Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Anales del Sistema Sanitario de Navarra
versión impresa ISSN 1137-6627
Anales Sis San Navarra vol.36 no.2 Pamplona may./ago. 2013
https://dx.doi.org/10.4321/S1137-66272013000200020
Heyde syndrome in a 71-year-old man who underwent chest radiotherapy at young age
Síndrome de Heyde en un hombre de 71 años que había recibido radioterapia en el pecho de joven
V.M. Santos1, L.A.M. Santos2, A.A.D. Modesto3, M.O. Amui4
1. Catholic University and Medicine Department from Armed Forces Hospital (HFA). Brazília-DF. Brazil
2. Surgery Department from State Workes Hospital (HSE). Sao Paulo-SP. Brazil
3. Family and Community Medicine. Sao Paulo-SP. Brazil
4. Internal Medicine. Uberaba-MG. Brazil
Dirección para correspondencia
ABSTRACT
We report the case of a 71-year-old man with diagnosis of aortic valve stenosis for ten years, who came to hospital because of breathlessness during the previous two months and recent low intestinal hemorrhage. On admission, laboratory tests and upper gastrointestinal endoscopy and colonoscopy revealed anemia and bleeding cecal angiodysplasia. The echocardiography study showed a severe aortic stenosis. Classical Heyde syndrome is described as the association of aortic stenosis, bleeding gastrointestinal angiodysplasia and secondary anemia. The antecedent of mediastinal radiotherapy for treatment of Hodgkin´s disease during his youth, and eventual late cardiac adverse effects that may include aortic or mitral valve disturbances are highlighted. Electrocoagulation with argonium was performed on the sites of active bleeding during the colonoscopy. In sequence, surgical replacement by bioprothesis was done on the aortic valve. The patient remains asymptomatic, under long-term outpatient surveillance, with normal control evaluations. The aim of this case study is to emphasize difficulties related to diagnosis, and to highlight the role of endoscopy and imaging studies to confirm a hypothesis of this underestimated condition.
Key words: Angiodysplasia, Aortic valve stenosis. Colon bleeding. Heyde syndrome. Mediastinal radiotherapy.
RESUMEN
Se presenta el caso de un varón de 71 años con estenosis aórtica diagnosticada diez años antes, que acude al hospital por disnea durante dos meses y reciente hemorragia digestiva baja. La analítica y la endoscopia oral y colonoscopia realizadas en el momento de la admisión revelaron anemia y angiodisplasia cecal con sangrado activo. El ecocardiograma mostró estenosis aórtica severa. El síndrome de Heyde clásico está descrito como asociación entre estenosis aórtica y sangrado por angiodisplasia gastrointestinal, con anemia secundaria. Se destaca el antecedente de radioterapia mediastinal para tratamiento de enfermedad de Hodgkin durante su juventud, y eventuales efectos adversos tardíos que pueden incluir trastornos de las válvulas aórtica y mitral. Durante la colonoscopia se realizó la electrocoagulación con argón del punto de sangrado activo. Posteriormente se realizó cirugía de sustitución valvular aórtica utilizando una bioprótesis. El paciente permanece asintomático, realizando un seguimiento ambulatorio a largo plazo, y con exámenes de control normales. El objetivo de este estudio es enfatizar las dificultades relacionadas al diagnóstico, y resaltar el papel de los estudios endoscópicos y de imágenes para confirmar una hipótesis de esta entidad subestimada.
Palabras clave: Angiodisplasia. Estenosis aórtica. Hemorragia digestiva baja. Síndrome de Heyde. Radioterapia mediastinal.
Introduction
Heyde syndrome is a challenging condition first described by Heyde in 1958, which consisted of aortic valve stenosis, bleeding of gastrointestinal angiodysplasia and iron deficiency anemia1-3. A secondary shear stress-enhanced proteolysis of high molecular weight multimers of von Willebrand factor during the blood flux through a severe aortic stenosis also play a role1-6. Although angiodysplasia and degenerative aortic stenosis often occur in elderly people, the association between these entities in patients with Heyde syndrome was found significant1,3 Moreover, valve replacement avoids recurrence of bleedings from angiodysplastic vessels2-6. Additional factors include cholesterol emboli from the stenotic aortic valve, sympathetic-mediated vasodilation secondary to hypoxia and atherosclerotic changes in mesenteric vessels1,3. Better awareness about this syndrome could contribute to early diagnosis and therapeutic decisions for management of patients with aortic valve stenosis and recurrent intestinal bleeding. This case study aims to increase the suspicious index about Heyde syndrome that is a challenging condition with not well-understood etiopathogenesis, involving multidisciplinary approaches.
