Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Cirugía Oral y Maxilofacial
versión On-line ISSN 2173-9161versión impresa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.29 no.6 Madrid nov./dic. 2007
CASO CLÍNICO
Enfermedad de Castleman de localizacion cervical
M.T. Martínez Iturriaga1, M.E. Reguero Callejas2, A. Prieto Fenech3, I. Alvarez4, E. Sánchez-Jauregi5, J.L. Martínez Laje6
1 Médico Residente. Servicio de Cirugía Oral y Maxilofacial
2 Médico Residente. Servicio de Anatomía Patológica
3 Jefe de Sección. Servicio de Cirugía Oral y Maxilofacial
4 Médico adjunto. Servicio de Cirugía Oral y Maxilofacial
5 Médico Residente. Servicio de Cirugía Oral y Maxilofacial
6 Jefe de Servicio. Servicio de Cirugía Oral y Maxilofacial
Hospital Ramón y Cajal. Madrid, España
ABSTRACT
Castleman´s Disease is characterized by the presence of lymphatic tissue masses. There are two forms the hyaline vascular 91% (unifocal) and the plasmatic 9% (multifocal). We present a 30 year old man with a left laterocervical painless mass. Total resection of the tumour was performed. The histological result was Castleman´s disease hyaline vascular form. Castleman´s disease presents mainly in the lymphatic tissue of the mediastinum. Cervical location is very rare. Periphery metastasis work up must be done to rule out the multifocal form of the disease. Surgical excision is curative for the unifocal form.
Key words: Castleman´s disease; Cervical mass; Lymphatic tissue.
RESUMEN
La enfermedad de Castleman se caracteriza por la presencia de masas de tejido linfático; existen dos variedades la hialino vascular 91% (localizada) y plasmática 9% (multicéntrica). Presentamos un varón de 30 años con tumoración latero cervical izquierda indolora. Se realizó una exéresis total de la lesión. La histología es Enfermedad Castleman variante hialino vascular. La enfermedad de Castleman se presenta fundamentalmente en el tejido linfático mediastínico. La localización cervical es muy rara. Se debe realizar un estudio de extensión para descartar la forma multicentrica de la enfermedad. En la forma localizada la extirpación de la lesión implica la curación de la enfermedad.
Palabras clave: Enfermedad de Castleman; Masa cervical; Tejido linfático.
Introduction
Castlemans disease (giant lymph node hyperplasia, lymph node hamartoma) is a rare disorder that is more a particular form of lymphoid hyperplasia than a tumor or hamartoma. The tumor is of unknown origin and it is characterized by the presence of pseudotumoral masses of lymphatic tissue. It occurs in children or young adults and has no sexual or racial predominance.
It was first described in 1954 and later characterized by Castleman in 1956.1-3
Two varieties exist. The vascular hyaline variety (91%) is characterized by intense follicular proliferation with hyaline vascular changes in the germinal centers of the lymph node. It usually affects the mediastinum. The other one is the plasma cell variety (9%), which is characterized by the proliferation of plasma cells in the ínterfollicular areas of the lymph node without hyaline vascular changes in the follicles. This form is usually extramediastinal. A very infrequent mixed form also exists.4
The case presented here involved an extramediastinal location, which is highly uncommon for the hyaline vascular variant, which is usually located in the mediastinum.
Clinical case
A 30-year-old man without a medical or surgical history of interest consulted for a left lateral cervical tumor of several months evolution. The patient referred nocturnal sweating in recent months as the only notable finding in his history.
In the examination, a tumor of 5x5 cm diameter was found medial to the lower third of the sternocleidomastoid muscle (SCM). It was of elastic consistency, poorly defined, not adhered to deep planes or to skin, did not vary in size with postural changes, was nonpulsatile, and had negative auscultation.
Fine needle aspiration biopsy guided by computed tomography (CT) was requested. It was reported as lymph node cellularity with indeterminate changes that were not cytologically typifiable. Viral serologic study was recommended.
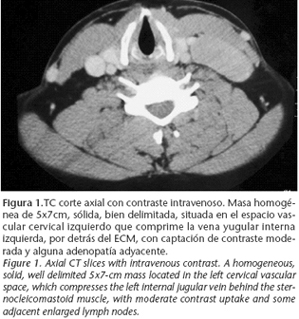
CT with intravenous contrast revealed a homogeneous, solid, well delimited, 5x7 cm mass that was located in the left cervical vascular space and compressed the left internal jugular vein behind the SCM. It showed moderate contrast uptake and some adjacent enlarged lymph nodes (Fig. 1). The mass did not exhibit the increased uptake of carotid glomus. The radiographic differential diagnosis included lymphoproliferative process, neurogenic tumor, and mesenchymal tumor.
