Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO  Similares en Google
Similares en Google
Compartir
Revista Española de Cirugía Oral y Maxilofacial
versión On-line ISSN 2173-9161versión impresa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.27 no.2 Madrid mar./abr. 2005
Artículo Clínico
Conservative treatment of condyle fractures:
Radiological and clinical evaluation
Tratamiento conservador de las fracturas del cóndilo:
Evaluación radiológica y clínica
A. Wassouf, R. Verdeja, K.W. Grätz
|
Abstract: Benefits of surgical treatment for condylar fractures are to date discussed controversially
in the literature. As conservative treatment is the method of choice in our
clinic, the purpose of this study is to evaluate the outcomes of a randomised
selected group of our patients who received conservative treatment for condylar fractures. Key words: Fractures; Maxillo-mandibular fixation; Radiological dislocation. |
Resumen: Las ventajas del tratamiento quirúrgico de las fracturas del proceso condilar hasta la fecha han
despertado controversia en la literatura. El tratamiento conservador es el
método de elección en nuestra clínica, por lo tanto, el propósito de este
estudio es evaluar los resultados obtenidos en un grupo de nuestros pacientes,
seleccionados y aleatorizados, que recibieron un tratamiento conservador de
fracturas del proceso condilar. Palabras clave: Fracturas; Fijación maxilomandibular; Luxación radiológica. |
Recibido: 10-09-2003
Aceptado: 06-10-2004
Departamento de Cirugía Craneomaxilofacial,
Hospital Universitario de Zurich, Suiza
Correspondencia:
Dr. Raúl Verdeja
Boulevard de Pérolles 20
1700 Fribourg - Suiza
raulverdeja@hotmail.com
Introduction
Condyle fractures are considered to be one of the most common fractures of the mandible. Treating this kind of fractures is controversially discussed in the literature. Some prefer to treat it conservatively2,6 and some others prefer the surgical treatment3-9 according to the philosophy which says that shortening of the ascending ramus and displacement of the broken condyle has potentiality of (TMJ) functional limitation8.
Open reduction of condyle fracture and using of mini plates or lag screws, even they give good radiographs and functional results but they also have the potentiality of condyle resorption which could be more problematic than possible complications of the conservative treatment.5
In our department the conservative treating of these fractures without consideration to the ramus shortening or broken condyle position is the treatment of choice since we have very positives results as shown on these 12 months follow up study.
This article presents a retrospective study on 30 randomised selected patients who had 35 conservatively treated condylar fractures. Ramus shortening and the position of the fractured condyle were not limiting factors for conservative treatment in this group.
Materials and methods
30 radiological and clinical documented cases (18 males, 12 females) of condylar fractures between 1997- 2001. Age of the patients ranged between 15 and 65 years with a mean age of 25 years. The mean follow up time of the patients was 1 year.
A total number of 35 condyle fractures divided in two groups were included in this study. A unilateral group of 25 fractures and bilateral fractures group of 10 fractures in 5 patients.
9 patients had additional fractures in the mandible.
Condyle fractures were divided into 5 levels as follow according to Köhler (1951):
1. Inter-capsular fracture or high condyle fracture.
2. High neck fracture.
3. Neck fracture.
4. Low neck fracture.
5. High ramus fracture.
The treatment was 2 Weeks Maxillo-Mandibular fixation for unilateral and 3 to 4 Weeks for bilateral fractures independent from the localisation as shown on figure 1. Our goal was to show the result and compare it according to these different types of fractures.
After applying of the wire splint described by Obwegeser (1952) a maxillo-mandibular fixation (MMF) was applied for 2 weeks for the unilateral fractures, and 3-4 weeks for the bilateral fractures.
Assessing of ascending ramus shortening and dislocation of the fractured condyle were performed only for the unilateral group as described by Lindqvist & Iizuka1. In the bilateral group these measurement were not possible to assess due to the absence of the reference side. Ascending ramus shortening and anterior or posterior dislocation were performed on the panoramic X-Ray (Fig. 2) Height of the Ramus is the perpendicular distance between the mandibular line (ML) and a tangential line to the superior point of the condyle (CA) measured along the ramus line (RL) on the fractured and non-fractured sides from point (A) to point (D). Reduction of the ramus height is represented by the difference in length between the fractured and non-fractured sides without regards for the enlargement factor due to the projection. Dislocation angle (α) in the anterior-posterior direction was defined between the (RL) line and the lateral border of the broken condyle (CL). The angle (α) presents the angle between (RL) and the posterior border of the condyle (CL) on the intact side, in the anterior dislocation the value of (α) was added to the measured angle on the fractured side. In the posterior dislocation the value of (α) was subtracted from the measured angle on the fractured side (Fig. 2).
