Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.13 no.35 Murcia jul. 2014
ENFERMERÍA Y PERSPECTIVA DE GÉNERO
Factors affecting the performance of a selective episiotomy in nulliparous women
Factores que influyen en la realización de una episiotomía selectiva en mujeres nulíparas
Hernández Pérez, Javier*; Azón López, Esther**; Mir Ramos, Eduardo***; Peinado Berzosa, Ruth****; Val Lechuz, Belén***** and Mérida Donoso, Ángel******
* Nurse. Specialist in Gynecology and Obstetrics at Hospital Universitario Miguel Servet . Zaragoza. Email: javi22perez@yahoo.es
** Nurse at the Healthcare Centre of Villarrolla de la Sierra (Zaragoza) Specialist in Gynecology and Obstetrics.
*** Nurse at the Emergency Service 061 in the Autonomous Community of Aragon. UME (Medical Emergency Unit) of Alcañiz (Teruel).
**** Nurse of Continuous Care in Sector III of Zaragoza. Specialist in Gynecology and Obstetrics.
***** Nurse. Specialist in Gynacology and Obstetrics at the Healthcare Centre of Delicias Sur. Zaragoza.
******Nurse at Hospital Universitario Miguel Servet. Zaragoza.
ABSTRACT
Objective: To determinate factors affecting the performance of a selective episiotomy in nulliparous women.
Methods: A descriptive cross-sectional study was conducted at the Miguel Servet University Hospital (HUMS) of Zaragoza within a sample of 568 nulliparous women. The performance of episiotomy was compared to postpartum variables such as: maternal age, nationality, gestational age, fetal weight, time of birth, fetal sex, analgesia used and professional attending the birth, as well as the existence of tears and pH results fetal umbilical cord artery.
Results: The rate of episiotomy in nulliparous women at HUMS of Zaragoza is 62%. Factors influencing the performance of an episiotomy are greater fetal weight (p=0,000), as well as individual professional judgment attending childbirth.
Other factors such as gestational age, fetal sex, epidural analgesia, time of birth or nationality do not affect the above mentioned performance.
Lack of episiotomy increases first degree perineal tears and, to a lesser extent, the second degree, without causing an increased risk for fetal wellbeing. In addition, it allows the possibility of maintaining the full perineum after birth, mainly among younger women.
Conclusions: It would be advisable to revise the protocols of selective policy for episiotomy rate decrease and equalize rates between different professionals.
Key words: Selective episiotomy; routine episiotomy; perineal tear; restrictive episiotomy.
RESUMEN
Objetivo: Determinar los factores que influyen en la realización de una episiotomía selectiva en mujeres nulíparas.
Material y método: Se realizó un estudio descriptivo transversal en el Hospital Universitario Miguel Servet (HUMS) de Zaragoza con una muestra de 568 mujeres nulíparas. Se comparó la existencia o no de episiotomía tras el parto con las variables: edad materna, nacionalidad, edad gestacional, peso fetal, hora de nacimiento, sexo fetal, analgesia empleada y profesional que asiste el parto, así como la existencia de desgarros y los resultados del pH de la arteria umbilical fetal.
Resultados: La tasa de episiotomía en las mujeres nulíparas en el HUMS de Zaragoza es de un 62%. Entre los factores que influyen en la realización de una episiotomía se encuentran el mayor peso del feto (p =0,000), así como el criterio individual del profesional que asiste el parto. Otros factores como la edad gestacional, el sexo fetal, la analgesia epidural, la hora de nacimiento o la nacionalidad no influyen en su realización. El no hacer episiotomía incrementa los desgarros perineales de primer grado, y en menor medida los de segundo, sin que ocasione un mayor riesgo para el bienestar fetal. Además, su no realización permite la posibilidad de mantener el periné íntegro tras el parto, principalmente entre las mujeres más jóvenes.
Conclusión: Sería recomendable revisar los protocolos de política selectiva de episiotomía para conseguir disminuir su tasa e igualar los porcentajes existentes entre los diferentes profesionales.
Palabras clave: Episiotomía selectiva; episiotomía rutinaria; desgarro perineal; episiotomía restrictiva.
Introduction
The episiotomy is an incision made in the perineum to enlarge the vaginal opening It was clinically introduced in the 18th Century(1,2), but it was not routinely employed until de first half of the 20th. The cause of its use was based on the reduction of the risk of perineal tears, pelvic floor dysfunction, and urinary and faecal incontinence(2). Despite the limited data about its use, it became a regular proceeding, underestimating the potential adverse effects(2).
