Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Cirugía Oral y Maxilofacial
versión On-line ISSN 2173-9161versión impresa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.27 no.5 Madrid sep./oct. 2005
Artículo Clínico
Prognostic factors in primary malignant salivary gland neoplasms.
A 20-year retrospective study
Factores pronósticos en neoplasias malignas primarias de glándulas salivares.
Estudio retrospectivo de 20 años*
A. Capote Moreno1, L. Naval Gías2, F.J. Rodríguez-Campo2, M.F. Muñoz Guerra2, V. Escorial1, F.J. Díaz González3
|
Abstract: Objective. To analyze the possible prognostic factors for
survival and disease-free survival in a group of patients with primary
malignant salivary gland tumors. Key words: Salivary Gland Carcinoma; Survival; Disease-Free Survival; Facial Palsy.
|
Resumen: Objetivo. Analizar los posibles factores
pronósticos que pueden influir en la supervivencia y el desarrollo de
recurrencias en nuestra serie de pacientes con neoplasias malignas
primarias de glándulas salivares. Palabras clave: Carcinoma de Glándula Salivar; Supervivencia; Periodo Libre de Enfermedad; Parálisis Facial. |
Recibido: 15.11.2004
Aceptado: 05.01.2005
1 Médico Residente.
2 Médico Adjunto.
3 Jefe de Servicio.
Servicio de Cirugía Oral y Maxilofacial. Hospital Universitario de La Princesa.
Universidad Autónoma de Madrid. Madrid, España.
*Presentado como comunicación oral en el XVII Congreso Nacional de la
Sociedad Española de Cirugía Oral y Maxilofacial. Sevilla, Mayo 2003.
Correspondencia:
Dra. Ana Capote Moreno
C/ Valderribas 10, esc. drcha, 5ºH.
28007 Madrid, España.
e-mail: anacapote@inicia.es
Introduction
Primary malignant salivary gland neoplasms make up a heterogeneous group of tumors with diverse histologic characteristics that have a varied response to different therapeutic models. These neoplasms represent 10-15% of all glandular tumors and 1-3% of malignant tumors of the head and neck.1,2
These tumors are commonly located in the parotid gland, although the relative proportion of malignancy is superior in minor salivary gland tumors, while in the major salivary glands neoplasms of a benign nature predominate.3 With regard to prognosis, clear cell carcinoma and low-grade mucoepidermoid carcinoma have better survival rates than other histologic variants such as adenocarcinoma, cystic adenoid carcinoma or epidermoid carcinoma.4-6
Glandular surgery is still the treatment of choice for this type of neoplasm, and this has been backed by previous multicenter studies2 and by authors with an ample case experience. Radiotherapy is reserved as adjuvant therapy for those patients with bad prognosis factors, or as palliative treatment in those cases in which surgery is ruled out. There is no doubt as to the indication for neck dissection when there are clinically positive nodes. However, elective dissection in salivary gland cancer continues being a controversial issue.4,7
Various prognostic factors have been described that are related to the survival of these neoplasms as well as to a greater risk of developing locoregional recurrence or distant metastasis. Factors such as tumor size, cervical metastasis, the degree of malignancy or the histologic type are classic factors related with the prognosis of these tumors.4,8-10 In this way, factors related with the patient such as sex and age have been described as independent variables in survival studies.8 Recently, the presence of pain and facial palsy at diagnosis has been correlated with a worse prognosis for these neoplasms.2,6
The objective of this study was to identify the possible prognosis factors that can affect the progression of patients in our series of primary malignant salivary gland tumors, by analyzing the relationship with survival rates and recurrence development.
Material and methods
A retrospective study was carried out of 75 patients (41 males and 34 females; mean age 59.17 years; age range 17 to 91 years), with primary malignant epithelial tumors of salivary glands treated between 1980 and 2003 by the Service of Oral and Maxillofacial surgery of the University Hospital of La Princesa, Madrid. The analysis of melanomas, lymphomas, sarcomas and carcinoma metastases was excluded. Patient follow-up was entered periodically into the tumor data base (MSDOS-dBASE) that exists in the Service. It was considered that the minimum follow-up period of the series should be 12 months (mean follow-up 56.93 months).