Case report
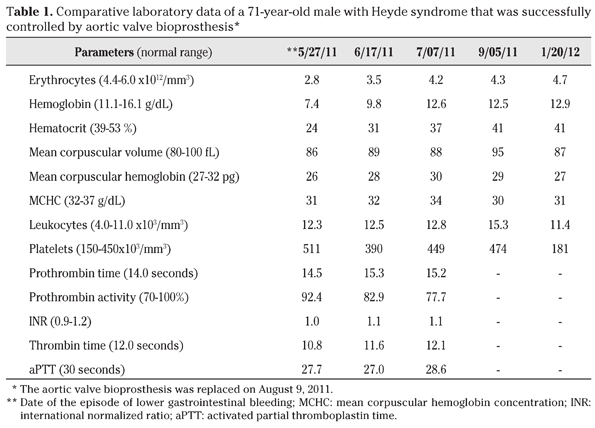
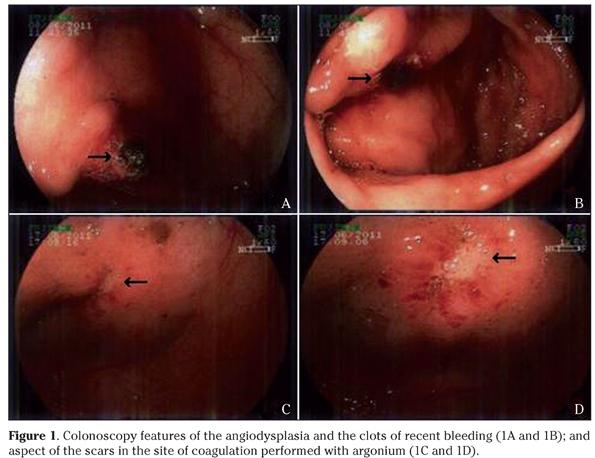
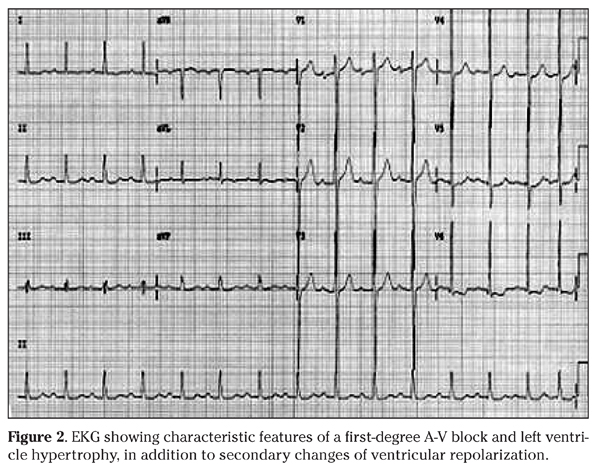
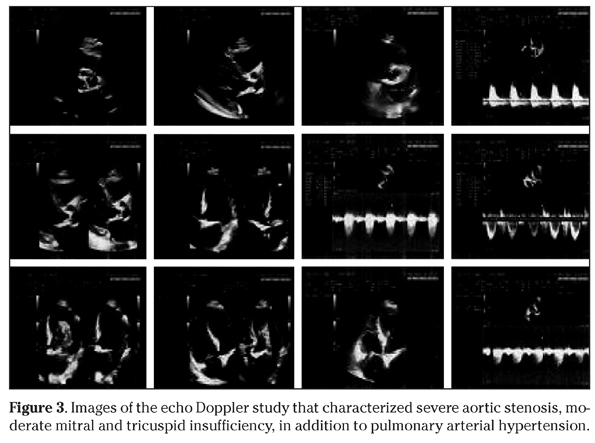
A 71-year-old man, with diagnosis of arterial hypertension and aortic valve stenosis for nearly ten years, claimed progressive breathlessness for the last two months, and rectal loss of bright blood. He was taking amlodipine, captopril, furosemide and enteric-coated aspirin. There was a history of chemotherapy and several courses of mediastinal radiotherapy to treat Hodgkin´s lymphoma when he was a young man. He denied antecedent of pharyngotonsilites, rheumathic diseases or hemorrhagic disorders. On physical examination he was pale, with an aortic systolic murmur (3+) and a mitral diastolic murmur (2+); heart rhythm was regular with 70 bpm, and his blood pressure was 110/80 mmHg. Hematology data (Table 1) showed severe anemia, which was treated with a blood transfusion, in addition to iron supplementation. The lipidogram showed total cholesterol: 122 mg/dL, HDL-cholesterol: 34 mg/dL, LDL-cholesterol: 86 mg/dL, and triglycerides: 108 mg/dL. The results of other laboratory exams were unremarkable, including coagulation factors, tumor markers, hepatic and renal functions, as well as serologic tests. Upper digestive endoscopy was normal, but the colonoscopy study detected cecal angiodysplasia with signs of recent bleeding (Figs. 1A and 1B), and local hemostasy was performed by coagulation with argonium (Figs. 1C and 1D). Following his clinical management, he showed a gradual and slowly progressive improvement. The EKG revealed left ventricle (LV) hypertrophy and ST segment elevation (Fig. 2); while the heart catheterization study did not detect significant coronary artery obstructions. The images of cardiac echo Doppler study (Fig. 3) showed: a) mild left atrial (LA) dilation, moderate LV hypertrophy, calcifications in the mitral ring and in the mitro-aortic junction; b) maximum diastolic LA-LV gradient of 21 mmHg with a mean value of 12 mmHg, in addition to a discrete mitral valve insufficiency; c) trivalvular aortic valve with fibro calcifications, and commissural fusion; d) maximum diastolic LV-aorta gradient of 94 mmHg with a mean value of 58 mmHg and a valve area of 0.5 cm2, and a relation between the aortic subvalvar and the valvar velocity of 0.17; e) moderate tricuspid insufficiency; f) normal pulmonary valve; and g) and estimated systolic pulmonary artery pressure of 68 