Recent research advice the use of the selective episiotomy against the routine because its restrictive use presents a lower rate of maternal morbidity derived from a minor perineal trauma. Its restrictive use causes a minor risk of subsequent perineal trauma, a minor need of suture of its perinea trauma and less complications related to the cicatrisation within seven days(1,6). However, the restrictive policy causes an increase of first and second grade tears(7), mainly located in the anterior perineum(1,8), but not an increase on those of third and fourth grade(6,8,9).
About the fetal morbility, no association has been found between the use of selective episiotomy and the bad perinatal results(5,7), such as the 5-minutes apgar of less than 7(10-12).
The Strategy for Childbirth proposed by the Spanish Ministry of Health and Consumption (Estrategia de Atención al Parto Normal del Ministerio de Sanidad y Consumo), recommends to avoid the routine episiotomy in spontaneous vaginal delivery(13), limiting its used to instrumental delivery (except those in need of vacuum assistance) and in cases of confirmed fetal distress. The objective of this recommendation is to achieve episiotomy rates lower than 10%(14). In spite of the wide evidence about the benefits of the selective episiotomy, it is still being employed in a high percentage of deliveries and without following a common criterion(13). For instance, in Colombian hospitals, the episiotomy rate varies from 51-61% among nulliparous women(8). In Brazil, the rate is 29.1%(10), while it reaches 63.3% in South Africa and 100% in Guatemala(15). In Spain the percentage varies from 33% to 73%, depending on the Autonomous Community(13). According to a research published in 2006, the episiotomy rate is 50.48%(16) . However, this rate seems to be falling in our country, with a reduction of 20% between 2001 and 2006(3). This fact coincides with other European countries, such as France, where, after implementing the restrictive episiotomy policies, the rate has fallen from 55.7% to 13.3%(17). According to a research published in 2005(9), after the implementation of the restrictive policies at the Miguel Servet Hospital (Zaragoza, Spain), the episiotomy rates varied from 83.7% to 59%.
Among the variables related to the realization of episiotomy, we can find the age, the nulliparity and the maternal pathology (hypertensive syndrome and gestational diabetes)(10). About the age, the performance of episiotomy is more common among the teenagers, while it decreases from 35 year-old-women(10). The maternal pathology(10) and the nulliparity(7,10,11,15) are associated to an increase on the prevalence of the episiotomy.
Other variables such as the gestational age or the newborn's weight did not present any relation to the performance or non performance of the episiotomy(7,10,11).
Other factors, such as the fetal gender, the type of anaesthesia, the nationality or the professional attending the delivery, have been studied in a lower extent. Therefore, the authors believe this research to be necessary, because it would provide more information to consolidate the use of the selective episiotomy among the health professionals.
Objectives
-Analyze whether any association among the variables exists: maternal age and nationality, gestational age, gender and fetal weight, time of birth, professional attending the delivery, type of anaesthesia used with or without episiotomy.
-Determine whether the realization of the episiotomy influences the fetal pH, the appearance of perineal tears and its grade.
Materials and methodology
Design
Cross sectional study about the episiotomy performance employed at the HUMS through the revision of the registry book kept in the delivery room.
Scope
Childbirth Unit of HUMS; level III hospital whose maternity unit assists areas 2 and 5 of the healthcare map in the Autonomous Community of Aragón (Spain).
Period of study
From September 2012 to February 2013, both included.
Population Sample
Every nulliparous woman who had a full-term pregnancy, unique alive fetus with cephalic presentation, whose delivery was either spontaneous or induced, attended at the HUMS within the above specified period was included in the research.
Therefore, primiparae or multiparae were excluded. Out-of-hospital deliveries, toco-surgical proceedings (through forceps, vacuum, or caesarean births), multiple pregnancies, preterm babies or dead fetus were excluded. Those cases where the gestational age was unknown at the moment of delivery and those where the woman had had genital mutilation were also excluded.
Sample size determination
Study criteria for inclusion were fulfilled by a total of 568 women. The authors decided not to practice any sampling because it was considered imperative to analyze the information of every individual.
Data collection
A template was employed to collect socio-demografic, obstetric, and newborn data. These data were obtained from the registry book kept at the delivery room of the HUMS, referring to above mentioned period-September 2012 to February 2013.
Research variables
Main dependent variable:
Episiotomy performance: YES/NO.
