Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 no.3 Madrid mar. 2017
https://dx.doi.org/10.17235/reed.2016.4269/2016
CASE REPORT
Mucormycosis: an unusual cause of gastric perforation and severe bleeding in immunocompetent patients
Patricia Sánchez-Velázquez1, Manuel Pera1, Javier Gimeno2, Ana Zapatero3, Juan Nolla3 and Miguel Pera1
Departments of 1Surgery, 2Pathology and 3Intensive Care Unit. Hospital del Mar-Medical Research Institute (IMIM). Barcelona, Spain
ABSTRACT
Mucormycosis is a rare and often fatal opportunistic infection that especially occurs in immunocompromised patients. Primary gastrointestinal infection is uncommon and accounts for only approximately 7% of all cases of mucormycosis but it is associated with an 85% mortality rate due to perforation and massive bleeding. Very few cases of gastrointestinal mucormycosis in an immunocompetent host have been reported. We describe a case of gastric necrosis and massive bleeding due to fulminant invasive mucormycosis.
Key words: Gastric. Mucormycosis. GI bleeding.
Introduction
Mucormycosis is a rare and often fatal opportunistic infection that especially occurs in immunocompromised patients (1,2). The most frequent forms of presentation are rhinocerebral, pulmonary, cutaneous or disseminated. Primary gastrointestinal infection is uncommon and accounts for only approximately 7% of all cases of mucormycosis, but it is associated with an 85% mortality rate due to perforation and massive bleeding (3-5). Very few cases of gastrointestinal mucormycosis in an immunocompetent host have been reported (6-8). We describe a case of gastric necrosis and massive bleeding due to fulminant invasive mucormycosis.
Case report
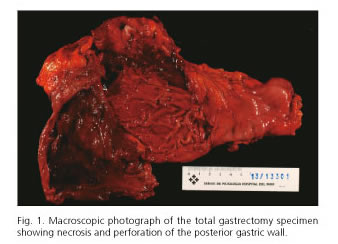
A 53-year-old female was referred to our Intensive Care Unit (ICU) with the diagnosis of intracraneal hemorrhage caused by rupture of an aneurysm from the right posterior communicant artery that underwent embolization. The patient was sedated and required mechanical ventilation and dexamethasone 4 mg intravenously every 6 hours. Her medical history was remarkable for hypertension, asthma, and conservative surgery for breast cancer two years before. Neurological recovery was complicated with aspiration pneumonia treated with antibiotics. On the 12th day of stay in the ICU, the patient suddenly presented a massive hematemesis and hypovolemic shock. After hemodynamic stabilization, an upper endoscopy was performed which showed a large circumferential ulcer extending from the esophagogastric junction to the upper stomach, which was full of blood clots. Consequently, emergency laparotomy was performed that revealed about 2 liters of hemoperitoneum, extensive necrosis and perforation of the posterior wall of the stomach. Total gastrectomy was performed (Fig. 1). During the procedure the patient presented signs of coagulopathy so we decided not to perform anastomosis, and control of bleeding with packing. Perioperative blood products requirements were 8 packed red blood cells units and 2 liters of fresh frozen plasma. Despite intensive resuscitation, the patient developed multiple organ failure and died 8 hours later. An autopsy was requested but it was refused by the family.
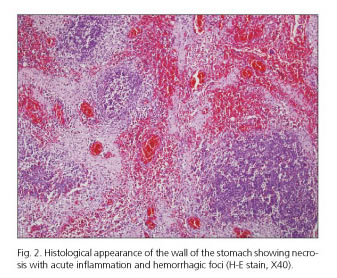
Histologic examination revealed extensive areas of gastric transmural coagulative necrosis associated with mild inflammation (Fig. 2) and the presence of structures consistent with hyphae, some of them inside blood vessels, and causing vascular thrombosis. Periodic acid Schiff (PAS) and Grocott staining were performed to better characterize the morphology of the hyphae, and revealed several broad non-septate fungal hyphae with irregular right angle branching, with a measure between 10 and 20 µm in width. The fungal organisms were morphologically consistent with gastric mucormycosis (Fig. 3 A and B).
Discussion
Mucormycosis is a life-threatening opportunistic invasive infection caused by fungal agents within the order Mucorales (1). The fungi live in the soil and they are also present in the air and food (2). The most commonly isolated family is Mucoraceae, which includes Rhizopus, Rhizomucor, Actinomucor, and Mucor, among other species (1). Members of this family usually cause an acute and invasive infection in patients with cancer, bone marrow and solid organ transplant recipients, as well as in patients with inherited immunodeficiencies (2,3,5,9). However, unlike other filamentous fungi, mucormycosis can also be a frequently lethal infection in hosts with greater immunocompetency, such as those with diabetes mellitus, cirrhosis, malnutrition or chronic renal failure (2,4,9,10). Very few cases of gastrointestinal mucormycosis have been reported in presumably immunocompetent patients admitted to the ICU for trauma or pneumonia (6-8).