Dislocation of the broken condyle toward the medial or lateral directions was assessed on the anterior posterior cephalogram projection (PA). Angulation of the condyle is assessed as the angle between a mid-condylar line (MCL) and a line along the lateral cortical plate (LCP) of the mandibular ramus. The angle (ß) presents the angle on the brocken side. Dislocation of the fractured side is presented by the difference between the angles on the fractured and non-fractured sides. The angle ( ß') presents the intact side angle between (MCL) and (LCP), it was subtracted in case of medial dislocation (Fig. 3) and was added in case of the lateral dislocation.
Only 17 patients had the (PA) radiographs. Clinical and radiological examinations were assessed in regular intervals of 6 weeks, 3, 6 and 12 months.
Results
In the unilateral condyle fractures group (ULG) among 25 patients 8 had additional fractures in the lower jaw. The angulation of the dislocated condyle was assessed on the panoramic X-Ray for all these 25 patients. In bilateral fractures group (BLG) assessing the angulation was not possible due to the absence of a reference side. Ramus shortening was assessed only for the (ULG) also for the same reason. 12 condyles presented anterior dislocations with a mean value of 23º ranging between 1º-139º. The other 13 condyles presented Posterior dislocation with a mean value of 10º ranging between 1º-17º.
Mesial-lateral dislocation was possible to assess only for 15 patients in the (ULG) who had the (AP) projections. 12 condyles presented medial angulation with a mean value of 14º ranging between 2º-37º. The other 3 condyles presented distal dislocation with a mean value of 8º ranging between 2º-19º.
The figures 4, 5, 6, and 7 below show the previous values in details.
Ramus shortening on the broken side is detected (Fig. 2), the results are clarified in the figure 8.
Fractures kinds distribution in these 30 patients was as follow:
Inter capsular fractures: 1 fracture.
High collum fractures: 1 fracture.
Collum fractures: 6 fractures.
Low collum fractures: 14 fractures.
High ramus fractures: 3 fractures.
Maxillo-mandibular fixation (MMF) time was 2-3 weeks for the (ULG), and 3-4 weeks for the (BLG). In the (ULG) the mean time of the (MMF) was 17 days ranging between 14-23 days. The difference existed due to the case and occlusal stability after 1 and 3 days after the removal of the (MMF).
In all the (BLG) the (MMF) time was 21 days. In both groups the function and occlusion showed minimal disturbance, without individual complaints of the patient, at the last controlling. None of the cases necessitate later occlusal correction via ramus sagital splitting.
Mouth opening mean value was 46 mm and ranged between 30 and 60 mm for 28 patients, 2 patients were dropped out because no existing data about mouth opening value could be found.
Lateral movements were assessed for 15 patients, the broken side showed a mean value of 7 mm and the intake side showed 8 mm. Protrusion mean value was 5 mm for 11 patients of the (ULG) and ranged between 1- 9 mm.
5 patients of 29 showed clicking in the Temporo-mandibular joint (TMJ), one case had no information in the file about this subject.
Deviation when opening the mouth was found in 14 patients of 27 since for 3 patients it was not mentioned if they showed deviation when opening the mouth or not.
Two patients showed slight pain when palpating the broken side, they informed that it was not significant and doesn't affect the function of the (TMJ).
No case in this study showed occlusal disturbance affecting the function of the (TMJ) on any side, no case needed sagitale splitting of the ramus as an occlusion correction procedure.
No later open bite formation or worsening of the symptoms was reported.
Discussion
Conservative treatment for condylar fractures is the way of treatment in our department. By avoiding surgical intervention great benefits and high results can be achieved in this kind of fractures. Ramus shortening is creating an asymmetrical situation on the ascending ramus, but according to E. Ellis III4 three kinds of adaptation has been noticed in conservatively treated cases.
1. Adaptation within the neuromuscular system that is changing the biomechanics of the mandibular function which helps the patients to establish their normal occlusion at the end.