Secondary dependent variables:
Ph of the umbilical artery. The pH of the umbilical artery was measured after the birth. The values were classified as follows(18)
> o = 7.10 (normal value)
7.0-7.09 (acidosis)
< 7.00 (pathological fetal acidosis)
Perineal tear. Were classified into: no tear/ 1st grade / 2nd grade / 3rd grade / 4th grade.
Independent variables:
Maternal age. Was collected quantitatively, expressed in years. Besides, it was grouped qualitatively, as follows: <15 years/ 15-19 / 20-24 / 25-29 / 30-34 / 35-39 / 40-44 / >45 years.
Gestational age. Was collected quantitatively, expressed in years. It was collected also qualitatively, grouping as follows: 37-37,6 / 38-38,6 / 39-39,6 / 40-40,6 / 41-41,6, >42.
Maternal nationality. In order to achieve a larger sample, the nationalities were grouped as follows: West Europe / East Europe / South America / North America / Asia / Australia / Africa Sub-Sahara / Africa Maghreb.
Time of birth. Expressed in hours and minutes.
Fetal gender: Male / Female.
Fetal weight. The newborn weight was collected during the first hour of life, expressed in grams. As qualitative variable, was grouped as follows: <1500 /1500-1999 / 2000-2499/ 2500-2999/ 3000-3499 / 3500-3999 / 4000-4499 / >4500 grams.
Type of anaesthesia: None / epidural / intradural / combined / local.
Category of the professional attending the delivery: Gynaecologist / Midwife / Midwife resident / Resident of gynaecology.
Category of the professional attending the delivery: Each professional was registered by a different number.
Data analysis
Data collected using the software Microsoft Office Excel 2007© were imported to a matriz with the format of the software Statistical Package for the Social Sciences© (SPSS), on its 15.0 version.
In the non-variable analysis-qualitative variables-the numerical analysis was performed by frequency tables, while the graphic analysis which complements it was elaborated using either pie charts or bar charts. About the quantitative variables-the numerical analysis-different measures of summary were employed and frequency tables in those cases where the variable had few different values. The graphic analysis was performed by means of histograms or box charts. In the bivariate analysis, if both variables were qualitative, the corresponding contingency table was elaborated, together with the χ2 (Chi-squared) test, complementing the information with grouped bar charts. When one of the variables was quantitative and the other qualitative, the averages were compared by means of box charts or error bars.
Ethical considerations
The Unidad de Calidad Asistencial (Asistential Quality Unit) of the HUMS, the Direcciones de Enfermería y Médica (Nursery and Medical Directions) of the hospital and the Ethics Comitee of the Centre (Comité de Ética del Centro), were informed about the conduction of this research and consent it. No ethical conflict was identified.
Results
During the study period, 2035 deliveries were registered at the HUMS. From them, 1075 corresponded to nulliparous women (52.83%), and 568 women (27.91%) fulfilled the criteria for inclusion within the research.
The average age of the sample was 30.6 years. The most frequent nationality was Spanish (76.4%).
Episiotomy was performed on 62% of women included in the research. Concerning the assessment of the perineal tears after delivery, 68.8% of the cases did not present any tear. Within the different grades of tears, the first was the most common (32.2%).
Concerning the fetus, male sex was predominant (51.1%) over female. The average birth weight was 3237 grams, and the average gestational age, 40 weeks. As a neonatal result, the pH of the umbilical artery was determined, obtaining an average value of 7.26.
Concerning the professional attending the delivery, it should be highlighted that on 56.3% of the cases, it was the midwife who intervened, followed by the midwife residents (25.7%), residents of gynaecology (14.4%) and gynaecologists (3.5%).
Comparing different variables collected by the performance of episiotomy, the following results were obtained:
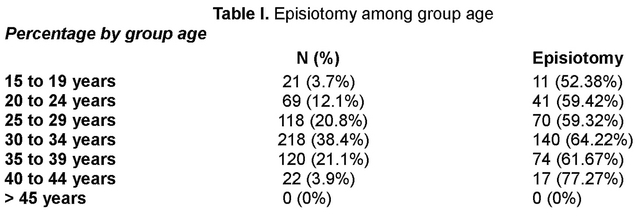
Maternal Age / Performance of episiotomy
An increase on the episiotomy percentages was observed as the maternal age increased, rising from 52.38% in the 15-19 years group to 77.27% from 40 years on. Nevertheless, comparing the maternal age in both groups (episiotomy or not) no significant relation was found between both variables (p = 0.208).
