INTRODUCTION
Dermoid cyst (DC) is a rare development derived injury, arising from epithelial rests resulting from the union of the first and second gill arches, and histologically it may be classified as true dermoid cyst, epidermoid cyst (EC), and teratoma1,2,3,4. When it occurs on the head and neck, it corresponds to up to 7 % of the cases1,2,4,5,6, and in only 1.6 % of the cases it appears in the oral cavity, and the floor of the mouth is the most affected area1,4,5,7. If compared to all oral cavity cysts, they account for less than 0.01 %3-7 of the cases.
EC is a benign lesion2. It presents non-pathognomonic clinical signs, basically involving an increase of volume4,6,7. They present slow, painless, and fluctuating growth masses5. The diagnostic of such lesions through clinical exams and conventional radiography is difficult1. It is necessary to correctly plan an intervention, with complimentary exams, such as ultrasound (US), computerized tomography (TC), magnetic resonance (RM), and a histopathological exam1,6. Fine needle aspiration cytology (FNAC) is a safe and economic alternative for the pre-surgery diagnostic of CE's; however, it is not possible to determine histological subtypes5. Differential diagnostic includes infectious processes, cyst in the thyroglossal duct, cystic hygromas, accumulation of adipose tissue, and neurofibroma and hemangioma6.
Treatment involves enucleation, and it may be performed intra- or extraorally, with low recurrence rates3,4,5. In addition to that, few cases have been reported in the literature, especially those affecting the tongue7. The tongue is a structure that is difficult to evaluate8,9. Thus, the purpose of the current work is to report a case of rare tongue injury diagnosed as an EC in an adult patient treated surgically.
CASE REPORTS
Case Report 1
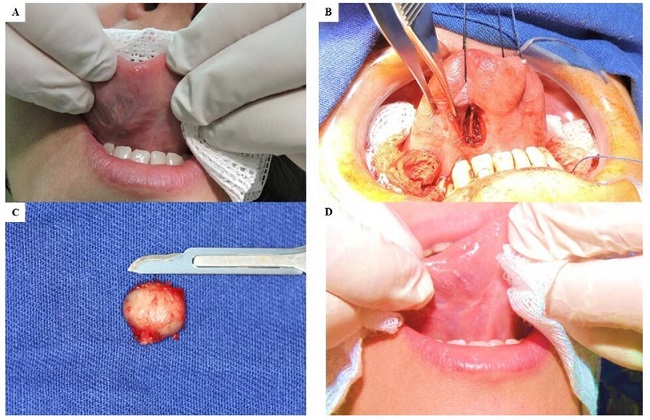
A 65-year old man came to the oral and maxilofacial surgery service of Uopeccan\Cascavel, complaining about a "little ball" on his tongue. A reddish nodular lesion on the left lateral edge of the tongue was clinically observed, hard to palpation, with a painful symptomatology that had been evolving for 90 days. As diagnostic hypotheses, a squamous cell carcinoma and a traumatic fibroma were suggested. After an incisional biopsy and a histopathological analysis, the result was a non-specific mild chronic inflammatory process, negative for malignity. It was then decided to perform a full surgical resection of the lesion, under general anesthesia and nasotracheal intubation. The incision was marked (Figure 1A), and an ellipse type incision was performed, approximately 5 x 2 cm long, running from the mucosa up to the upper longitudinal muscle of the tongue (Figure 1B). A dissection of the remaining tissues was performed and then the site was sutured using a Vicryl 3.0 thread, and closed through first intention (Figure 1C). The specimen was sent to histopathological analysis. The histological samples were stained using the hematoxylin and eosin technique (HE). The most relevant microscopic findings are shown below (Figure 2 A, B and C). The final diagnostic pointed to an epidermoid cyst. During the post-surgery period, the patient did not present any complication and at the 1-year follow-up exam did not make any complaint (Figure 1D). Patient gave informed consent.
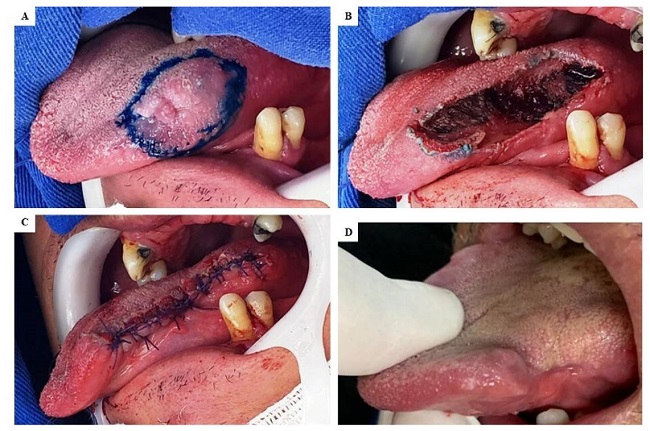
Figure 1. A: marking of the wedge type incision. B: remaining tongue tissue after the excision of the lesion. C: immediate post-surgery state. D: post-surgery state after 1 year.