The group of patients that was studied was made up of 25 cases (33.3%) with clinical stage I, 5 cases (6.7%) with stage II, 34 cases (45.3%) with stage III, 10 cases (13.3%) with stage IV and one case that was not staged, as it was a hidden tumor (Tx). The staging of these tumors, clinically as well as pathologically, was carried out according to the criteria of the TNM classification of the American Joint Committee on Cancer.11
In the preoperative study FNA diagnosis was used in 33 patients (44%), while a diagnostic biopsy was carried out on 39 patients (52%). The cervicofacial CAT scan or Magnetic Resonance were the diagnostic tests used for the study of locoregional extension.
The treatment carried out in all cases was surgical with local resection of the tumor combined with neck dissection in 28 patients (37.3%) due to the clinical or radiographic suspicion of positive cervical adenopathy, or in an elective manner in neoplasms with high-grade malignancy. The removal of the primary tumor implied carrying out an osteotomy of the subjacent bone in 27 patients (36%). In one case radiotherapy was administered preoperatively in order to reduce tumor volume.
Adjuvant postoperative radiotherapy was used in those cases meeting the established criteria of the Hospitals Tumor Protocol Committee: two or more positive cervical nodes, nodal extracapsular spread, tumors with high-grade malignancy or with regional extension, unclear surgical resection margins and perineural spread of the tumor.
In the statistical study of crude and cause-specific survival as well as of disease-free intervals, the Kaplan-Meier method was used. In this way, the possible prognostic factors implied in the progression of these tumors was analyzed, using the Log Rank test for the univariate study of causespecific survival and for disease-free intervals. The factors studied were: Sex, location, the presence of pain and/or facial palsy at diagnosis, tumor size (pT), tumor stage (pTNM), histologic type, surgical margins, perineural spread, lymphatic spread and vascular spread. In order to identify the independent factors in the multivariate analysis, the Cox proportional hazards model (hazard ratio) was used. In these tests, the accepted significance level was p<0.05. The statistical study was carried out using the SPSS 8.1 program.
Results
In the patient series studied, 34 cases (45.3%) were related to tumors located in the parotid gland (one of them in an accessory gland), while in 33 cases (44%) they were located in a minor salivary gland, and in 8 cases (10.7%) in the submaxillary gland. The histology of these tumors has shown great diversity in the global group, with cystic adenoid carcinoma being the most common neoplasm in 18 patients (24%), followed by adenocarcinoma in 11 patients (14.7%) and low-grade mucoepidermoid carcinoma, high-grade mucoepidermoid carcinoma and glandular epidermoid carcinoma in 7 patients respectively (9.3%) (Table 1). However, cystic adenoid carcinoma was the predominant neoplasm in minor salivary glands (12 cases; 36.4%), while the adenocarcinoma was the most common histologic type in the major salivary glands (7 cases; 20.6%).
Affected facial nerves were observed at diagnosis in 11 patients (14.7%), together with paralysis in one or various branches of the nerve or of its main trunk, while 22 patients (29.3%) had pain at diagnosis.
Postoperative adjuvant radiotherapy was used for 52% of tumors (39 patients) according to the criteria described previously. Of these 39 patients, 31 cases (79.5%) were related to advanced stages of the disease (stages III and IV) and only 8 cases (20.5%) were in the early stage (stages I and II).
With regard to anatomopathologic size, 16 patients were identified with pT1, 16 patients with pT2, 3 patients with pT3 and 40 patients with pT4. Of the 28 patients that underwent cervical dissection, 17 patients had nodal metastases that were clinically positive at diagnosis. However, in 26.7% of cases (20 patients) there was either one or various positive nodes in the definitive histologic study and, as a result, hidden nodal metastases was identified in three patients (4%). The distribution in the series according to pathological staging was: 16 patients (21.3%) with stage I, 10 patients (13.3%) with stage II, 3 patients (4%) with stage III and 46 patients (61.3%) with stage IV.