Fetal weight / Performance of episiotomy
Analyzing both variables it was confirmed that in those cases where the episiotomy was performed, the average fetal weight was 3284.7 grams; when it was not performed, the average was 3162.0 grams (a difference of 122.7 grams). This difference, even small, was statistically significant (p = 0.000).
Category of the professional attending the delivery / Performance of episiotomy
Analyzing the percentages of episiotomy for each professional category, it was confirmed that the gynaecology residents had the highest rates (74.4%), followed by the midwife residents (59.6%), and midwifes (60.6%). Gynaecologist rate was 50%. When performing the Chi-squared test, a statistical value of 7.180 and a significance of 0.066 were obtained.
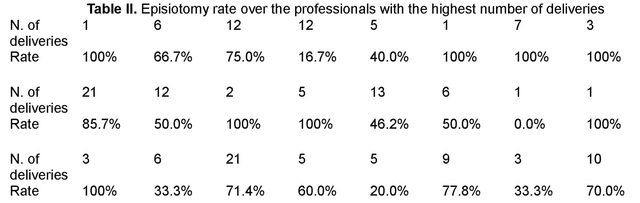
Professional episiotomy rate
The individual episiotomy rate determined was over 91 professionals. Analyzing the results, there is no existence of uniformity between the individual rates of episiotomy.
Other variables / Performance of episiotomy
No significant statistical relation was found among the variables: maternal nationality (Chi-squared=3.735 and p=0.588), fetal gender (Chi-squared=0.548 and p=0.490), gestational age (p= 0.204), time of birth (Chi-squared=11.746 and p=0.383), and type of anaesthesia (Chi-squared=5.649 and p=0.130) with the performance or non performance of episiotomy.
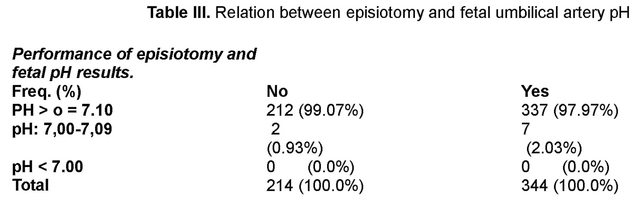
Performance of episiotomy and fetal pH result
Performing the statistical analysis of both variables, a Chi-squared of 1.007 and a significance of 0.494 were obtained.
In both groups (episiotomy or not) the fetal pH results found were normal (pH larger or equal to 7.10). No pathological fetal acidosis was found in any case.
Perineal tears / Performance of episiotomy
In our research, it was observed that the percentage of perineal tears was lower within the episiotomy group (6.5%) than in the non-episiotomy group (71.3%), association which was found statistically significant (Chi-squared:261.721; p=0.000).
Taking the tear grade into account, it was observed that:
-The episiotomy group presented lower percentages of first and second tears (3.4% and 2.8% respectively), compared to the no episiotomy group.
-There was a significant rise of the first grade tears (55.6%) against the second grade (15.7%) within the no episiotomy group.
-The rate of third grade perineal tears was 0.3% in those women who had episiotomy done, but it did not happen within the no episiotomy group. No fourth grade tears appeared in any group.
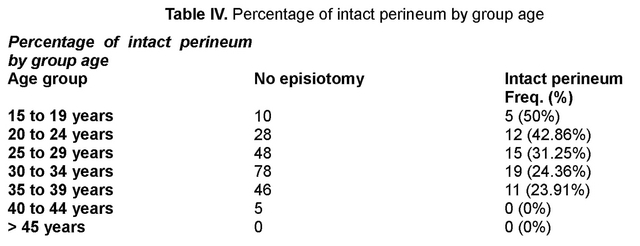
-The percentage of intact perineum's (no tears or episiotomy) was 28.7%. They were more frequent among the youngest women (15-19 years), with a rate of 50%, decreasing as the age increased.
Discusion
After the publication of a research showing a decrease of the episiotomy rates over 24.7%, a selective episiotomy policy was implanted at the HUMS in 2005. Therefore, an episiotomy rate of 59% in nulliparous women(9) was achieved. This particular data is similar to the one obtained in our research (62%), although is still higher than the recommended by The Strategy for Childbirth proposed by the Spanish Ministry of Health and Consumption (Estrategia de Atención al Parto Normal del Ministerio de Sanidad y Consumo)(14).