mmHg. Association of severe aortic valve stenosis with bleeding from cecal angiodysplasia was consistent with the diagnosis of Heyde syndrome in this patient, and replacement of the abnormal valve by bioprothesis was successfully performed, soon after correction of the blood parameters. The patient did not have new intestinal bleedings, and Table 1 shows the improved blood tests.
Discussion
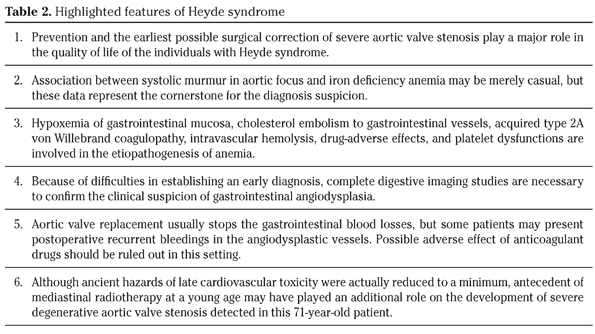
A bleeding tendency found in Heyde syndrome was associated with the acquired type 2A von Willebrand disease3. Enlarged and fragile angiodysplastic vessels are more often found in the mucosa and submucosa of colon, stomach, small intestine, and nose, where recurrent episodes of bleeding may occur3. Batur et al found aortic stenosis in about 32% of patients with gastrointestinal arteriovenous malformations, while this valve change was detected in only 14% of the control population1. Coexistent aortic stenosis has been described in 7-29% of patients with gastrointestinal angiodysplasia, and gastrointestinal bleedings may occur in 3% of those with severe stenosis3,6. Furthermore, in the majority of patients with Heyde syndrome, the aortic valve replacement can prevent future recurrences of bleeding episodes of the gastrointestinal angiodysplastic vessels1-12. The degree of anemia secondary to intestinal blood losses is a major concern that should be clinically and endoscopically managed before the valve replacement1. Preoperative hemolysis associated with the turbulence and shear stress produced by flow through the stenosed valve constitutes an important factor related to the mechanism of anemia13. Moreover, the aortic valve replacement by bioprothesis contributes to control the occurrence of microangiopathic hemolysis. Mainstay of Heyde syndrome is aortic valve stenosis and bleeding angiodysplasia, but acquired von Willebrand coagulopathy type 2A (vWS-2A) was further considered part of the syndrome3,12. This coagulopathy has multivariate origin3, and cardiovascular causes yield 12% of the cases3,6. The heaviest multimers of von Willebrand factor (vWF) are needed to stop angiodysplasic bleedings, because they can mediate the platelet aggregation on the sites of vascular damage2,3,5,6. Plasma proteases, activated in sites of turbulent blood flow, can clear these multimers2,3,12. Unremarkable results of preoperative coagulation investigations constituted our initial concern; however, hematological abnormalities are related to severity and