A horizontal left supraclavicular incision was made under general anesthesia and the SCM muscle was sectioned at the same level to obtain adequate exposure. A 5x7 cm tumor of congestive appearance was found. It was hard and had prolific peripheral vascularization that made dissection difficult. The tumor had a plane of separation from the vascular space.
The clinical appearance at the time of the intervention impressed the authors as characteristic of a vascular tumor (Fig. 2).
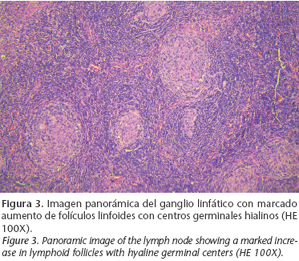
The histopathologic study of the piece confirmed that it was a lymph node with conserved architecture, a marked increase in the number of lymphoid follicles
(Fig. 3), and positivity for immunohistochemical markers (CD20+CD10+, bcl2-)
(Fig. 4). Characteristically, the germinal centers presented hyaline material, vessels, and an "onion-layer" disposition of the lymphocyte crown
(Fig. 5).
The number of plasma cells (CD138) was within the range of normality and showed no restriction for immunoglobulin light chains (kappa and lamda). In the molecular study, the PCR technique did not detect the presence of human herpes virus type 8 (HHV 8).
Thoraco-abdomino-pelvic CT showed results within the range of normality. The complete analytical study, immunological study, and serology were normal. These findings were consistent with the localized form of lymphoid angiofollicular hyperplasia, or Castlemans disease, hyaline vascular variant.
Discussion
The many names (lymph node hamartoma, giant lymph node hyperplasia, lymphoid angiofollicular hyperplasia, Castlemans lymphoma, etc) by which Castlemans disease is known demonstrate that the pathogenesis of the condition is still uncertain. It occurs between the ages of 2 and 71 years and is more frequent in adults. The lesions can appear in thorax (60%), neck (14%), abdomen (30%), and axilla (4%).
Castlemans disease can occur in a local and single-focus form (80-90%), which is benign and resolves after surgical resection of the lymphatic mass, or in an extended and multifocal form (10-20%) with systemic symptoms and a more aggressive clinical course.5 The most common location of this lymphatic proliferation, probably reactive, is the mediastinum (60%), followed by the abdomen (14%), neck (13%), and axilla (4%). However, it can appear anywhere that lymph nodes exist. Cases have been reported in the parotid gland, pancreas, adrenal glands, liver, penis, and vulva.2,6 In the maxillofacial territory, the most frequent location is the lymph nodes of the neck. In the literature we found reports of involvement of the parotid (7 cases), submaxillary gland (2 cases), floor of the mouth (1 case), parapharyngeal space (1 case), larynx (1 case), and palate (1 case). The clinical diagnosis of cervical Castlemans disease is difficult because most patients only present a painless cervical mass without fever or anemia. In the vascular hyaline form there are usually no analytical abnormalities and the fine needle aspiration biopsy (PAAF) is generally inconclusive. The diagnosis was made after surgical excision of the lesion, which is curative.
Patients with multifocal Castlemans disease exhibit clinical or radiological evidence of generalized lymph node involvement. Histopathologic evidence of the disease should be present in at least one lymphatic region. Patients are usually older (mean age 56 years) and have systemic symptoms like hepatosplenomegaly, hypochromic and microcytic anemia that does not respond to iron treatment, hypergammaglobulinemia, and accelerated ESR. The affected lymph nodes may secrete an antierythropoietic substance responsible for the anemia.
Histologically, the disease is usually the plasma cell type. The multifocal variant is more aggressive and can transform itself into lymphoma or Kaposis sarcoma, which is exceptional in the hyaline variant.
The radiographic findings are relatively nonspecific.
Ultrasonographic findings are similar to those of lymphoma. 11
In angiographic studies, an intense pattern of peripheral neovascularization in the lesion has been described,12 which we confirmed during the excision of the tumor in the present case, which made the intervention more difficult and prolonged.
