Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.110 no.8 Madrid ago. 2018
https://dx.doi.org/10.17235/reed.2018.5255/2017
SPECIAL ARTICLE
Review of duodenal perforations after endoscopic retrograde cholangiopancreatography in Hospital Puerta de Hierro from 1999 to 2014
1Servicio de Cirugía General y Aparato Digestivo. Hospital Universitario Puerta de Hierro. Majadahonda, Madrid, Spain
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is the most suitable test to diagnose and treat bile duct pathology 1,2,3. In 1968, the endoscopic cannulation of the bile duct was performed for the first time by Mc Cune and Schorb. More than 40 years later, it is still the most adequate test for the diagnosis of most biliary pathologies as well as treatment. However, the procedure has significant associated complications that should be considered.
ERCP can result in a major complication rate of up to 10% 4,5,6 such as acute pancreatitis, hemorrhage and perforation with an associated mortality of 1%. The risk of perforation is around 1%, with an associated mortality rate of up to 18% in centers with extensive experience 7,8.
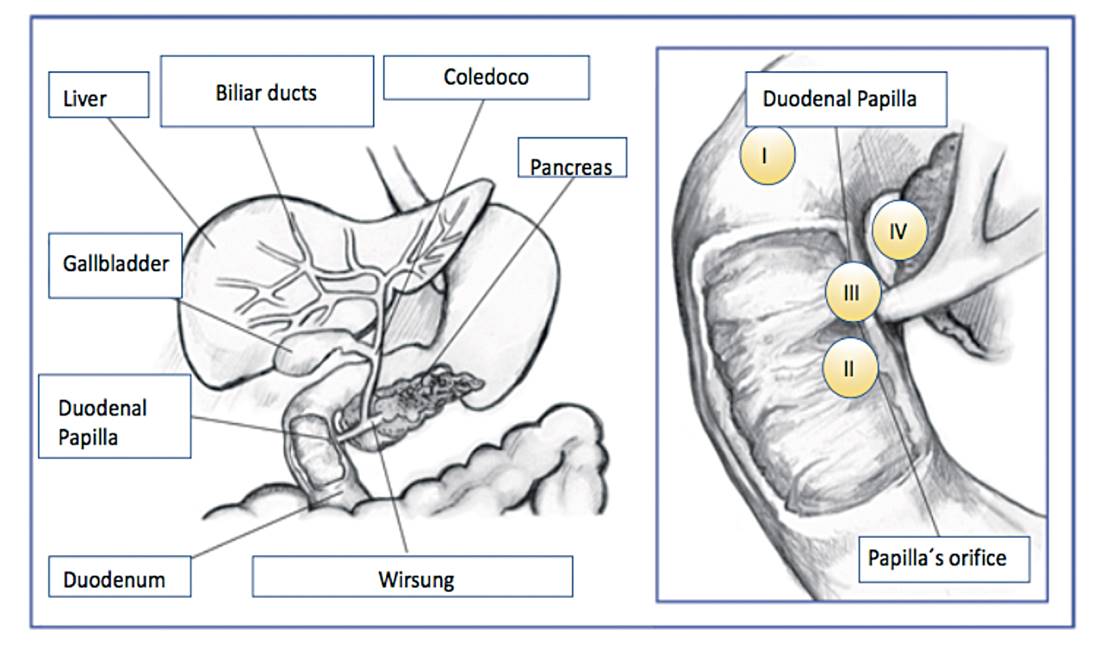
Since its description more than 15 years ago 9, the Stapfer classification is used to stage perforations associated with the procedure and to determine the adequate treatment. The classification consists of four types according to the place of injury and mechanism, with associated therapeutic and prognostic implications. Type I perforations are produced by the metal guide and are located on the medial or lateral aspect of the duodenum. Type II include periampullary perforations derived from a sphincterotomy. Type III occur far from the papilla and are related to the instrumentation. Type IV perforations are associated with the presence of retropneumoperitoneum post-ERCP and are not considered as true perforations (Fig. 1). The most frequent are type II followed by type III. The most serious and less frequent are type I 10.
