Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.17 no.51 Murcia jul. 2018 Epub 01-Jul-2018
https://dx.doi.org/10.6018/eglobal.17.3.295821
Originals
Detection, surveillance, and monitoring of multiresistant germs, in the sanitary areas III-IV of Cantabria (2013-2016)
1 Enfermeros del Servicio de Medicina Preventiva, Calidad y Seguridad del Paciente del Hospital Sierrallana de Torrelavega (Cantabria).España dulio@eresmas.com
In the European Union, according to the Center for Disease Control, die approximately 250,000 individuals per year because of the multidrug resistant bacteria to antibiotics, with an additional cost of €1,500 million to health systems. The World Health Organization has defined as " the great threat to the public health" and predicts that could cause 10 million deaths in the year 2050.
The present prospective study about the incidence of patients carriers of germs multiresistant to antibiotics (GMA), has been done from 2013 to June 2016 in the sanitary areas III-IV of Cantabria; with an estimated population of 200,000 inhabitants, distributed in two local hospitals (Hospital Sierrallana Torrelavega, Hospital of Three Seas Reinosa), 14 health centers and social health centers.
The process was applied monitoring, control and epidemiological monitoring, made from the Preventive Medicine Service Quality and safety of the patient with the collaboration of the Service of Microbiology and Primary Care.
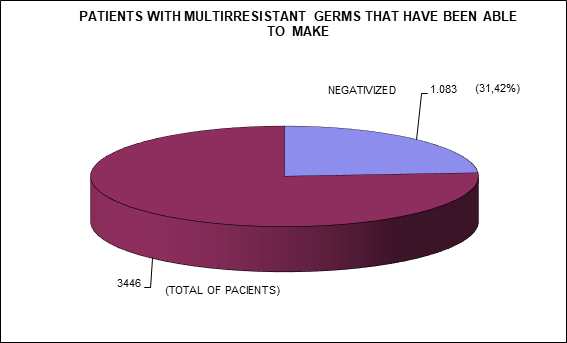
Of a total of total of 3446 patients with germs with GMA, have been negativizar 1083 patients, which represents the 31,42% of the total.
Taking into account that each of these patients remain admitted an average stay of 5 days more than those who do not have these multirresistencias to antibiotics. Has been achieved that these patients once negatives could enter without being isolated and what this presents at the level of health, economic and psychologically; as well as to improve the sanitary resources.
Keywords: Risk factor; Cross infection; Bacterial drug resistance
INTRODUCTION
The emergence of GMA, is a serious threat to global public health. The development of these resistors is a natural biological phenomenon that is widening year after year 1
Among the factors related with infections/colonizations by GMA, we describe: the prolonged hospitalization, chronic diseases, surgical interventions, the stay in the ICU, the insertion of invasive devices, the breach of the rules of isolation and biosecurity measures and the inappropriate use of antibiotics 2
When a patient has an infection/colonization by a GMA, the prognosis is worse, since the same is associated with increased morbidity and mortality and the cost of the treatment. A GMA is characterized by resistance to three or more groups of antibiotics commonly used in the treatment of infections and that this resistance has a clinical relevance.
In the year 2009, the European Center for Disease Prevention and Control (ECDC) estimated that in the EU approximately 400,000 patients/year suffer an infection caused by one of the five multidrug resistant bacteria more common, and about 25,000 patients/year die as a result of an infection caused by this group of microorganisms 3
In addition, the costs they generate (health and loss of productivity) are close to 1,500 million €/year. Similar figures are described in the US where, each year, at least 2 million people acquire serious infections caused by GMA 4
The epidemiologic surveillance, the outreach and information to professionals and the family, the implementation of solutions alcoholic for the hygiene of the hands and the insulation at the hospital level of the patients carriers of germs multiresistant, have a proven efficacy in reducing these germs and in turn in the negativization of infected patients and/or colonized with considerable savings in expenditure on health and at the level of sociolabour 5
MATERIAL AND METHODS
We performed a prospective descriptive observational study of the incidence of the patients carriers of GMA.
The period of duration, has been the period between 1 January 2013 to 30 June 2016.The population object of study has been attended to in the sanitary areas III-IV of Cantabria. According to the estimates of the municipal registers amounts to 200,000 inhabitants, distributed in two local hospitals: Hospital Sierrallana (Torrelavega), Hospital of Three Seas (Reinosa)), 14 Health Centers and Social Health Centers. The process was applied monitoring, control and epidemiological monitoring, made from the Preventive Medicine Service Quality and safety of the patient with the collaboration of the Service of Microbiology and Primary Care.