The CT findings reveal a homogenous mass that exhibited early enhancement with contrast in the hyaline vascular form.11 In the case presented, moderate uptake excluded a carotid glomus.
Published MRI findings are scant and nonspecific.12
The patient has to undergo a study of the extension, including thoraco-abdomino- pelvic CT, in search of disseminated disease, complete blood tests with ESR, complete immunological study, and serology.
The differential diagnosis must be made with lymphoma, metastasis, granulomatous disease, sarcoma, branchial cyst, thyroid mass, and neural tumors because they may show radiographic images similar to Castlemans disease.11
Treatment of the affected lymph node masses must be surgical, which is curative; recurrence is rare.3, 14
Radiation therapy has not been shown to produce disappearance or a reduction in the size of the lymphatic masses2,3 in head and neck.
The patient presented had a follow-up period of 16 months in which we have not detected signs of recurrence.
Conclusion
Castlemans disease is a rare disorder of the lymph nodes of unknown origin. Although its most frequent form of presentation is as a mediastinal mass, it must be considered in the differential diagnosis of cervical tumor. Surgical excision is curative in localized forms (90%), but the extension must always be studied to rule out disseminated disease.
![]() Correspondence:
Correspondence:
Dra. M.T. Martínez Iturriaga
C/ Julio Caro Baroja 84,
28050 Madrid, España
Email: 1@colmeitu.e.telefonica.net
Received: 23.10.06
Accepted: 04.06.07
References
1. Castleman B, Iverson L, Menendes V. Localized mediastinal lymph-node hyperplasia resembling thymoma. Cancer 1956;9:822-30. [ Links ]
2. Keller AR, Hochholzer L, Castleman B. Hyalinevascular and plasma cell types of giant lymph node hyperplasia of mediastinum and other locations. Cancer 1972; 29:670-83. [ Links ]
3. Bowne WB, Lewis JJ, Filippa DA, Niesvizky R, Brooks AD, Burt ME, Brennan MF.The management of unicentric and multicentric Castleman´s disease: a report of 16 cases and a review of the literature. Cancer 1999;85:706-17. [ Links ]
4. Shahidi H, Myers JL, Kuale PA. Castleman´s disease. Mayo Clinic Proc 1995;70: 969-77. [ Links ]
5. Herrada J, Cabanillas F, Rice L, Maning J, Pugh W. The clinical behaviour of localizad and multicentric Castleman disease. Ann Intern Med 1998;128:657. [ Links ]
6. Anagnostou D, Harrison CV. Angiofollicular lymph node hyperplasia (Castleman). J Clin Pathol 1972;25:306-11. [ Links ]
7. Gangopadhyay K, Mahasin ZZ, Kfoury H. Castleman disease (giant lymph node hyperplasia). Arch Otolaryngol Head Neck Surg 1997;123:1137. [ Links ]
8. Yi AI, de Tar M, Becker TS, y cols. Giant lymph node hyperplasia of the head and neck (Castlemans disease): A report of five cases. Otolaryngol Head Neck Surg 1995;113:462. [ Links ]
9. Goodisson DW, Carr RJ, Stirling RW. Parotid presentation of Castlemans disease: report of a case. J Oral Maxillofac Surg 1997;55:515. [ Links ]
10. Sanchez Cuellar A, de Pedro M, Martin-Granizo R, Berguer A. Castleman disease (giant lymph node hyperplasia) in the maxillofacial region: A report of 3 cases. J Oral Maxillofac Surg 2001;54:228-31. [ Links ]
11. Yamashita Y, Hirai T, Matsukawa T, Ogata I, Takahashi M. Radiological presentations of Casleman´s disease. Comput Med Imaging Graph 1993;17:102-17. [ Links ]
12. Inoue Y, Nakamura H, Yamazaki K, Mizumoto S, Kokubu I, Mori H. Retroperitoneal Castleman´s tumors of Hyaline vascular type: imaging study. Clin Imaging 1992;16:239-42. [ Links ]
13. de Geer G, Webb WR, Sollito R, Golden J. MR characteristics of benign lymph node enlargement in sarcoidosis and Castleman´s disease. Eur J Radiol 1986; 6:145-8. [ Links ]
14. Germaine LM, Newhouse JH. Castleman´s disease. Clinical Imaging 2003; 27:431-4. [ Links ]











 texto en
texto en