Classically, post-ERCP perforations were an indication of surgical treatment, with more or less extensive resections. However, the approach has changed due to the greater knowledge of anatomy and surgical techniques and the development of non-invasive radiological techniques. Nowadays, some perforations can be managed conservatively with a good outcome 11.
The aim of this study was to review all post-ERCP perforations reported and managed by the Department of General and Digestive Surgery of Puerta de Hierro Clinic (Madrid) and Hospital Universitario Puerta de Hierro (Majadahonda) between 1999 and 2014. Our experience with regard to the treatment according to the type of perforation was evaluated.
MATERIAL AND METHODS
Between 1999 and 2014, 4,513 ERCP procedures were performed, with and without sphincterotomy, in Puerta de Hierro Clinic and Hospital Universitario Puerta de Hierro Majadahonda in Madrid. Thirty-six patients (0.79%) suffered duodenal perforations during the procedure. The mean age of the patients was 72.02 years; twenty-five were female (69%) and eleven were male (31%) (Table 1).
Table 1 General characteristics of patients undergoing ERCP
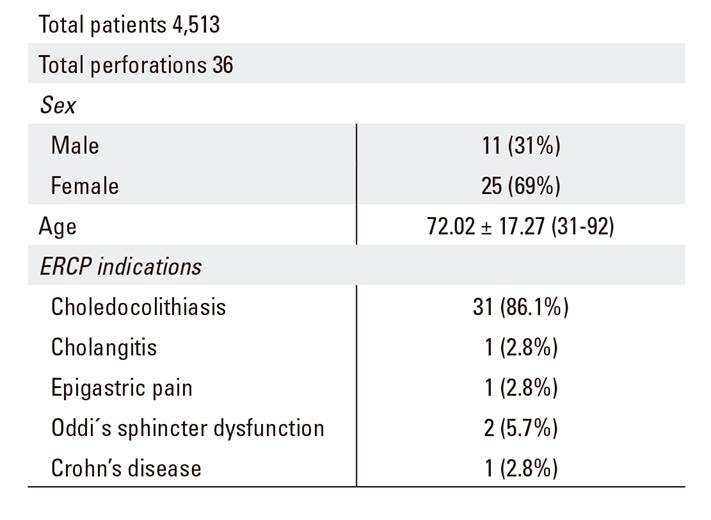
Data are expressed as the mean ± SD (range) or number (percentage).
The following data were retrospectively collected in thirty-six patients with documented duodenal perforations during or after ERCP: indication and findings of the ERCP, type of perforation (Stapfer), perforation symptoms, method of diagnosis, time to diagnosis (immediate [during the ERCP], < 24 hours or > 24 hours later), type of treatment (conservative or surgical), time to surgery, type of surgery performed, hospital stay and morbimortality.
RESULTS
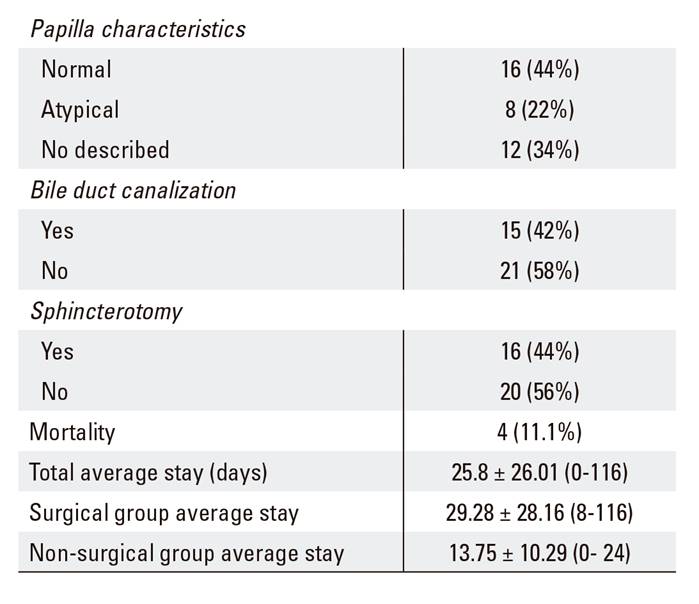
ERCP indications included residual choledocholithiasis before cholecystectomy in 31 patients (86.1%) and cholangitis with associated choledocholithiasis in 2.8% of cases. Other causes included epigastralgia in one case, two sphincter dysfunctions of Oddi and one case with Crohn's disease (Table 1). Table 2 shows the clinical aspects and findings related to the ERCP procedure.