The data on GMA, have been obtained from: the database in the computer application DIAS, which contains all of the patients the historical and current carriers of infections by GMA, of the discharge reports for the medical-surgical services and by the flyers of the results of the Laboratory of Microbiology.
Once detected patients with GMA, are entered in the database days; if you require hospital admission is applied to the contact isolation in your room to prevent the spread to other patients, informing the professionals who attend to you to implement the protocol of GMA and follow the measures of standard precautions appropriate to adopt (hand hygiene, gloves and Bata). At home it is not necessary to apply measures of isolation, because in your environment do not usually tend to live together with people who suffer from immunosuppression or do not have immune mechanisms of defense against the aforementioned germs.
During your stay in the hospital, you are series of crops of smear every seven days, if they are positive and from three series in that same income, will not be repeated (except that remain entered more than a month since the last collection of smears); but will remain the insulation until the high. If the number is negative are repeated without waiting for the time of one week between each series. To get three series negative is removed from the positive in the database days and removed the insulation.
If you have a partner at the time of detection of GMA, pulls out of the room but does not apply insulation whatsoever; but he performs a series crops of smear for the same isolated germ in your partner.
If a negative behavior is not nothing more; but if the outcome of the series of crops is positive, it performs the insulation and monitoring as her former colleague.
You do not need to the three series of smears of crops are made necessarily during the same hospital admission, since this can be short and not to give time to complete the study. In this case, will be tracked from Primary Care or in successive revenue if any.
If the next entry takes place more than a year since the previous, will have a single series of smears of crops of germ; and if the result is negative you are removed from the positive in the database days.
In Attention Primacy, also skips the alarm in the computer program, IMO-AP; each time that the patient go to the Health Center.
In the EMC environment does not lack collect the smears every seven days; but that if the results obtained are positive are spaced over a period of a month between a smear and another. It is also removed from the basis of the positive patients when obtained three series negative. When the GMA is more than one year since its detection without income or samples of follow-up of their infection/colonization, pulls out of the database days to obtain a single sample with a result of microbiological negative.
Each time that the patient go to the Hospital, in the label of the demographics staff jumps a code ERUDINET and the GMA, with which to specify income hospìtalario, will isolated.
Every day at first hour of the morning, accesses the database DIAS, that crosses the information with the list of patients admitted and provides us with the relationship of users with GMA in the hospital; subsequently leads to each floor of hospitalization follow-up sheet individualized for each professional, both medical and nursing. Likewise, the ship via fax to the health centers of the information to the health personnel responsible for the patients carriers of the GMA and the collection if it originates from the series of smear needed to perform a proper monitoring of the state of infection /colonization of the patient, with the ultimate objective of descolonizarlo and pass it on to state of negative.
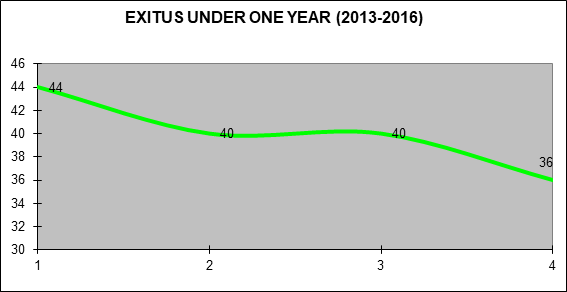
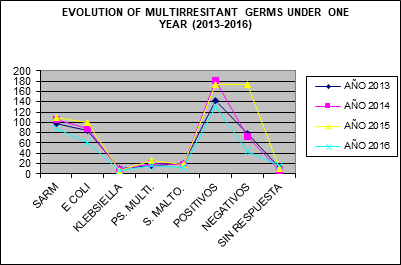
In the group of patients with GMA under 1 year of age and who were not negatives, have died 160 ( 13.74%). (Fig.2)
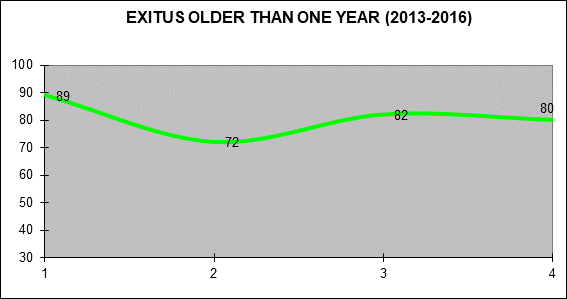
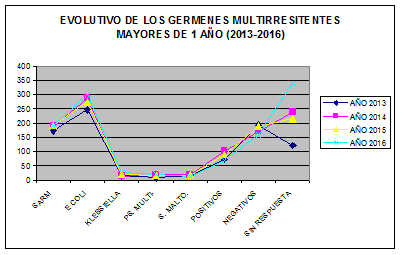
In the other group of patients with GMA older than 1 year and that were not negatives, has died 323 (14,15%). (Fig. 3)
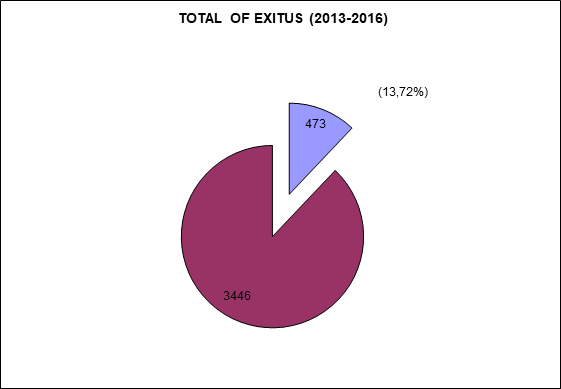
Of all the patients contained in the two groups, have died without being negatives 473 which is the 13.72% of the total. (Fig. 4)
We emphasize that the patients who died had pluripatologías concomitant that favored the morbidity and mortality, and that the fact of being infected and/or colonized worsened the clinical prognosis; although the death has not been due to the single cause of being a carrier of a GMA.