The correct surgical margins were those that were tumor free and at a greater distance or equal to 5mm from the tumor. Therefore in the series, 31 patients (41.3%, 17 patients with early-stage and 14 patients with late-stage disease) were considered to have correct margins, while 44 patients (58.7%; 10 patients with early-stage and 34 patients with late-stage disease) had affected margins. Perineural spread by tumor cells in 24 patients (42.1%) of the 57 patients analyzed was identified. Likewise, 11 out of the 37 patients analyzed (29.7%) had lymphatic spread and 3 out of 39 patients analyzed (7.7%) had vascular spread.
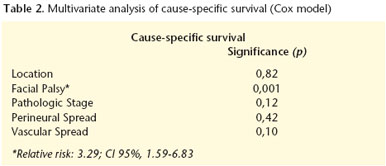
Crude survival in the series, using the Kaplan-Meier method, was 74.9% at five years and 63% at 10 years. Cause-specific survival showed similar rates with 77.7% at 5 years and 65.3% at 10 years. Of all the possible prognostic factors studied in the univariate analysis, the following had a statistically significant influence in survival rates of the series: tumor location (p=0.03), pathological staging (p=0.006), the presence of facial palsy at diagnosis (p=0.02) (Fig. 1), perineural spread (p=0.03) and vascular spread (p=0.001) (Fig. 2). Other factors such as sex, the size of the tumor, the presence of pain at diagnosis, surgical margins, histologic type or lymphatic spread did not reach a significant statistical level. On analyzing these significant variables using the Cox proportional model, the only variable that showed a statistically significant influence in the multivariate survival analysis was the presence of facial palsy at diagnosis (Table 2). During the follow-up period, 32 patients (43.8%) suffered recurrence of tumor growth (Table 3) while 41 patients (56.2%) did not suffer locoregional or distant recurrence. The recurrence rate for tumors located in the major glands was 53.7% (22 cases) as opposed to 31.3% for minor glands (10 cases). Disease free survival showed rates of 51.8% at 5 years and 43.2% at 10 years. In the Log Rank analysis of the disease-free interval, the factors that were statistically significant were sex (p=0.004), tumor location (p=0.04), pathological stage (p=0.0001), tumor size (p=0.001), facial palsy at diagnosis (p=0.04) (Fig. 3), and vascular spread (p=0.0002) (Fig. 4). Thus, the factors that turned out to be statistically significant in the multivariate analysis were facial palsy at diagnosis and vascular spread (Table 4).
With regard to surgical margins, the group of patients with correct margins showed better progression with regard to survival and disease- free intervals, although these results did not reach statistical significance (p<0.05).
Of the 48 patients diagnosed with advanced stage tumors, 31 (64.6%) received postoperative radiotherapy. On analyzing the influence of radiotherapy in patient progression by means of the Log Rank survival test and disease-free intervals, this turned out to be insignificant in both statistical analyses (cause-specific survival: p=0.2; diseasefree survival: p=0.3).
Discussion
Primary carcinomas of the salivary glands are considered an uncommon neoplasm in the area of the head and neck. Due to this infrequency and to the considerable histologic diversity, there are very few global studies analyzing the factors that intervene in the behavior of these neoplasms, as most of these concentrate on neoplasms of the major salivary glands.2,4
Crude survival in the series presented (77.4% at 5 years) has shown similar values to those described by various authors (between 81%- 65% at five years),2,6,12 Various studies have tried to analyze and identify the possible factors related to the prognosis of these patients that carry a greater risk of recurrence. Classically, significant variables include tumor size (T), clinical stage (TNM) and histologic type.6,12-14 In our analysis we have not identified a significant relationship between these factors and survival, while the size of the tumor was a relevant factor in relation with disease-free intervals (p=0.0001). For statistical study purposes the pathological stage was taken into account, as the histologic analysis confirmed the extension of the tumor as well as the degree of lymph node involvement. This factor has had statistical significance in univariate studies, despite not turning out to be an independent prognostic factor.
For various authors such as Therkildsen et al,12 OBrien et al15 or Spiro el al,16 tumor location does not seem to influence survival in multivariate analyses. This fact is confirmed in our study as, in spite of being significant in the log rank test, it looses value in the Cox model.