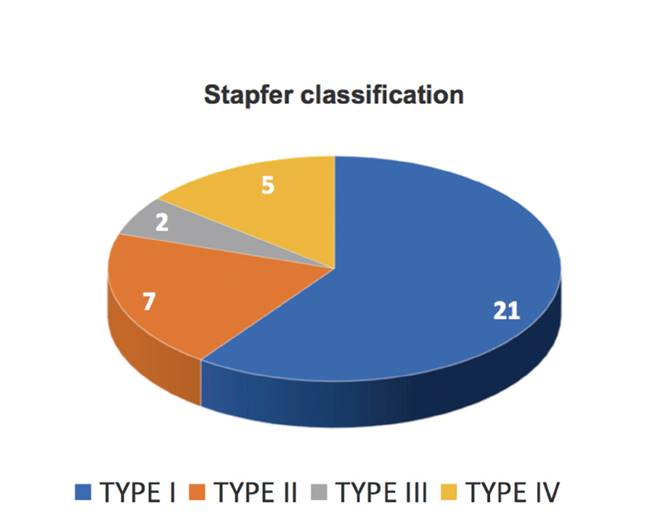
According to the Stapfer's classification, 21 patients had type I perforations (58.3%); eight, type II (22.2%); two, type III (5.6%); and five, type IV (13.9%) (Fig. 2).
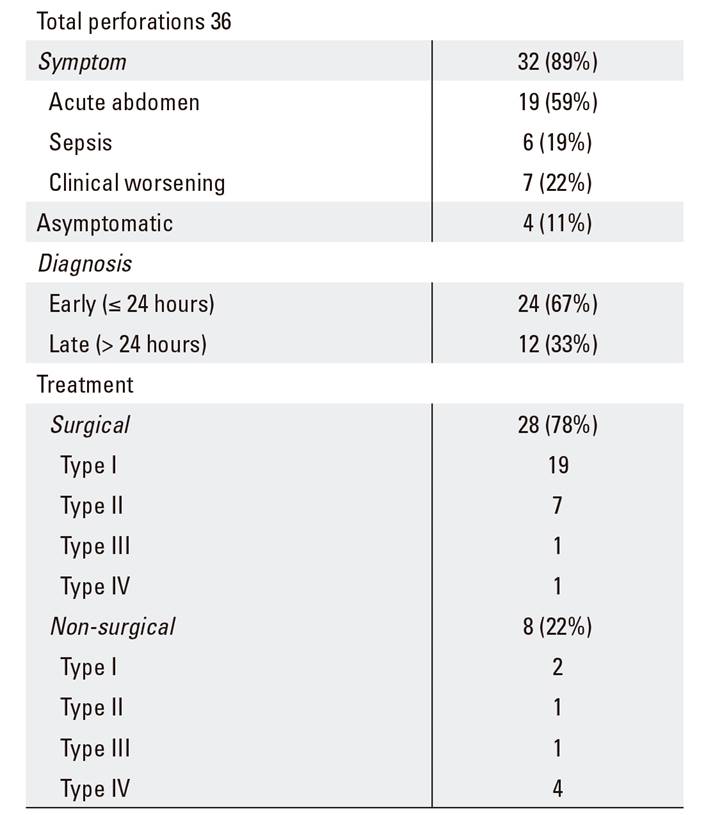
With regard to symptoms, 19 patients (52.8%) had an acute abdomen with moderate pain and a pathological examination. Six patients (16.7%) developed sepsis and seven patients (19.4%) experienced a deterioration from their baseline condition such as greater abdominal pain or a deterioration in the biochemical parameters. Four patients (11.1%) were asymptomatic (Table 3).
In 24 of the 36 cases (67%), the diagnosis was made or suspected during the first 24 hours after the ERCP; 12 patients (33%) were diagnosed a few days after the procedure. Diagnosis was performed via computerized tomography (CT) in the majority of patients (72%) (Table 3).