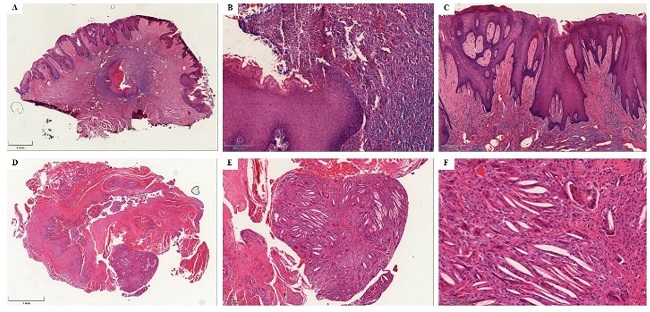
Figure 2. A: panoramic view (focus 8.7) of the central area with partially torn and sore epithelial cyst. B: greater detail (focus 28.5) of the epithelial inclusion cyst, with the cyst transition area and a torn and sore area. C: detail (focus 38.8) of the cyst surface epithelium, with irregular acanthosis. D: panoramic view (focus 26.5), with a fibrous tissue that comprises muscle fibers and pseudocystic spaces in the center, while in the periphery there is a foreign body type granuloma with cholesterol crevices. E: greater detail (focus 75) of the area with a foreign body type granuloma. F: greater detail (focus 249) of the area with a foreign body type granuloma. There are giant foreign body type cells and cholesterol crevices.
Case Report 2
A 40-year old woman came to the oral and maxilofacial surgery service of Uopeccan\Cascavel, complaining about a "little ball" on her tongue that had been evolving for 3 months. The clinical exam pointed to a painless increase of volume in the belly of tongue and soft to palpation (Figure 3 A). The patient was submitted to a FNAP (Fine Needle Aspiration Puncture) during which a yellowish liquid was found compatible with the cystic lesion. The liquid was sent to a histopathological exam, which resulted in a cystic content. The patient was submitted to cystic enucleation under general anesthesia (Figure 3 B). The specimen was sent to histopathological analysis (Figure 3 C). The histological samples were stained using the hematoxylin and eosin technique (HE). The most relevant microscopic findings are shown below (Figure 2 D, E and F), and an Epidermoid Cyst was diagnosed. The patient has been under a 3-year follow-up regime, without any complaint (Figure 3 D). Patient gave informed consent.
DISCUSSION
EC is a rare injury in the oral cavity7,10, and it is even much rarer in the tongue2,7,10. Ueno et al. (2018) performed a literature review with the published cases of EC in the tongue and found just 12 cases of EC, plus the case they were reporting. We have observed that, after that publication, there has been another report of this lesion and its location, by Jain (2019). Thus, the current cases have become the 14th and 15th cases of EC in the tongue found in the literature, thus confirming the relevance of the current work.
Since it involves a lesion without specific characteristics, the diagnostic of this lesion depends on histopathological analysis and may be supported by US in order to determine its location, extension, and relationship with the adjacent structures7. In the current case, the patient was submitted to an incisional biopsy and presented a histopathological condition involving a mild non-specific chronic inflammatory process, negative for malignity, and was then submitted to a full resection of the lesion, with a final result of the histopathological analysis indicating an EC in the tongue.
This pathology might affect children and adults, and in the study undertaken by Ueno et al. (2018) and Jain (2019), these authors found a higher prevalence of occurrences in children, with 9 cases out of the 13 studied ones. The highest manifestation in children might be related to the congenital etiological theory, according to which the surface ectoderm fails to separate from the subjacent neural tube, or from the surface ectoderm invagination along the embryological fusion sites during the embryonic stage1,2,5,10. Our patient is an exception, considering that he was a 65-year old adult. The age of the patient has also led us to correlate the etiology of his lesion as possibly being a trauma, pointing to the acquired type theory, which is related to traumas5,7,10. However, there is no clinical or histopathological difference between both types10.
Treatment is based on surgical excision3,4. It is important to perform it, since the growth of the lesion might lead to an obstruction of air passages2, making it difficult to breath2,6,7, including dysphonia, dysphagia, dysarthria, with interference on chewing, moving the tongue, and speech4,5,6,7. And 5 % of the lesions might become malign lesions1,3,4. Thus, the indication to fully remove it was rather correct, since the lesion had been growing and thus causing increasing distress to the patient, which might evolve into the above mentioned consequences.
CONCLUSION
Epidermoid cyst in the oral cavity is a rare disease, which may clinically manifest itself in many different forms. Although image exams help to diagnose it, incisional biopsy and/or FNAP are highly valuable to ensure a definitive diagnostic. The standard golden treatment is a full surgical resection of the lesion. In the current cases, the lesion occurred in an uncommon age group, and was treated surgically.