Neoplastic cell involvement of the seventh pair of cranial nerves before surgical treatment significantly worsens the prognosis for these tumors.2,4-6 In this study the influence of facial palsy in a worse patient prognosis was demonstrated, together with a strong association with survival as well as recurrence. Another clinical characteristic described in the literature with a negative prognostic factor is the presence of preoperative pain.13 Nevertheless, this factor does not have statistical significance according to the results obtained in the analysis we have described.
Although perineural spread and survival has been widely studied,4,10 in very few articles has there been an attempt at correlating survival with the presence of lymphatic or vascular spread. In this analysis the strong influence of vascular spread was demonstrated, even as an independent factor, as it appears to favor an increase in recurrence significantly. This fact could be relevant for opening new lines of investigation and for establishing therapeutic alternatives for tumors with intra and peritumoral blood vessel involvement.
One of the objectives of surgery is to achieve tumor cellfree margins, which has classically been considered to be one of the most relevant factors for improving patient prognosis. 2,5,9,12 In our study, the presence of correct surgical margins is suggestive of a better prognosis for these patients, despite the result not showing a statistical significance in survival curves and disease-free intervals.
The existence of nodal metastasis at diagnosis is a clear indication for surgical treatment of the neck with routine neck dissection. However, the indications for elective neck treatment continue being a controversial issue.1,17 While in the study series, a crude incidence of nodal metastases was identified of 26.7%, the hidden metastasis rate was 4%, a relatively low rate with regard to other authors.4,17 According to Armstrong et al,17 the risk of hidden nodal metastasis in major salivary gland tumors is associated with the size of the tumor and with the histologic grade. Therefore, in certain cases with associated risk factors, elective surgery of the neck should be carried out. The criteria determining this indication vary from one author to the other according to the results obtained in the studies. In general, carrying out elective neck dissection is recommended for tumors with a high degree of malignancy and for locally aggressive tumors with regional extension.12,17
Postoperative radiotherapy in conjunction with surgical treatment for primary tumors has been demonstrated as significantly influencing the progression of these patients.7,12,17- 21 This has been observed principally in improvements in the rates of locoregional control following radiotherapy.2,19-21 In spite of there not being universal criteria as to the indications of radiotherapy for salivary gland neoplasms, there is a certain concordance among various authors as to what cases are eligible for treatment. The existence of pathologic adenopathy, tumors with a high degree of malignancy or in advanced stages (III and IV), locally aggressive tumors (T3 and T4), affected surgical margins, perineural spread form the principal criteria that determine the need for complementary irradiation of the surgical bed and the affected neck.2,10,13,18 Nevertheless, in the series presented the beneficial effect of postoperative radiotherapy has not been demonstrated with regard to recurrence control and survival improvement. This could be due to changes over time in the selection criteria used for the patients that are eligible for this treatment, as well as to the absence of groups with similar characteristics that would have allowed comparisons of the different therapeutic modalities.
Discussion
In conclusion, it can be affirmed that malignant neoplasms of salivary glands form a heterogeneous group of tumors with diverse characteristics and behavior that makes carrying out survival studies and identifying the different risk factors difficult. Tumor location, sex, pathologic stage, the presence of facial palsy at diagnosis, perineural and vascular spread have turned out to be prognostic factors for survival and/or recurrence in the univariate analysis of this study, with facial palsy and vascular spread being independent factors. Complementary radiotherapy does not appear to improve survival in patients in the series presented, and no significant differences were found between this treatment and isolated surgical treatment.