Twenty-eight patients were managed surgically (77.8%). Eight patients (22.2%) were treated medically due to the presence of the following parameters: Stapfer type IV (except for clinical or analytical deterioration) and Stapfer type II and III with a normal physical examination; the absence of sepsis, minimal leakage and the absence of collections of retroperitoneal fluid were demonstrated by computed tomography; two patients with a type I perforation but not candidates for surgical treatment due to comorbidities (Table 3).
Surgical treatment
Twenty-eight patients (77.8%) were treated surgically: 19 patients with type I perforations, seven with type II, one with type III and one with type IV. The time interval until surgery was less than 24 hours in 21 (75%) cases. The remaining seven patients (25%) underwent surgery after a clinical deterioration such as the development of septic peritonitis with large intra-abdominal or retroperitoneal collections.
A perforation suture, cholecystectomy with intraoperative cholangiography and drainage placement was performed in seven patients (25%). The second most frequent surgical procedure (14.3%) was the placement of a Kehr drainage. Other techniques included biliary tract derivation (hepaticojejunostomy in three patients or choledochoduodenostomy in three patients) or a gastrectomy (Table 4). The median hospital stay of surgically treated patients was 18.5 days.
Table 4 Surgical technique
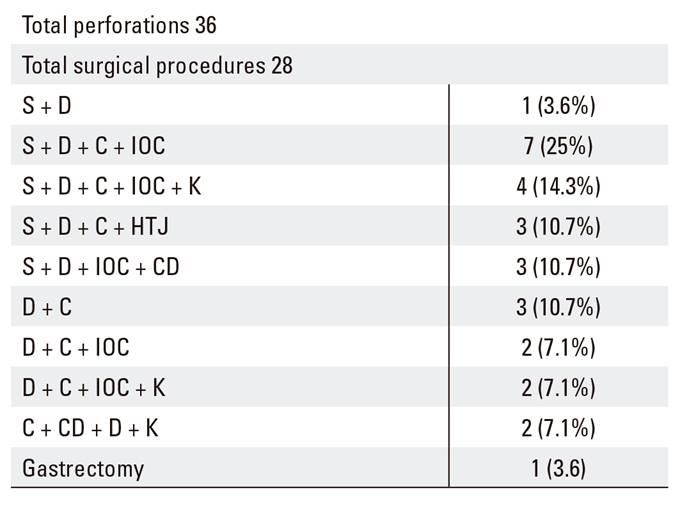
Data are expressed as the mean ± SD (range) or number (percentage). S: suture; D: drainage; C: cholecystectomy; IOC: intraoperative cholangiography; K: Kerh drainage; HTJ: hepaticojejunostomy; CD: choledocoduodenostomy.
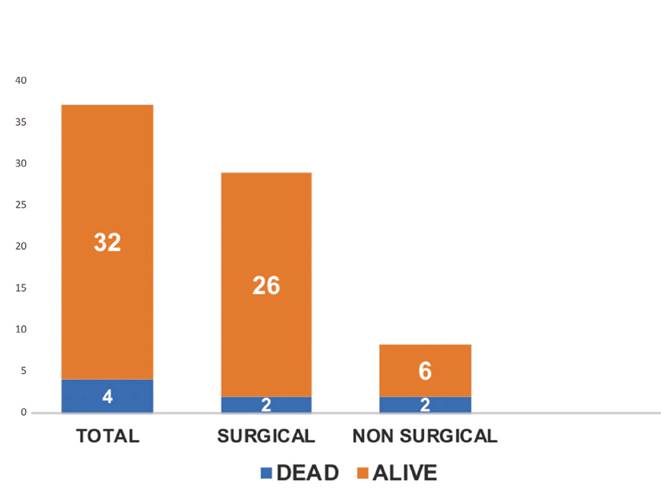
Eleven of the patients who underwent surgery had complications (39.3%). The most frequent complication was abdominal abscess or leakage, which occurred in eight patients (73%). All cases were managed conservatively with antibiotics and percutaneous drainage. Other complications included acute cholangitis after primary surgical treatment, gastrointestinal hemorrhage and medical complications such as atrial fibrillation or acute renal insufficiency. None of the 28 surgical patients required further surgery due to duodenal leakage. Only one patient required an additional surgery due to acute cholangitis that did not respond to medical treatment. A hepatic jejunostomy was performed in this case. There were two deaths in the surgically treated group, both cases with type I perforations and aged around 80 years, with a previous diagnosis of choledocholithiasis. One of them died due to a complication related to a digestive hemorrhage and the other, due to a previous comorbidity (Fig. 3).