In the group of patients under the age of 1 year since its detection, and that we have not had a response 65 (5.58%)
In the other group, patients older than 1 year since its detection, and that we have not had a response 615 (26,95%).
The total of patients of the groups and that we have not received a response, have been 680 which represents the 19,73%.
In response to the designation of GMA and doing the division among children under 1 year of age and older than 1 year, we have the following results:
In the group of children under one year of age, we have detected 403 Stafilococcus aureus meticilinresistente (MRSA) and 332 Eschericha coli beta lactamase of expectro extended (E coli BLEE) of a total of 917 GMA; which means the 43,94% and 36,20% respectively. (Fig. 5)
In the group of more than a year, we have detected 745 SARM and 1109 E coli ESBL out of a total of 2058 GMA; which means the 36,20% and 53,88% respectively. (Fig. 6)
In the total of the two study groups, we have detected 1148 SARM and 1441 E coli ESBL out of a total of 2975 GMA; representing 38.58% and 48,43% respectively. Now, if we gather the MRSA and E coli BLEE, we obtain the 87.02% of the total of GMA.
The most frequent locations of these two GMA majority during this period have been found in PU (pressure ulcers) and in soft tissues for MRSA, and urinary tract and surgical wounds for E coli BLEE, respectively.
The Stay measured of the admitted patients carriers of GMA is 5 more days long, compared to those who enter and are not infected and/or colonized by these germs multiresistant.
DISCUSSION
Given the complexity of the problem of the GMA and the implementation of policies for the rational use requires a multidisciplinary approach 6)(7)(8
The implementation of the programs for the prevention and control of the GMA and more specifically the epidemiological surveillance, is the most effective tool to improve the quality of health services and represents a significant reduction in the rates of infection related with health care; decreasing the cost of health care of the patients.
Called substantially the attention in the present study; that in the group of GMA in patients older than 1 year since its detection, we have not had a response by the health professionals in 26,95% compared to 5.58% enel another group of patients under the age of 1 year.
This is due in part to the lack of involvement and awareness of the same; since i more time passes the patient being the bearer of GMA monitoring decreasing. And also that during this period there has been a process of transfers of doctors and nurses who have specified a period of time to adapt, understand and implement measures for the prevention, control, monitoring and epidemiological surveillance in front of the GMA.
The monitoring and control of the GMA, applying the existing protocols Insulation of contact with the measures of prevention Universal, have allowed 1083 patients to benefit that their infections and/or colonization were cured of GMA and what it represents for him and his family the working hours lost, the discomfort and which pose to the health who attend to you in the insulation hospitable.
Bearing in mind that each of the users carriers of GMA remain admitted an average of 5 days more in a room without being able to use the bed of the partner by the hospital center; and the increase in the pressure of care that this involves. 9)(10
In addition knowing that the DRG (Diagnostic Related Group) is similar to a pneumonia simple & pleuritis age > 17 years without complications, and has a cost of billing for the Service Cantabrian Health, 1.737,88 € per process.
It can be estimated that during the period of the present study, which runs from 1 January 2013 to 30 June 2016; from the Preventive Medicine Service Quality and safety of patient with implementation of the preventive measures mentioned above, there has been a saving theorist of 1.882.124,04 €, resulting in improved efficiency in the management and in the level of quality of the health care provided.