may lack in 8-33% of cases3,8,12. Moreover, some case studies about Heyde syndrome have been published without confirmation by the gold standard gel electrophoresis that the heaviest vWF multimers were decreased2,5,12,14. This may be due to unavailability of the required high cost assays in developing regions, and vWS-2A coagulopathy may be absent in patients with aortic gradients below 50 mmHg6,12. Additional concern in the management of this group of patients is about the use of medicines that can enhance the hemorrhagic tendency, like aspirin, clopidogrel, ticlopidine, and warfarin3,10. Avoiding unnecessary colectomy after valve replacement, one must distinguish adverse-effects of these drugs from recurrent bleeding of angiodysplasia. The main features of Heyde syndrome, in addition to a possible relationship with chest radiation in the present case are showed in Table 2. This 71-year-old patient with clinical diagnosis of Heyde syndrome underwent mediastinal radiotherapy to treat a Hodgkin´s lymphoma nearly 40 years earlier. Cardiovascular injuries induced by radiation are the second main cause of late mortality in survivors of Hodgkin´s lymphoma submitted to mediastinal radiotherapy15. Survival patients with lymphoma treated by mediastinal radiation at a young age may develop asymptomatic or symptomatic effects, which include accelerated coronary disease, aortic calcification, myocardial fibrosis, pericarditis, and aortic or mitral valve dysfunction15-19. Mechanisms of these abnormalities are not elucidated, and the changes usually evolve for very long periods of time after mediastinal radiotherapy15-19. Aortic and/or mitral replacement may be required to correct the late effect of radiation-associated valvular disease, which can be characterized from 5 to 30 years after the radiotherapy15,17-19. Although degenerative calcified changes are often found in elderly people, and result in variable aortic valve dysfunction, an additional role of mediastinal radiation was not ruled out in this case. Technological advances in radiotherapy, developed in the last two decades, have contributed to increase the tumor control without provoking further toxicity. These improvements include three-dimensional conformal radiotherapy, intensity modulated radiotherapy for maximum conformation, and high precision in radiation delivery and better preservation of healthy tissue20. Therefore, ancient hazards of late cardiovascular toxicity were actually reduced to a minimum.