Non-surgical treatment
Eight patients (22.2%) were treated conservatively: two patients with type I perforations, one with type II, one with type III and four with type IV.
Only patients with type IV perforations were candidates for conservative treatment, except for one young patient with moderate abdominal pain and altered complementary tests who finally underwent surgery. Cases with type II and III perforations with minimal abdominal pain, without sepsis or collections according to the imaging test, also underwent a conservative treatment. Furthermore, there were two cases with type I perforations who were not candidates for surgical treatment due to age and comorbidities and also received a conservative treatment. The median hospital stay of this group was 19.5 days. There was only one case of pulmonary thromboembolism as a complication. The two patients who were not surgically treated finally died due to a previous morbidity (Fig. 3).
DISCUSSION
Endoscopic retrograde cholangiopancreatography is still the technique of choice for both the diagnosis and treatment of a biliary pathology, especially choledocholithiasis and acute cholangitis. However, there is a 10% risk of major complications; acute pancreatitis is the most frequent 5, followed by hemorrhage and perforation (0.01- 2.1%) 7,12. The latest reported associated mortality is up to 18%.
Stapfer et al. 9 classified duodenal perforations according to their cause, size and location. Type I are caused by the endoscope and are located on the medial or lateral side, usually large and far from the blister. Type II are peri-ampullary lesions that occur after trying to canalize the papilla. Type III are usually small and are related to the cannulation of the bile duct with the guides. Those of type IV are not considered as real perforations and are due to the compression of the air used to maintain intraluminal visualization (Fig. 1).
Due to technical improvement within endoscopy units and the early diagnosis during the procedure, the handling of these complications has changed in the last decades from a surgical approach 13 to a more conservative treatment 2. Surgery is reserved for cases of a direct duodenal perforation by the endoscope (type I) or type II and III cases with poor prognosis data.
In this study, all perforations documented and treated within the Department of General and Digestive Surgery over the last 15 years have been reviewed. Their management has been classified according to the type of perforation (Stapfer classification) and the treatment.
A total of 36 perforations were reported in a total of 4,513 ERCP performed over the last 14 years. The global incidence was 0.79%, which is within the incidence range of other centers. The majority of cases were female (there was a higher incidence of lithiasis in this group) and the diagnosis was usually early and occurred during the procedure or within the first 24 hours. The diagnosis was confirmed via an urgent abdominal CT which identified extra-luminal gas or collections associated with the perforation in a few cases, with the exception of the cases diagnosed during the ERCP procedure, when no imaging test was required or other cases where it was not clinically possible. Computerized axial tomography is the radiological method of choice for an early diagnosis in most series 14.
Abdominal pain is the most common clinical manifestation of complications. This usually begins a few hours after the procedure and varies in intensity depending on the type of perforation and the associated complications. It is also associated with leukocytosis and fever in more severe cases. Sepsis and peritonitis were rare findings in our case series (16.6%).
Generally speaking, the treatment of periduodenal perforations secondary to ERCP should be oriented according to the clinical and radiological findings. Non-surgical management is becoming more frequent 2 but the challenge is to identify patients who would benefit from a conservative treatment 11.
The type of surgery depends on the type, size and location of the perforation and the state of the duodenum at the time of perforation 15. With regard to the indications for surgery, the following situations should be considered as indicative: moderate contrast extravasation during ERCP, duodenal perforation caused by the endoscope (type I), retroperitoneal collections in the imaging test, massive subcutaneous emphysema with an endoscopic image of a large duodenal diverticulum, a documented perforation with an unresolved choledocholithiasis, failure of conservative treatment and a poor evolution with signs of sepsis 16. Thus, type I perforations require immediate surgical intervention whereas type II and III perforations allow a conservative management in the absence of associated retroperitoneal collections and/or signs of sepsis or peritoneal irritation. Type IV perforations respond to conservative management.