It should be noted the hygiene of the hands of the health professionals and the most effective measure to decrease the spread of the GMA in infections related to health care; secondly, the monitoring and control in the application of the measures of isolation and epidemiological surveillance.
The risk factors that are associated with resistance to antibiotics are: 12
● gravity of the patient.
● underlying disease.
● degree of immunity.
● indiscriminate use of antibiotics
The application of the epidemiological surveillance and control of the GMA does not have as its purpose the economic savings, but the prevention of infections and improve the quality of life in the health of patients. In order to increase these objectives must be to focus primarily on the following measures: 13
REFERENCIAS
1. Organización Mundial de la Salud. Ginebra, Suiza; 2003 (acceso: 29.11.2013). Prevención de las infecciones nosocomiales. Guía Práctica. 2ª Edición. Disponible en: http://www.who.int/csr/resources/publications/ES_WHO_CDS_CSR_EPH_2002_12.pdf. [ Links ]
2. Sociedad Española de Medicina Intensiva Crítica y Unidades Coronarias(SEMICYUC), Grupò de trabajo de Enfermedades Infecciosas. Estudio Nacional de Vigilancia de la Infección Nosocomial en Servicio de medicina Intensiva. ENVIN_HELICS. Informe 2012. Disponible en :http://hws.vhebron.net/nvin-helics/. [ Links ]
3. European Center for Disease Prevention and Control and the European Medicines Agency. ECDC/EMEA Joint technical Report. The Bacterial Challenge: Time to React. 2009. http://www.ecdc.eruopa.eu/en/publications/ Publications/0909_TER_The_Bacterial_Challende_Time_to_React.pdf (11 August 2013, date last accessed). [ Links ]
4. Jane D. Siegel, MD, Emily Rhinehart, RN, MPH, CIC, Marguerite Jackson, PhD, Linda Chiarello, RN, MS, and the Healthcare Infection Control Practices Advisory Committee Dallas, Texas; San Diego, California; and Atlanta, Georgia. Management of multidrug-resistant organisms in health care settings, 2006. Am J Infect Control 2007; 35:S165-S193. [ Links ]
5. Rodriguez Camacho E, Diaz Garcia B. Infecciones/colonizaciones por Gérmenes Multirresistentes. Galicia Clin 2014; 75 (1) 17-21. [ Links ]
6. Freixas N, Sallés M, Garcia L. Cambios en el control de la infección nosocomial: nuevos retos y competencias de la enfermera de control de infección. Enfermedades Infecciosas y Microbiología Clínica. Volume 27, Issue 5, May 2009, Pages 285-289. [ Links ]
7. Rodríguez-Baño J. Bischofberger C, Álvarez-Lerma F, Asensio A, Delgato T, et al. Vigilancia y control de Staphylococcus aureus resistente a meticilina en hospitales españoles. Documento de consenso GEIH_SEIMC y SEMPSPH. Enfermedades Infecciosas y Microbiología Clínica. Volume 26, Issue 5, May 2008, Pages 285-298. [ Links ]
8. Cantón R, Morosini M.I. Microorganismos multirresistentes en los hospitales: un riesgo amenazante. GH Continuada. Septiembre-Octubre 2010. Vol.9 Nº5. pag 254-257. [ Links ]
9. Scanvic A, DenicL, Gaillon S, Giry P, Adremont A, Lucet JC, Duration of colonizacion by methicillin-resistant Staphylococcus auresus after hospital discharge and risk factors for prolonged carriage. Clinical infectius diseases: an official publication of the infectious Siseases Society of America. 2001; 32(10): 1398-8 Epub 2001/004/24. [ Links ]
10. Weintrob AC, Roediger MP, Barber M, Summers A, Fieberg AM, Dunn J, et al. Natural history of colonization with gram-negative multidrug-resitant organisms among hospitalized patients. Infection control and hospital epidemiology. 2010;31(4):330-7. Epub 2010/02/24. [ Links ]
11. Orden SAN/12/2011, DE 20 DE Abril, por las que se fijan las cuantías de los precios públicos de los Servicios Sanitarios prestados en el Servicio Cántabro de Salud. Publicado en el BOC número 85, de jueves 25 de Mayo de 2011. [ Links ]
12. Alvarez Lema F. Impacto de las resistencias bacterianas sobre la política de antibiótica. Med Intensiva. 1998; 22: 17-23. [ Links ]
13. Lieborwitz LD. MRSA burden and intervention. Int J Antimicrob Agents. 2009;34 Suppl 3:S11-3. [ Links ]
Received: May 31, 2017; Accepted: September 10, 2017











 texto en
texto en