This research claims the fetal weight to be the main factor influencing the performance of episiotomy. Actually, it is observed that the average weight of the babies delivered by mothers who had episiotomy done was 122.7g heavier than in mothers who had not (3284.7g vs. 3162g), being statistically significant the rise of fetal weight with the realization of episiotomy. These results coincide with those obtained by Juste-Pina A. et al.(9), Okeke TC, et al.(19), Gossett DR, et al.(20), Wu LC, et al.(21) y Koskas M, et al.(22), relating fetal weight and episiotomy increase. However, other studies, such as Molina-Reyes. C, et al.(7), Carvalho CC, et al.(10), Herrera B, et al.(11). Figueira L, et al.(12), y Trinh AT, et al.(23) did not found statistically significant relation between the newborn weight and the performance of episiotomy.
Individual criteria seem to be another factor influencing the performance of episiotomy. Episiotomy rates vary from 75% to 16.7% among different professionals, what determines the non-existence of common criteria when performing the episiotomy. The said individual criteria was highlighted on Gossett dR, et al.(20) y Wu LC, et al.(24) research. However, in our study, every professional sample is quite low, so new research would be needed to confirm this conclusion.
No relation between the variables seems to exist when analyzing the professional category as factor influencing the realization of episiotomy. In spite of it, and based on episiotomy frequencies of each group, we could highlight a higher rate of episiotomy among the gynaecology residents (74.4%), compared to midwives (60.6%) and resident midwives (59.6%). This result coincides with the obtained by Robinson JN, et al.(25), who obtained rates slightly higher among the resident midwives (33.3%) than among the midwives (21.4%). The episiotomy rate among the gynaecologists was 50%, much lower than in the rest of categories. However, the number of deliveries assisted by this group is also lower, so it would be necessary to enlarge the sample to confirm the statement.
Concerning the relation between age and episiotomy, no statistically significant association was found between both variables, coinciding with the result obtained by Azón-López E, et al.(26). The consulted studies show different results, because some authors establish a relation between the increase of episiotomy rate and the age increase(7,21), while others show higher rates among the youngest groups(10,20,27,28), or women from 35 years old(10).
Analyzing nationality as a possible underlying factor for episiotomy, no association was found between both variables in our study. However, the number of women in some population groups is quite low, so new research would be needed to confirm this conclusion. Other consulted studies, such as Azón-López E, et al.(26), did not find any relation either, while others established a higher episiotomy rate among Indians(21), as well as Hispanics against Afro-Americans(28).
No statistically significant relation was found between the gestational age and the performance of episiotomy, result that coincides with the obtained by Herrera B, et al.(11).
Other variables, such as the use of analgesia during the delivery, did not present any association with the performance of episiotomy, mainly epidural analgesia and local analgesia. When revising the existent studies, contradictory results were found, above all, related to the epidural analgesia use. Authors such as Robinson JN, et al.(25) and Molina-Reyes C, et al.(7), found a relation between the use of analgesia and episiotomy, while others, such as Trinh AT, et al.(23), did not.
Concerning the fetal gender and the time of birth, no association was found between the variables and the performance of episiotomy. No research analyzing these variables has been found.
Concerning the question whether the performance or non performance of episiotomy may influence the neonatal results, determined b the umbilical artery pH, it was observed that the results were normal in both groups, so it does not influence the fetal well-being parameters. This result coincides with other studies consulted(29,30), even with those who value the Apgar test as a measure to determine fetal well-being(7,10,12,30,31). Therefore, the justification of the use of episiotomy to reduce fetal and neonatal morbility would not be supported.
Analyzing whether the performance or non performance of episiotomy influences perineal tears, our research determines that the no realization increases the percentage of first and second grade tears, mainly those of first grade. This data coincides with the biggest part of the revised studies(4,7,9,10,12,30-33). Besides, in our research, the non performance of episiotomy increased the percentage of more serious tears (third and fourth grade), coinciding with other consulted studies(30-34), although authors such as Zafran N, et al.(35), associate an increase of 0.8% on anal sphincter tears to the realization of restrictive episiotomy on primiparous women. Considering the episiotomy itself a second grade injury, we may say that its non performance will cause a higher risk of perineal injury, maximum a tear of the same grade, while an extremely high probability of a lower tears exists. This fact should be highly considered within the youngest women group, when the probability of keeping the perineum intact after the birth is higher.
A weakness of our study is the variable "perineal tear grade", which may cause a bias in the classification, because its assessment is carried out by each professional delivering the birth, and interpreting differences among each individual may exist. It would be important for future research to control the said bias by a previous training programme to unify the classification criteria or trusting a unique observer to determine this variable.