Blood vessels invasion by hyphae leads to arterial thrombosis, tissue infarction, hemorrhage and necrosis (6). When mucormycosis involves the gastrointestinal tract, it is most frequently seen in the stomach (58%) or colon (32%) (2,4). The most common presenting symptom for invasive mucormycosis is upper gastrointestinal bleeding, which was consistent with this patient presentation. Gastric mucormycosis, from colonization to infiltrative disease, has been described complicating peptic ulcer disease and a other gastrointestinal conditions such as peritonitis, tuberculosis, and gastric carcinoma (3,7,9).
It remains unclear how the fungal pathogen was introduced into her gastrointestinal tract. Fungi of the mucorales order are ubiquitous in the environment and several predisposing factors such as gastric ulcer, the ingestion of contaminated food and the use of nasogastric intubation have been described as responsible for the development of gastric mucormycosis. In the present case an undiagnosed acute or chronic peptic ulcer might have facilitated fungal entry and the development of invasive mucormycosis. An outbreak of five cases of gastric mucormycosis in a single ICU associated with the use of contaminated wooden tongue depressors was recently reported (10). Although environmental cultures were not performed in our ICU, during the subsequent year no other case of mucor was identified in our center.
In conclusion, gastric mucormycosis is an exceedingly rare infection, particularly in immunocompetent individuals. In our case, it seems likely that fungal colonization occurred prior to her hospital admission, and infection developed after performing multiple invasive procedures. Early diagnosis and antifungal therapy along with gastric resection in selected cases are essential to improve prognosis.
References
1. Kontoyiannis DP, Lewis RE. Invasive zygomycosis: Update on pathogenesis, clinical manifestations, and management. Infect Dis Clin North Am 2006;20:581-607. DOI: 10.1016/j.idc.2006.06.003. [ Links ]
2. Roden M, Zaoutis T. Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis 2005;41:634-53. DOI: 10.1086/432579. [ Links ]
3. Kaiser P, Maggio EM, Pfammatter T, et al. Histopathological evidence of invasive gastric mucormycosis after transarterial chemoembolization and liver transplantation. Infection 2014;42:779-83. DOI: 10.1007/s15010-014-0603-7. [ Links ]
4. Corey KE, Gupta NK, Agarwal S, et al. Case records of the Massachusetts General Hospital. Case 32-2013. A 55-year-old woman with autoimmune hepatitis, cirrhosis, anorexia, and abdominal pain. N Engl J Med 2013;369:1545-53. DOI: 10.1056/NEJMcpc1208153. [ Links ]
5. Irtan S, Lamerain M, Lesage F, et al. Mucormycosis as a rare cause of severe gastrointestinal bleeding after multivisceral transplantation. Transpl Infect Dis 2013;15:E236-8. DOI: 10.1111/tid.12147. [ Links ]
6. Choi HL, Shin YM, Lee KM, et al. Bowel infarction due to intestinal mucormycosis in an immunocompetent patient. J Korean Surg Soc 2012;83:325-9. DOI: 10.4174/jkss.2012.83.5.325. [ Links ]
7. Berne JD, Villarreal DH, McGovern TM, et al. A fatal case of post-traumatic gastric mucormycosis. J Trauma 2009;66:933-5. DOI: 10.1097/01.ta.0000233673.30138.0c. [ Links ]
8. Johnson CB, Ahmeti M, Tyroch AH, et al. Gastric mucormycosis as a cause of life-threatening upper gastrointestinal bleeding in a trauma patient. Am Surg 2010;76:E76-7. [ Links ]
9. Chhaya V, Gupta S, Arnaout A. Mucormycosis causing giant gastric ulcers. Endoscopy 2011;43:289-90. DOI: 10.1055/s-0030-1256425. [ Links ]
10. Maraví-Poma E, Rodríguez-Tudela JL, De Jalón JG, et al. Outbreak of gastric mucormycosis associated with the use of wooden tongue depressors in critically ill patients. Intensive Care Med 2004;30:724-8. DOI: 10.1007/s00134-003-2132-1. [ Links ]
![]() Correspondence:
Correspondence:
Patricia Sánchez-Velázquez.
Department of Surgery.
Hospital del Mar-Medical Research Institute (IMIM).
Passeig Marítim, 25-29.
08003 Barcelona, Spain
e-mail: 99976@parcdesalutmar.cat
Received: 15-02-2016
Accepted: 05-04-2016