References
1. Bhattacharyya N, Fried MP. Nodal metastasis in major salivary gland cancer. Predictive factors and effects on survival. Arch Otolaryngol Head Neck Surg 2002;128:904-8. [ Links ]
2. Tullio A, Marchetti C, Sesenna E, Brusati R, Cocchi R, Eusebi V. Treatment of carcinoma of the parotid gland: results of a multicenter study. J Oral Maxillofac Surg 2001;59:263-70. [ Links ]
3. Rinaldo A, Shaha AR, Pellitteri PK, Bradley PJ, Ferlito A. Management of malignant sublingual salivary gland tumors. Oral Oncology 2004;40:2-5. [ Links ]
4. Régis de Brito Santos I, Kowalski LP, Cavalcante de Araujo V, Flávia Logullo A. Multivariate analysis of risk factors for neck metastases in surgically treated parotid carcinomas. Arch Otolaryngol Head Neck Surg 2001;127:56-60. [ Links ]
5. Bhattacharyya N. Survival and prognosis for cancer of the submandibular gland. J Oral Maxillofac Surg 2004;62:427-30. [ Links ]
6. Carinci F, Farina A, Pelucchi S, y cols. Parotid gland carcinoma:1987 and 1997 UICC T classifications compared for prognostic accuracy at 5 years. Eur Arch Otorhinolaryngol 2001;258:150-4. [ Links ]
7. Lee S, Kim GE, Park CS, y cols. Primary squamous cell carcinoma of the parotid gland. Am J Otolaryngol 2001;22:400-6. [ Links ]
8. Wahlberg P, Anderson H, Biörklund A, Möller T, Perfekt R. Carcinoma of the parotid and submandibular glandsæa study of survival in 2465 patients. Oral Oncol 2002;38:706-13. [ Links ]
9. Brandwein M, Ivanov K, Wallace DI y cols. Mucoepidermoid carcinoma. A clinicopathologic study of 80 patients with special reference to histologycal grading. Am J Surg Pathol 2001;25:835-45. [ Links ]
10. Kokemueller H, Eckardt A, Brachvogel P, Hausamen JE. Adenoid cystic carcinoma of the head and neck: a 20 years experience. Int J Oral Maxillofac Surg 2004;33:25-31. [ Links ]
11. Greene FL, Page D, Morrow M, y cols. (eds.) AJCC Cancer Staging Manual, 6th ed. New York: Springer, 2002. [ Links ]
12. Therkildsen MH, Christensen M, Andersen LJ, y cols. Salivary gland carcinomas: prognostic factors. Acta Oncol 1998;37:701-12. [ Links ]
13. Camilleri IG, Malata CM, McLean NR, Kelly CG. Malignant tumors of the submandibular salivary gland: a 15-year review. Br J Plast Surg 1998;51:181-5. [ Links ]
14. Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2807. Head Neck Surg 1986;8:177-84. [ Links ]
15. O´Brien CJ, Soong S, Herrera GA, Urist MM, Maddox WA. Malignant salivary tumors-analysis of prognostic factors and survival. Head Neck Surg 1986;6:82-92. [ Links ]
16. Spiro RH, Thaler HT, Hicks WF, Kher Ua, Huvos AH, Strong EW. The importance of clinical staging of minor salivary gland carcinomas. Am J Surg 1991;162:330-6. [ Links ]
17. Armstrong JG, Harrison LB, Thaler HT, y cols. The indications for elective treatment of the neck in cancer of the major salivary glands. Cancer 1992;69:615-9. [ Links ]
18. Harrison LB, Armstrong JG, Spiro RH, Fass DE, Strong E. Postoperative radiation therapy for major salivary gland malignancies. J Surg Oncol 1990;45:52-5. [ Links ]
19. Armstrong JG, Harrison LB, Spiro RH, Fass DE, Strong EW, Fuks ZY. Malignant tumors of major salivary gland origin: a matched pair analysis of the role of combined surgery and postoperative radiation therapy. Arch Otolaryngol Head Neck Surg 1990;116:290-3. [ Links ]
20. North CA, Lee DJ, Piandosi S, Zahurak M, Johns ME. Carcinoma of the major salivary glands treated by surgery or surgery plus postoperative radiotherapy. Int J Radiat Oncol Biol Phys 1990;18:1319-23. [ Links ]
21. Borthne A, Kjellevold K, Kaalhus O, Vermund H. Salivary gland malignant neoplasms: treatment and prognosis. Int J Radiat Oncol Biol Phys 1986;12:747-54. [ Links ]











 texto en
texto en