Conclusions
From the obtained results, it could be concluded that, in our study, the main factors that seem to influence the performance of episiotomy are the fetal weight and the individual criteria of each professional attending the delivery.
Other factors, such as the gestational age, fetus gender, and epidural analgesia, time of birth or nationality seem to have a scarce or even inexistent influence over the performance or non performance of the episiotomy.
In this particular study, it has been confirmed that the non performance of episiotomy increases first grade tears and, in a lower extent, the second grade ones, without endangering the fetal well-being. Besides, by avoiding the routine episiotomy, the possibilities of keeping the perineum intact after the delivery increase.
The episiotomy rate within the sample population reaches 62%, a higher percentage than the recommended by the Spanish Ministry of Health and Consumption (Ministerio de Sanidad y Consumo). Therefore, it would be advisable to revise the selective episiotomy policy at the hospital to reduce the said percentage and unify the criteria among the health professionals.
References
1. Carroli G, Belizán J. Episiotomía en el parto vaginal (Revisión Cochrane traducida). En: La Biblioteca Cochrane Plus, número 3, 2008. Oxford, Update Software Ltd. Disponible en: http://www.update-software.com (Traducida de The Cochrane Library, Issue. Chichester, UK: John Wiley & Sons, Ltd. [ Links ]).
2. Grupo de trabajo de la Guía de Práctica Clínica sobre Atención al Parto Normal. Guía de Práctica Clínica sobre la Atención al Parto Normal. Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad y Política Social. Agencia de Evaluación de Tecnologías Sanitarias del País Vasco (OSTEBA). Agencia de Evaluación de Tecnologías Sanitarias de Galicia (Avalia-t). 2010. Guías de Práctica Clínica en el SNS: OSTEBA No 2009/01. [ Links ]
3. Maceira Rozas MC, Salgado Barreira A, Atienza Merino G. La asistencia al parto de las mujeres sanas: estudio de variabilidad y revisión sistemática. Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad y Política Social. Axencia de Avaliación de Tecnoloxías Sanitarias de Galicia; 2007. Informes de Evaluación de Tecnologías Sanitarias: avalia-t. No. 2007/03. [ Links ]
4. Lai CY, Cheung HW, Hsi Lao TT, Lau TK, Leung TY. Is the policy of restrictive episiotomy generalisable? A prospective observational study. J Matern Fetal Neonatal Med. 2009 Dec; 22(12):1116-21. doi: 10.3109/14767050902994820. [ Links ]
5. Shahraki AD, Aram S, Pourkabirian S, Khodaee S, Choupannejad S. A comparison between early maternal and neonatal complications of restrictive episiotomy and routine episiotomy in primiparous vaginal delivery. J Res Med Sci. 2011 December; 16(12):1583-1589. Pubmed PMID:22973367. Pubmed PMCID:PMC3434900. [ Links ]
6. Carroli G, Mignini L. Episiotomía para el parto vaginal (Revisión Cochrane traducida). Cochrane Database of Systematic Reviews 2012 issue 11. Art. No.: CD000081. DOI: 10.1002./14651858.CD000081.pub2. Pubmed PMID:19160176. [ Links ]
7. Molina-Reyes C, Huete-Morales MD, Sánchez JC, Ortiz-Albarín MD, Jiménez I, Aguilera MA. Implantación de una política de episiotomía selectiva en el Hospital de Baza. Resultados materno-fetales. Prog Obstet Ginecol. 2011; 54(3):101-8.doi:10.1016/j.pog.2011.01.008. [ Links ]
8. Rodríguez A, Arenas EA, Osorio AL, Mendez O, Zuleta JJ. Selective vs routine midline episiotomy for the prevention of third- or fourth-degree lacerations in nulliparous women. Am J Obstet Gynecol. 2008 Mar;198(3):285.e1-4. doi:10.1016/j.ajog.2007.11.007. Epub 2008 Jan 25. [ Links ]