2. A new temporomandibular articulation is established between the mandible and the base of the skull.7
3. Dentoalveolus adaptation, when mandibular plane steeping occurs because of loos of the posterior vertical dimension, then the only way to maintain a normal occlusion is by extrusion of the anterior teeth and/or by intrusion of the posterior teeth.4
By these three adaptations the problems which can appear due to the asymmetrical situation between the broken and intact side can be over came.8
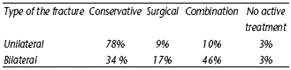
In a survey to clarify the opinions of a group of 120 maxillofacial surgeons around the world about the preferred method to treat condyle fractures, Baker et al.2 The results were as follow according to fractures kind considering that the fractured condyle is dislocated and associated with an altered occlusion. (Table 1)
From the schedule above it looks that the conservative treatment is still considered to be the treatment of choice for a lot of maxillofacial surgeons, also preference of combination between the surgical treatment with a period of (MMF) application refers to the benefit of a period of occlusion stabilising for better outcomes. In our study none of the patients presented needing for later ramus sagittal splitting or occlusion adjustment due to occlusal disturbance, a stable and balanced occlusion is obtained in this group of patients after conservative treatment. Better occlusion stability after conservative treatment is reported by E. Ellis III et al.3 when compared to surgical treated cases.
In 6 patients (4 ULG and 2 BLG) symptoms as clicking and slight pain when palpating the (TMJ) could be detected. One patient who had bilateral fracture associated with severe ramus shortening on both sides and heavy dislocation of both condyles presented both symptoms, clicking and slight pain on palpation. Ramus shortening in 4 of these 6 patients ranged between 6-10 mm with a mean value of 8 mm. It looks that when ramus shortening is more than 8 mm then the chance of clicking and pain on palpation to occur is higher.8 Deviation on opening toward the fractured side was noticed in 13 patients in the unilateral fractures group where ramus shortening ranged between 0-14 mm with a mean value of 5.9 mm. None of 9 ULG patients who had ramus shortening less than 5 mm showed clicking or pain on palpation. These results are similar to the outcomes reported by Silvennoinen et al.8 In an other study reported by Konstantinovic and Dimitrijevic6 on 80 patients where 54 patients received conservative treatment and 26 were treated surgically, no difference was found between the two treatments. However, the radiographic examinations of the same group showed a statistically better position of the surgical reduced condylar process fractures, taking in consideration that the conservatively treated fractures presented initially less dislocation when compared to the surgical group.
Due to these outcomes and our long satisfactory experience in treating condylar fracture in a conservative way by rigid (MMF) application for 2- 3 weeks in the unilateral fractures and 3- 4 weeks in the bilateral fractures, followed by a later period of elastic (MMF), it is still the treatment of choice in our department.
Conclusion
Conservative treatment of condylar fractures by maxillo- mandibular fixation (MMF) application is a safe treating method avoiding surgery with predictable good results. For unilateral condyle fractures we perform 2-3 weeks of MMF, and 3- 4 weeks for the bilateral fractures. Later short period of elastic MMF is recommended for enhanced results. Displacement severity of the broken condyle or ascending ramus shortening on the fractured side didn't prevent obtainig satisfactory results in this study.
References
1. Atlas of Craniomaxillofacial Osteosynthesis. Georg Thieme Verlag, Rüdigerstrasse 14 D-70469 Stuttgart, Germany, 1999, p.p. 63-4. [ Links ]
2. Baker AW, McMahon J, Moos KF. Current consensus on the management of fractures of the mandibular condyle – A method by questionnaire. Int J Oral Maxillofac Surg 1998; 27: 258-66. [ Links ]
3. Ellis E III. Occlusal results after open or closed treatment of fractures of the mandibular condylar process. J Oral Maxillofac Surg 2000: 58: 260-8. [ Links ]
4. Ellis E III, Simon P, Throckmorton G S. Complications of mandibular condyle fractures. Int J Oral Maxillofac Surg 1998: 27: 255-7. [ Links ]
5. Iizuka T, Lindqvest C, Hallikainen D, Mikkonen P, Paukku P. Sever bone resorption and osteoarthrosis after mini-plate fixation of high condylar fractures. A clinical and radiologic study of thirteen patients. Oral Surg 1991: 72: 400-7. [ Links ]
6. Konstantinovic VS, Dimitrijevic B. Surgical versus conservative treatment of unilateral condylar process fractures: clinical and radiographic evaluation of 80 patients. Int J Oral Maxillofac Surg 1992: 50: 349-53. [ Links ]
7. Lindahl L, Hollender L. Condylar fractures of the mandible. II. Radiographic study of remodeling processes in the tempomandibular joint. Int J Oral Surg 1997: 6: 153-65. [ Links ]
8. Silvennoinen U, Rausita AM, Lindqvist C, Oikarinen K. Occlusal and tempomandibular joint disorder in patients with unilateral condylar fracture. A prospective one- year study. Int J Oral Maxillofac Surg 1998; 27: 280-5. [ Links ]
9. Eckelt U. Zugschraubenosteosynthese bei Unterkiefergelenkforsatzfrakturen. Dtsch Z Mund Gesichts Chir 1991; 15: 51-7. [ Links ]











 texto en
texto en