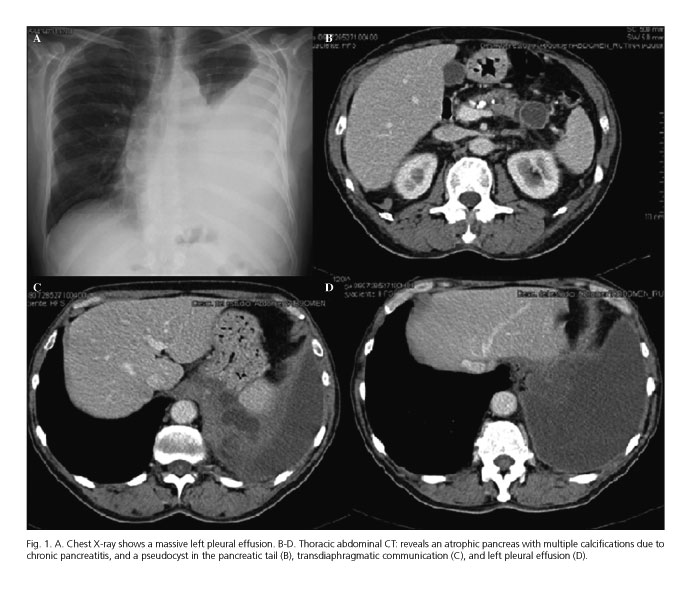
We present a 63-year-old male patient complaining of progressive dyspnoea, cough and fever with a history of smoking, alcoholism and chronic pancreatitis. A chest X-ray performed in the Emergency Department (Fig. 1), revealed a massive left pleural effusion. A thoracocentesis was performed, showing a negative culture result for pathogens, with 60 % polymorphonuclear exudate in which 12,400 IU/L of amylase in pleural fluid stood out. A thoracic CT was performed, revealing infiltrate in the LLL and small ground glass alterations. Suspicion of a parapneumonic effusion led to medical treatment. However, the effusion worsened, and a new diagnostic and evacuative thoracocentesis was performed, with negative cytology for malignant cells, negative culture, a pleural biopsy with no evidence of tumour, and with high amylase levels standing out again at 10,156 IU/L. Given the persistent pleural effusion, a thoracic-abdominal CT was performed (Fig. 1) revealing a 28 mm pancreatic pseudocyst communicating with a liquid collection of 2 x 5.5 x 7 cm extending from the pancreas to the subphrenic space, and associated with the massive left pleural effusion. These findings indicated the presence of pancreaticopleural fistula.
A medical treatment was initiated which consisted of fasting, total parenteral nutrition, chest drainage with a tube and octreotide, administered by subcutaneous injection of 100 µg every 8 hours, doubling the dose in the event of high drainage flow. An ERCP was performed aimed at stenting the main pancreatic duct, which was not technically possible due to the fact that the fistula was located in the pancreatic pseudocyst, in turn located in the pancreatic tail. Despite the initial medical treatment, the patient showed no improvement, so he was finally surgically intervened two months after the treatment was initiated. The intervention revealed a 2 cm diaphragmatic orifice exposing the pseudocyst to the pleural cavity and constituting the pancreaticopleural fistula. A distal pancreatectomy was performed as well as closure of the left diaphragmatic orifice. Due to the massive pancreatic inflammation, a splenectomy could not be avoided. These procedures were followed by a left pleural drainage with derivation of the transmesocolic-retrocolic roux-en-Y distal termino-lateral Wirsung duct after extraction of calculi. The patient showed satisfactory progress, the pleural drain being removed on the third post-operative day with no recurrence of effusion, and the patient being discharged on the sixth. The patient remains asymptomatic two years following the intervention.
Discussion
The pancreaticopleural fistula is a rare entity, inducing predominantly thoracic symptoms. Initial treatment should be medical with chest drainage, inhibition of pancreatic secretions, and application of a pancreatic stent -although there are studies supporting early surgical intervention since this reduces recovery time and has a higher success rate.
Montiel Jiménez-Fuertes1, Manuel Durán-Poveda2 and Damián García-Olmo3
1Hepatobiliopancreatic Surgery Unit. Department of General and Digestive Surgery.
2Department of General and Digestive Surgery. Hospital Rey Juan Carlos. Móstoles, Madrid. Sapin.
3Department of General and Digestive Surgery. Fundación Jiménez-Díaz. Madrid, Spain
References
1. Zubiaurre L, Oyarzabal I, Beguiristain A, Amato E, Zapata E, Salvador P. Fístula pancreatopleural: pruebas diagnósticas y tratamiento. Cir Esp 2005;77:359-61. [ Links ]
2. Sut M, Gray R, Ramachandran M, Diamond T. Pancreaticopleural fistula: A rare complication of ERCP-induced pancreatitis. Ulster Medical Journal 2009;78:185-6. [ Links ]
3. Safadi BY, Marks JM. Pancreatic-pleural fistula: the role of ERCP in diagnosis and treatment. Gastrointestinal Endoscopy 2000;51:213-5. [ Links ]
4. Roberts KJ, Sheridan M, Morris-Stiff G, Smith AM. Pancreaticopleural fistula: Etiology, treatment and long-term follow-up. Hepatobiliary Pancreat Dis Int 2012;11:215-9. [ Links ]
5. King JC, Reber HA, Shiraga S, Hines OJ. Pancreatic-pleural fistula is best managed by early operative intervention. Surgery 2010; 147:154-9. [ Links ]
6. Wronski M, Slodkowski M, Cebulski W, Moronczyk D, Krasnodebski IW. Optimizing management of pancreaticopleural fistulas. World J Gastroenterol 2011;17:4696-703. [ Links ]
7. Khan AZ, Ching R, Morris-Stiff G, England R, Sherridan MB, Smith AM. Pleuropancreatic fistulae: Specialist center management. J Gastrointest Surg 2009;13:354-8. [ Links ]
8. Dhebri AR, Ferran N. Nonsurgical management of pancreaticopleural fistula. Journal of the Pancreas 2005;6:152-61. [ Links ]
9. Rockey DC, Cello JP. Pancreaticopleural fistula: Report of 7 patients and review of the literature. Medicine 1990;69:332-44. [ Links ]
10. Iribarren Díaz M, Castro Parga G, Díaz Cardamas P, Freiria Barreiro G, Pérez Domínguez L, Rivo Vazquez A, et al. Comunicación pancreático-pleural secundaria a pseudoquiste pancreático. Uma complicación de evolución variable. Rev Esp Enferm Dig 2008;100:730-1. [ Links ]











 texto en
texto en