9. Juste-Pina A, Luque-Carro R, Sabater-Adán B, Sanz-de Miguel E, Viñerta-Serrano E, Cruz-Guerreiro E. Episiotomía selectiva frente a episiotomía rutinaria en nulíparas con parto vaginal realizado por matronas. Matronas Prof. 2007; 8 (3-4):5-11. [ Links ]
10. Carvalho CC, Souza AS, Moraes Filho OB. Prevalence and factors associated with practice of episiotomy at a maternity school in Recife, Pernambuco, Brazil. Rev Assoc Med Bras. 2010 May-Jun; 56(3):333-9. Pubmed PMID:20676543. [ Links ]
11. Herrera B, Gálvez A. Episiotomía selectiva: un cambio en la práctica basado en evidencias. Prog Obstet Ginecol. 2004; 47(9):414-22. [ Links ]
12. Figueira L, Ibarra M, Cortés R, Blasco M, Mendoza A, Velásquez G. Episiotomía selectiva versus rutinaria en pacientes nulíparas. Rev Obstet Ginecol Venez. 2004; 64(3):121-27. [ Links ]
13. Sistema Nacional de Salud. Ministerio de Sanidad y Consumo. Estrategia de Atención al parto normal (internet). Ministerio de Sanidad y Consumo;2007 (citado 3 deabrilde 2014. Disponible en: http://www.msc.es/organizacion/sns/planCalidadSNS/pdf/equidad/estrategiaPartoEnero2008.pdf. [ Links ]
14. Santos Redondo P, Al-Adib Mendiri M. Estrategia de Atención al Parto Normal en el Servicio Extremeño de Salud. Documento de adhesión a la EAPN del SNS y Protocolos de aplicación práctica (internet). Servicio Extremeño de Salud; 2013 (citado 3 de abril de 2014). Disponible en: http://saludextremadura.gobex.es/c/document library/getfile?uuid=932e46ac-63cb-49fe-9f23-e85c8d84e029&groupld=19231. [ Links ]
15. Graham ID, Carroli G, Davies C, Medves JM. Episiotomy rates around the world: an update. Birth. 2005; 32(3):219-23. Pubmed PMID:16128977. [ Links ]
16. Melchor JC, Bartha JL, Bellart J, Galindo A, Miño M, Perales A. La episiotomía en España. Datos del año 2006. Prog Obstet Ginecol. 2008;51(9):559-563. doi: 10.1016/S0304-5013(08)72329-X. [ Links ]
17. Reinbold D, Eboue C, Morello R, Lamendour N, Herlicoviez M, Dreyfus M. From the impact of French guidelines to reduce episiotomy's rate. J Gynecol Obstet Biol Reprod (Paris). 2012 Feb;41(1):62-8. doi:10.1016/j.jgyn.2011.08.006. Epub 2011 Oct 20. French. Pubmed PMID:22018442. [ Links ]
18. Andreani M, Locatelli A, Assi F, Consonni S, Malguzzi S, Paterlini G, et al. Predictors of umbilical artery acidosis in preterm delivery. Am J Obstet Gynecol. 2007;197(3):303.e1-5. Pubmed PMID:17826430. [ Links ]
19. Okeke TC, Uqwu EO, Okezie OA, Enwereji JO, Ezenyeaku CC, Ikeako LC. Trends and determinants of episiotomy at the University of Nigeria Teaching Hospital (Unth), Enugu, Nigeria. Niger J Med. 2012 Jul-Sep;21(3):304-7. Pubmed PMID:23304925. [ Links ]
20. Gossett DR, Dunsmoor Su RD. Episiotomy practice in a community hospital setting. J Reprod Med. 2008 Oct; 53:803-8. Pubmed PMID:19004409. [ Links ]
21. Wu LC, Malhotra R, Allen JC Jr, Lie D, Tan TC, Ostbye T. Risk factors and midwife-reported reasons for episiotomy in women undergoing normal vaginal delivery. Arch Gynecol Obstet. 2013 Dic; 288(6):1249-56. doi:10.1007/s00404-013-2897-6. Epub 2013 May 26. Pubmed PMID:23708390. [ Links ]
22. Koskas M, Caillod AL, Fauconnier A, Bader T. Maternal and neonatal consequences induced by the French recommendations for episiotomy practice. Monocentric study by 5409 vaginal deliveries. Gynecol Obstet Fertil. 2009 Sep;37(9):697-702. doi:10.1016/j.gyobfe.2009.06.003. Epub 2009 Aug 13. French. Pub PMID:19682940. [ Links ]