BIBLIOGRAFÍA
1. Palomeque A, González C, Pérez D, et al. Tratamiento conservador de la perforación duodenal tras realización de colangiopancreatografía endoscópica terapéutica. Gastroenterol Hepatol 2015;38:285-6. DOI: 10.1016/j.gastrohep.2014.03.016 [ Links ]
2. Lee SM, Cho KB. Value of temporary stents for the management of perivaterian perforation during endoscopic retrograde cholangiopancreatography. World J Clin Cases 2014;2:689-97. DOI: 10.12998/wjcc.v2.i11.689 [ Links ]
3. Repiso A, Gómez-Rodríguez R, García-Vela A, et al. Estudio por ecoendoscopia de la vía biliar extrahepática en pacientes con pancreatitis aguda biliar. Rev Esp Enferm Dig 2008;100(6):337-42. DOI: 10.4321/S1130-01082008000600005 [ Links ]
4. Yilmaz B, Roach EC, Koklu S, et al. Air leak syndrome after endoscopic retrograde cholangiopancreatography: a rare and fatal complication. World J Gastroenterol 2015;21:4770-2. DOI: 10.3748/wjg.v21.i15.4770 [ Links ]
5. Talukdar R. Complications of ERCP. Best Pract Res Clin Gastroenterology 2016;30(5):793-805. DOI: 10.1016/j.bpg.2016.10.007 [ Links ]
6. Priego P, Rodríguez G, Mena A, et al. Hematoma subcapsular hepático tras CPRE. Rev Esp Enferm Dig 2008;99(1):49-60. [ Links ]
7. Ozgonul A, Cece H, Sogut O, et al. Pneumoperitoneum, pneumoretroperitoneum and bilateral pneumothorax caused by ERCP. J Pak Med Assoc 2010;60:60-1. [ Links ]
8. Tavusbay C, Alper E, Gökova M, et al. Management of perforation after endoscopic retrograde cholangiopancreatography. Ulus Travma Acil Cerrahi Derg 2016;22(5):441-8. DOI: 10.5505/tjtes.2016.42247 [ Links ]
9. Stapfer M, Rick Selby R, Stain SC, et al. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg 2000;232:191-8. DOI: 10.1097/00000658-200008000-00007 [ Links ]
10. Cho KB. The management of endoscopic retrograde cholangiopancreatography-related duodenal perforation. Clin Endosc 2014;47:341-5. DOI: 10.5946/ce.2014.47.4.341 [ Links ]
11. Machado NO. Management of duodenal perforation post-endoscopic retrograde cholangiopancreatography. When and whom to operate and what factors determine the outcome? A review article. JOP 2012;13:18-25. [ Links ]
12. García-Cano Lizcano J, González Martín JA, Morillas Ariño J, et al. Complicaciones de la colangiopancreatografía retrógrada endoscópica. Estudio en una unidad pequeña de CPRE. Rev Esp Enferm Dig 2004;96(3):163-73. [ Links ]
13. Armas MD, Ojeda V, Roque C, et al. Perforaciones duodenales tras colangiopancreatografía retrógrada endoscópica. Cir Esp 2015;93:403-10. DOI: 10.1016/j.ciresp.2015.01.004 [ Links ]
14. Vowinkel T, Senninger N. Retroperitoneal emphysema after endoscopic retrograde cholangiopancreatography. Chirurg 2015;86:462-7. DOI: 10.1007/s00104-014-2829-4 [ Links ]
15. Wu HM, Dixon E, May GR, et al. Management of perforation after endoscopic retrograde cholangiopancreatography (ERCP): a population-based review. HPB (Oxford) 2006;8(5):393-9. DOI: 10.1080/13651820600700617 [ Links ]
16. Knudson K, Raeburn CD, McIntyre RC Jr, et al. Management of duodenal and pancreaticobiliary perforations associated with periampullary endoscopic procedures. Am J Surg 2008;196:975-81. DOI: 10.1016/j.amjsurg.2008.07.045 [ Links ]
Received: September 18, 2017; Accepted: January 18, 2018











 texto en
texto en