References
1. Batur P, Stewart WJ, Isaacson JH. Increased prevalence of aortic stenosis in patients with arteriovenous malformations of the gastrointestinal tract in Heyde syndrome. Arch Intern Med 2003; 163: 1821-1824. [ Links ]
2. García-Martín A, Moreno A, Moro C. Heyde´s syndrome. Rev Esp Cardiol 2011; 64: 75-83. [ Links ]
3. Gola W, Lelonek M. Clinical implication of gastrointestinal bleeding in degenerative aortic stenosis: An update. Cardiol J 2010; 17: 330-334. [ Links ]
4. D´souza PM, Blostein MD. Diagnosis of Heyde´s syndrome by abnormal closure times despite normal von Willebrand´s activity. Blood Coagul Fibrinolysis 2011; 22: 622-623. [ Links ]
5. Gül M, Sürgit O, Ozal E, Ormeci A, Bakir I. Treatment of aortic valve stenosis and gastrointestinal bleeding by transcatheter aortic valve implantation in Heyde syndrome. Anatolian J Cardiol 2012; 12. doi:10.5152/akd.2012.224. [ Links ]
6. Mishra N, Moda P, Khanna A. Heyde´s syndrome: an unusual cause of lower gastrointestinal bleeding. Ann Nigerian Med 2012; 6: 54-55. [ Links ]
7. Granel B, Serratrice J, Bernit E, Chaudier B, Habib G, Mesana T, et al. Heyde syndrome. Presse Med 2002; 31: 1451-1453. [ Links ]
8. Massyn MW, Khan SA. Heyde syndrome: a common diagnosis in older patients with severe aortic stenosis. Age Ageing 2009; 38: 267-270; discussion 251. [ Links ]
9. Morishima A, Marui A, Shimamoto T, Saji Y, Tambara K, Nishina T, et al. Successful aortic valve replacement for Heyde syndrome with confirmed hematologic recovery. Ann Thorac Surg 2007; 83: 287-288. [ Links ]
10. Natowitz L, Defraigne JO, Limet R. Association of aortic stenosis and gastrointestinal bleeding (Heyde´s syndrome). Report of two cases. Acta Chir Belg 1993; 93: 31-33. [ Links ]
11. Scheffer SM, Leatherman LL. Resolution of Heyde´s syndrome of aortic stenosis and gastrointestinal bleeding after aortic valve replacement. Ann Thorac Surg 1986; 42: 477-480. [ Links ]
12. Vaz A, Correia A, Martins B, Capelo J, Ferreira P, Henriques P, et al. Heyde syndrome - the link between aortic stenosis and gastrointestinal bleeding. Rev Port Cardiol 2010; 29: 309-314. [ Links ]
13. Kawase I, Matsuo T, Sasayama K, Suzuki H, Nishikawa H. Hemolytic anemia with aortic stenosis resolved by urgent aortic valve replacement. Ann Thorac Surg 2008; 86: 645-646. [ Links ]
14. Figuinha FCR, Spina GS, Tarasoutchi F. Síndrome de Heyde: relato de caso e revisão da literatura. Arq Bras Cardiol 2011; 96: 42-45. [ Links ]
15. Poulin F, Semionov A, Roméo P, Demers P, Pressacco J, Basmadjian A. Extensive radiation-induced heart disease in an adult patient treated for lymphoma as a child. Can J Cardiol 2011; 27: 390.e1-4. [ Links ]
16. Apter S, Shemesh J, Raanani P, Portnoy O, Thaler M, Zissin R, et al. Cardiovascular calcifications after radiation therapy for Hodgkin lymphoma: computed tomography detection and clinical correlation. Coron Artery Dis 2006; 17: 145-151. [ Links ]
17. Carlson RG, Mayfield WR, Normann S, Alexander JA. Radiation-associated valvular disease. Chest 1991; 99: 538-545. [ Links ]
18. Daitoku K, Fukui K, Ichinoseki I, Munakata M, Takahashi D, Fukuda I. Radiotherapy-induced aortic valve disease associated with porcelain aorta. Jpn J Thorac Cardiovasc Surg 2004; 52: 349-352. [ Links ]
19. Tamura A, Takahara Y, Mogi K, Katsumata M. Radiation-induced valvular disease is the logical consequence of irradiation. Gen Thorac Cardiovasc Surg 2007; 55: 53-56. [ Links ]
20. Domínguez MA, Rico M, Vila MT. Role of radiotherapy in the XXI century. An Sist Sanit Navar 2009; 32 (Suppl 2): 5-12. [ Links ]
![]() Dirección para correspondencia:
Dirección para correspondencia:
Vitorino Modesto dos Santos
Armed Forces Hospital
Estrada do Contorno do Bosque, sn
Cruzeiro Novo 70658-900 Brazília-DF
Brazil
E-mail. vitorinomodestos@gmail.com
Recepción: 16 de noviembre de 2012
Aceptación provisional: 12 de diciembre de 2012
Aceptación definitiva: 17 de diciembre de 2012