23. Trinh AT, Khambalia A, Ampt A, Morris JM, Roberts CL. Episiotomy rate in Vietnamese-born women in Australia: support for a change in obstetric practice in Vietnam. Bull World Health Organ. 2013 May 1;91(5):350-6. doi:10.2471/BLT.12.114314. Epub 2013 Mar 21. Pubmed PMID:23678198. Pubmed PMCID:PMC3646354. [ Links ]
24. Wu LC, Lie D, Malhotra R, Allen JC Jr, Tay JS, Tan TC, et al. What factors influence midwives' decision to perform or avoid episiotomies? A focus group study. Midwifery. 2013 Aug;29(8):943-9.doi:10.1016/j.midw.2012.11.017. Epub 2013 Feb 28. Pubmed PMID:23453700. [ Links ]
25. Robinson JN, Norwitz ER, Cohen AP, Lieberman E. Predictors of episitomy use at first spontaneous vaginal delivery. Obstet Gynecol. 2000; 96(2):214-18. Pubmed PMID:10908765. [ Links ]
26. Azón-Lopez E, García-Martínez M, Subirón-Valera AB. Análisis de los resultados obstétricos y neonatales de los partos inducidos en nulíparas en el Hospital Clínico de Zaragoza. Matronas Prof. 2013;14(2):52-59. [ Links ]
27. Da Silva FM, de Oliveira SM, Bick D, Osava RH, Tuesta EF, Riesco ML. Risk factors for birth-related perineal trauma: a cross-sectional study in a birth centre. J Clin Nurs. 2012 Aug; 21(15-16):2209-18. doi:10.1111/j.1365-2702.2012.04133.x. Epub 2012 May 31. Pubmed PMID:22646921. [ Links ]
28. Ogunyemi D, Manigat B, Marquis J, Bazargan M. Demographic variations and clinical associations of episiotomy and severe perineal lacerations in vaginal delivery. J Natl Med Assoc. 2006 Nov; 98 (11):1874-1881. Pubmed PMID:17128701. Pubmed PMCID:PMC2569796. [ Links ]
29. Dannecker C, Hillemanns P, Strauss A, Hasbargen U, Hepp H, Anthuber C. Episiotomy and perineal tears presumed to be inminent: randomized controlled trial. Acta Obstet Gynecol Scand. 2004 Apr; 83(4):364-8. Pubmed PMID:15005784. [ Links ]
30. Cabrera-Guerra Y, Pascual-Pedreño A, Hernández-Martínez A, Mayorga-Campo M, Martínez-Bermejo MT, Bueno-Pacheco G. Evaluación y eficacia de las medidas preventivas en la anemia intraparto. Rev Calid Asist. 2010;25(4):193-199. doi:10.1016/j.cali.2009.12.002.Epub 2010 Jan 27. Pubmed PMID:20106693. [ Links ]
31. Ràisànen S, Vehvilàinen-Julkunen K, Heinonen S. Need for and consequences of episiotomy in vaginal birth: a critical approach. Midwifery. 2010 Jun; 26(3):348-56. doi:10.1016/j.midw.2008.07.007. Epub 2008 Sep 18. Pubmed PMID:18804317. [ Links ]
32. Pérez Valero S. Episiotomía en partos vaginales eutócicos en el Hospital Universitario "La Ribera". NURE Inv (Internet). 2013 mar-abr (citado 2 abril 2014);10(63):(aprox.6p.). Disponible en: http://www.fuden.es/FICHEROSADMINISTRADOR/ORIGINAL/NURE63originalepisiotomia.pdf. [ Links ]
33. Chehab M, Courjon M, Eckman-Lacroix A, Ramanah R, Maillet R, Riethmuller D. Impact of a major decrease in the use of episiotomy on perineal tears in a level III maternity ward. J Gynecol Obstet Biol Reprod (Paris). 2013 Jul 29. pii:S0368-2315(13)00153-1. doi: 10.1016/j.gyn.2013.06.002.(Epub ahead of print). Pubmed PMID:23906972. [ Links ]
34. Eckman A, Ramanah R, Gannard E, Clement MC, Collet G, Courtois L, et al. Evaluating a policy of restrictive episiotomy before and after practice guidelines by the French College of Obstetricians and Gynecologist. J Gynecol Obstet Biol Reprod (Paris).2010 Feb;39(1):37-42. doi:10.1016/j.jgyn.2009.09.013. Epub 2009 Nov 4. French. Pubmed PMID:19892475. [ Links ]
35. Zafran N, Salim R. Impact of liberal use of mediolateral episiotomy on the incidence of obstetric anal sphincter tear. Arch Gynecol Obstet. 2012 Sep;286(3):591-7.doi:10.1007/s00404-012-2333-3.Epub 2012 May 1. Pubmed PMID:22546947. [ Links ]











 texto en
texto en 


