Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Cirugía Oral y Maxilofacial
versión On-line ISSN 2173-9161versión impresa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.31 no.4 Madrid jul./ago. 2009
What would your diagnosis be?
¿Cuál es su diagnóstico?
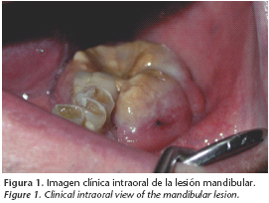
Male, 82 years old, non smoker being treated for hypertension and severe COPD, he has a history of in home oxygen therapy and cortical therapy. His dentist sent him to the emergency room at University Hospital of La Paz because of a tumor on the gum "mandibular edentia" the tumor has an ulcer-necrotic appearance and is 1 cm in diameter and 4 weeks progressed. During anamnesis the patient reports that his dentist treated him with antibiotherapy and anti-inflammatory, given the presumed diagnosis as a dental abscess, without improvement of the square (Fig. 1). The main symptoms are intense pain in the affected gum and subjacent mandible, and hypoesthesia in the area surrounding the left inferior dental nerve. It doesn't cause dysphagia or odynophagia.
Upon physical exploration there is no purulent material drained. Nor is there active bleeding even when pressure is applied to the lesion. There was no trismus, perceived upon ballooning palpation of the mandible cortical vestibular. There were no other lesions of adeonpathies felt in the oral cavity. In a radiological study the ortopantomography shows the osteolytic image of the edentulous sector of the third mandible quadrant which corresponds to teeth 35-37. The image extends to the 2/3 superiors and to the height of the mandible body (Fig. 2). The CT verifies the presence of an osteolytic mandible lesion with a vague pattern and cortical vestibular mandible affectation. It highlights the existence of a 2x1 cm lesion with a necrotic center in soft parts of the corresponding super adjacent gum (Fig. 3). A biopsy of the lesion is carried out with alveolar bone curettage. The anatomopatological and inmunohistochemistry analyses are informed about the lympho proliferative monoclonal cells type B and phenotype CD 20+, CD 79 a+. The serology is negative for HIV, cytomegalovirus, HBV, and HCV.
High level primary mandible non Hodgkin's lymphoma
Linfoma no-hodgkin de alto grado primario mandibular
L. Pingarrón Martín, J. Arias Gallo, E. Mirada, M.J. Morán, E. Palacios, M. Burgueño
Médico residente
Servicio de Cirugía Oral y Maxilofacial. Hospital Universitario La Paz. Madrid. España
The lymphomas are haematological tumors derived from the lymphatic and reticuloendothelial system. They are the most frequent malignant tumors in the head and neck, the only tumor that is more common is epidermoid carcinoma.
Traditionally classified as Hodgkin and Non-Hodgkin lymphoma (NHL), the Hodgkin disease fundamentally affects the mediastinal and cervical node while 40% of Non- Hodgkin's cases are classified as extra nodal diseases. 2-3% of this 40% start its primary form in the maxilla-mandible zone and in the oral cavity.1
The NHL contains a group of malignant diseases of the lymph reticular system characterized by clonal expansion of lymphocytes, mainly B cells and less commonly of the T cell line, at various levels of ontogenetic development.
The most prevalent subtype is NHL of large cells (up to 40-58% of all of the NHL, depending on the series reviewed)1-3 subtype corresponding to the clinical case that is presented. Oral NHL is usually made up of a component within a disseminated pathological process with implications of regional adenopathies. It does not usually appear as a primary extra nodal disease in the oral cavity or in maxillas. These last ones are from craniofacial bones that have the most frequent affectation of the bone lymphomas. Risk of NHL disease increases in patient with autoimmune disorders (for example Sjögren syndrome) being the predominant lymphoma origin of B cells.
One of the main problems in diagnosing NHL is its great variety of symptoms. Besides its principal nodular location, the rest of the organs, particularly those composed of lymphoid, can be affiliated with lymphoma development, enabling them to be primary and secondary tumors (in disseminated forms).
Immunohistological laboratory analysis and Southern blot are the main ways to diagnose and characterize NHL's. These forms provide critical information that guides clinicians in appropriate protocol and treatment.4
According to the majority of authors, in particular Urquhart et al. who provides a large series of cases totaling 235 NHL patients affected in the head and neck,5 there is no significant predominance in one sex, but other studies show a predominance of oral cavity NHL disease with a ratio of 3:2 men: women.4
In accordance with the case that we provide, all of the series in the literature revised agree that an intraoral tumor is a principle sign that these tumors are present and usually followed by signs of ulceration and radiographic bone destruction.1 While the series of 16 patients studied by Djavanmardi et al.2 pain is chosen as the principle symptom, equally as common, as the intra oral tumor. He documented ulceration in only 6.25% of cases and a predominant occurrence of oral NHL like dental hypoesthesia and dental mobility.
At the beginning these symptoms can lead to the dentist or doctor to falsely diagnosing the infectious dental pathology. The average age range at the time of diagnosis is very broad, although affectation tends to be more common in adults with a peak age between 40 and 70 years old.
Epson Barr Virus (EBV) is especially associated with Burkitt, allowing us to make a correlation between these lympho proliferative tumors and other viruses such as Hepatitis C, Herpes Virus Type 8 or HIV. This makes it necessary to dismiss positive serology for all patients who have oral lesions where there are suspicions of lymphoma.6
Diagnosis of NHL is mainly based on morphological, histological and cytological analysis which should be immunlologically confirmed.
Once the diagnosis is confirmed the classification is clinical and radiological.
The prognosis doesn't depend on the number of clinical discoveries but rather it depends on the histology and state of the tumor (if it is localized or disseminated, its state of development, the number of extra nodal localizations ) Age is also an important prognostic factor.
The position of the tumor doesn't appear to be a determining factor in prognosis. The Maxillas are an uncommon place and establishment (primary mandible NHL makes up 8% of mandible tumors and 0.6% of the total NHL) but the frequency increases when found in the Waldeyer ring (extra nodal localization in the head and neck is most frequent), ventilated cavities of solid facial (assume up to one third of extra nodal NHL's), salivary glands and oral mucosa (in order of decreasing frequency).
The prognosis of patients with lymphoma is, in general, better than in patient with epidermoid carcinoma. The survival rate after 5 years is 73% for those with Hodgkin's lymphoma and 65% for those with extra nodal non Hodgkin's in the head and neck.4
Based on the criteria of malignancy and the prognostic index, a strategic treatment is defined which includes radiotherapy (35-40 Gy) associated or un associated to different chemotherapy protocols (CHOP, cyclophosphamide, adriamicine, vincristine, prednisolone; ACVBP: adriamicina cyclophophamide, vindesine, bleomicin, prednisolone) This combination is mainly recommended for high level localized lymphomas.7
Once total remission of the tumor is accomplished, the objective of clinical follow-up is early detection of possible relapses. Patient follow-up should take place for 10 years including a clinical exam every 3 months during the first 5 years after remission, and in the absence of pathological discoveries, annual reviews should continue.
Discussion
Lymphoma is the second most frequent malignant pathology of the oral cavity.
NHL diagnosis is mainly based on morphological, histological, and cytological analysis and should be immunologically confirmed.
We should carry out a differential diagnosis mainly for squamous carcinoma cells, the most prevalent tumor in the head and neck region. A biopsy is necessary for this differential diagnosis. The biopsy should be wide enough to allow morphological, pathological and cultured studies as well as an immunohistochemistry analysis. It is important to emphasize that the superficial biopsy, with scarce tissue obtaining, can lead us to an erroneous diagnosis.
Classification of the tumor is clinical and radiological. A therapeutic strategy is chosen based on the state of the tumor.
In localized non Hodgkin's cases, radiotherapy has proved to be the most efficient treatment needing or not needing to associate chemotherapy on the basis of an aggressive tumor.
Surgery is only useful in lesion diagnosis and for excision of small tumors.
An exhaustive oral and cervical lymphatic ganglion exploration is fundamental in identifying lesions that could depict lymphoma. The possibility of this pathology should always considered by maxillofacial surgeons as a potential diagnosis.
![]() Correspondence:
Correspondence:
Dra. Lorena Pingarrón Martín
Servicio de Cirugía Oral y Maxilofacial
Hospital Universitario La Paz.
Pº de la Castellana, 261
28046 Madrid. España
References
1. Kemp S, Gallagher G, Kabani S, Noonan V, O´Hara C. Oral non-Hodgkin´s lymphoma: review of the literature and World Health Oraganization classification with referente to 40 cases. Oral Surg Oral Med Oral Path Oral Radiol Endod 2008;105:194-201. [ Links ]
2. Djavanmardi L, Oprean N, Alantar A. Malignant non-Hodgkin´s lymphoma (NHL) of the jaws: A review of 16 cases. J Craniomaxillofac Surg 2008;36:410-4. [ Links ]
3. Epstein JB, Epstein JD, Le ND, Gorsky M. Characteristics of oral and paraoral malignant lymphoma: a population-based review of 361 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:519- 25. [ Links ]
4. Nocini P, Lo Muziol, Fior A, Staibano S,Mignogna MD. Primary non-Hodgkin´s lymphoma of the jaws: inmunohistochemical and genetic review of 10 cases. J Oral Maxillofac Surg 2000;58:636-44. [ Links ]
5. Urquhart A, Berg R. Hodgkin´s and non-Hodgkin´s lymphoma of the head and neck. Laryngoscope 2001;111:1565-9. [ Links ]
6. Balasubramaniam R, Goradia A, Turner L.N, Stoopler E.T, Alawi F, Frank D.M, Greenberg M.S. Burkitt lymphoma of the oral cavity: an atypical presentation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:240-5. [ Links ]
7. Ugar D.A, Turner M, Memis L. Primary lymphoma of the mandibule: report of a case. J Oral Maxillofac Surg 1995; 53:827-9. [ Links ]











 texto en
texto en